Quest for the right Drug
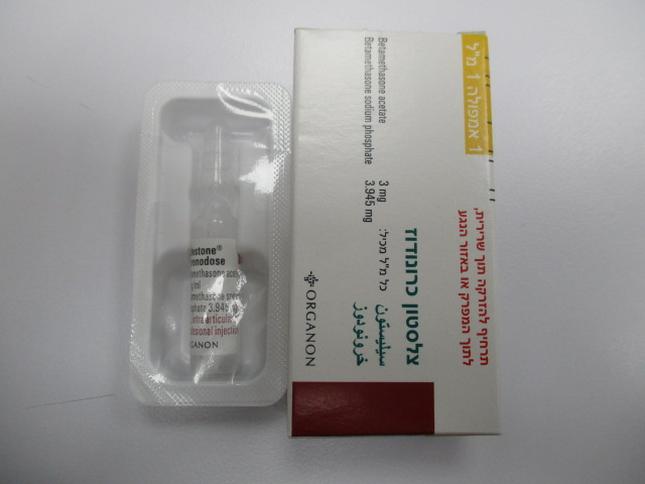
צלסטון כרונודוז CELESTONE CHRONODOSE (BETAMETHASONE ACETATE, BETAMETHASONE SODIUM PHOSPHATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-שרירי, תוך מפרקי, לתוך פצע : I.M, INTRA-ARTICULAR, INTRA-LESIONAL
צורת מינון:
תרחיף להזרקה : SUSPENSION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Celestone Chronodose cannot be used for intravenous or subcutaneous administration. Serious neurologic events, some resulting in death, have been reported with epidural injection of corticosteroids. Specific events reported include, but are not limited to, spinal cord infarction, paraplegia, quadriplegia, cortical blindness, and stroke. These serious neurologic events have been reported with and without use of fluoroscopy. The safety and effectiveness of epidural administration of corticosteroids have not been established, and corticosteroids are not approved for this use. Pheochromocytoma crisis, which can be fatal, has been reported after administration of systemic corticosteroids. Corticosteroids should only be administered to patients with suspected or identified pheochromocytoma after an appropriate risk/benefit evaluation. ANTISEPTIC TECHNIQUES ARE NECESSARY. Celestone Chronodose contains two betamethasone esters, one of which, betamethasone sodium phosphate, disappears rapidly from the injection site. Therefore, when using this product, the physician must take into account that this soluble portion of Celestone Chronodose may have a systemic effect. Corticosteroids are not indicated to treat hyaline membranes after birth. For the prophylactic treatment of hyaline membrane disease in premature infants, do not administer corticosteroids to pregnant women with pre-eclampsia or eclampsia or with signs of placental lesions. Intramuscular injection of corticosteroids should be performed deep in large muscle masses to avoid local tissue atrophy. Celestone Chronodose intramuscular injection should be administered with caution in patients with idiopathic thrombocytopenic purpura. The injection of corticosteroids in soft tissue, and their intralesional or intra-articular injection may induce systemic as well as local effects. It is essential to examine any liquid that may be present in the joint, in order to exclude a septic process. Avoid local injection into a previously infected joint. A net increase in pain and local swelling, further decrease in joint mobility, fever and malaise should raise the question of septic arthritis. If the diagnosis of infection is confirmed, appropriate antimicrobial treatment must be initiated. Do not inject corticosteroids in unstable joints, infected areas or intervertebral spaces. Repeated injections into osteoarthritis-affected joints can aggravate the destruction of the joint. Avoid injecting corticosteroids directly into tendons because tendon ruptures have been seen to occur subsequently. Rare instances of anaphylactoid/anaphylactic reactions with a possibility of shock have occurred in patients receiving parenteral corticosteroid therapy. Appropriate precautionary measures should be taken with patients who have a history of allergic reactions to corticosteroids. During prolonged corticosteroid therapy, consider switching from parenteral to oral administration after weighing the potential benefits and risks. Glucocorticoids may mask certain signs of infection, and new infections may appear during their use. A decrease in resistance and difficulty in localizing the infection can be observed when using glucocorticoids. Prolonged use can lead to posterior subcapsular cataract (especially in children) or to glaucoma, which can damage the optic nerves, and may exacerbate secondary ocular infections due to fungi or viruses. In case of prolonged treatment (over 6 weeks), it is necessary to have regular ophthalmological examinations. Average and large doses of corticosteroids can induce hypertension, fluid retention and increased potassium excretion. A low sodium diet and potassium supplements may be considered. All corticosteroids increase calcium excretion. PATIENTS ON CORTICOTHERAPY CANNOT RECEIVE THE FOLLOWING TYPES OF TREATMENT: - SMALLPOX VACCINATION; - OTHER METHODS OF IMMUNIZATION (ESPECIALLY AT HIGH DOSE) BECAUSE OF THE RISK OF NEUROLOGICAL COMPLICATIONS AND INADEQUATE ANTIBODY RESPONSE. However, patients receiving corticosteroids as replacement therapy, may be immunized (e.g., Addison's disease). Patients, especially children, receiving immunosuppressive doses of corticosteroids