Quest for the right Drug