should be warned to avoid exposure to chickenpox or measles. In the case of active tuberculosis, corticosteroids should be limited to cases of fulminating or disseminated tuberculosis, where corticosteroids are used in combination with a suitable anti-tubercular treatment regimen. If corticosteroids are indicated in patients with latent tuberculosis or reacting to tuberculin, strict monitoring is necessary, because it can produce a reactivation of the disease. During prolonged corticosteroid therapy, patients should receive chemoprophylaxis. If using rifampicin in a chemoprophylaxis program, its enhancing effect on the metabolic hepatic clearance of corticosteroids must be remembered; it may be necessary to adjust the dose of the corticosteroid. Secondary adrenocortical insufficiency induced by the medicinal product can be minimized by gradual reduction of the dosage. This relative insufficiency may last for several months after discontinuation of therapy; if a state of stress is observed during this period, a new hormonal treatment must be initiated. Since mineralocorticoid secretion may be impaired, it is necessary to provide simultaneous administration of a mineralocorticoid and/or salt. Glucocorticoids exert a greater effect in hypothyroidism or cirrhosis. Given the risk of corneal perforation, glucocorticoids should be administered with caution in patients with ocular herpes simplex. Emotional instability and existing psychotic tendencies may be aggravated by corticosteroids. Caution is advised in: Nonspecific ulcerative colitis - Impending perforation of abscesses and other pyogenic infections - Diverticulitis - Intestinal anastomosis - Gastro-duodenal ulcer - Renal insufficiency - Hypertension - Osteoporosis - Myasthenia gravis. As corticosteroids can disrupt the growth of infants and children and inhibit the endogenous production of corticosteroids, it is important to monitor their growth and development carefully during prolonged treatment. Corticosteroids can sometimes alter the motility and number of spermatozoa in some patients. Cases of tendon rupture have been reported when corticosteroids and fluoroquinolones are administered separately. Therefore, simultaneous administration may increase the risk. Special monitoring of the patient is required in the following situations: tuberculosis, ocular herpes simplex, glaucoma, acute psychosis, active or latent gastric ulcer, Cushing's syndrome, renal insufficiency, hypertension, osteoporosis, diabetes, psychotic tendencies, viral and bacterial infections, heart failure, difficult-to-treat epilepsy, growth failure, diverticulitis, recent intestinal anastomoses, thromboembolism or thrombophlebitis tendencies, myasthenia gravis, pregnancy. Visual disturbance Visual disturbance may be reported with systemic and topical (including, intranasal, inhaled and intraocular) corticosteroid use. If a patient presents with symptoms such as blurred vision or other visual disturbances, the patient should be considered for referral to an ophthalmologist for evaluation of possible causes of visual disturbances which may include cataract, glaucoma or rare diseases such as central serous chorioretinopathy (CSCR) which have been reported after use of systemic and topical corticosteroids. Results from a single, multicenter, randomized, controlled study with another corticosteroid, methylprednisolone hemisuccinate, showed an increase of early mortality (at 2 weeks) and late mortality (at 6 months) in patients with cranial trauma who had received methylprednisolone, compared to placebo. The causes of mortality in the methylprednisolone group have not been established. Sodium This medicine contains less than 1 mmol sodium (23 mg) per ml, that is to say essentially ‘sodium-free’. Benzalkonium chloride Celestone Chronodose contains benzalkonium chloride, which can cause irritation and skin reactions. This medicine contains 0.2 mg benzalkonium chloride in each 1 ml ampoule which is equivalent to 0.2 mg/ml.
Effects on Driving
4.7 Effects on ability to drive and use machines Although vision problems are rare side effects, patients who drive vehicles or machinery must be informed of that.

שימוש לפי פנקס קופ''ח כללית 1994
Rheumatoid arthritis, osteoarthritis, other arthritic conditions by intra-articular injection, inflammatory, allergic & rheumatic conditions requiring a glucocorticoid effect, in patients for whom treatment with oral corticosteroid is not feasible. יירשם ע"י רופא אורטופד
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
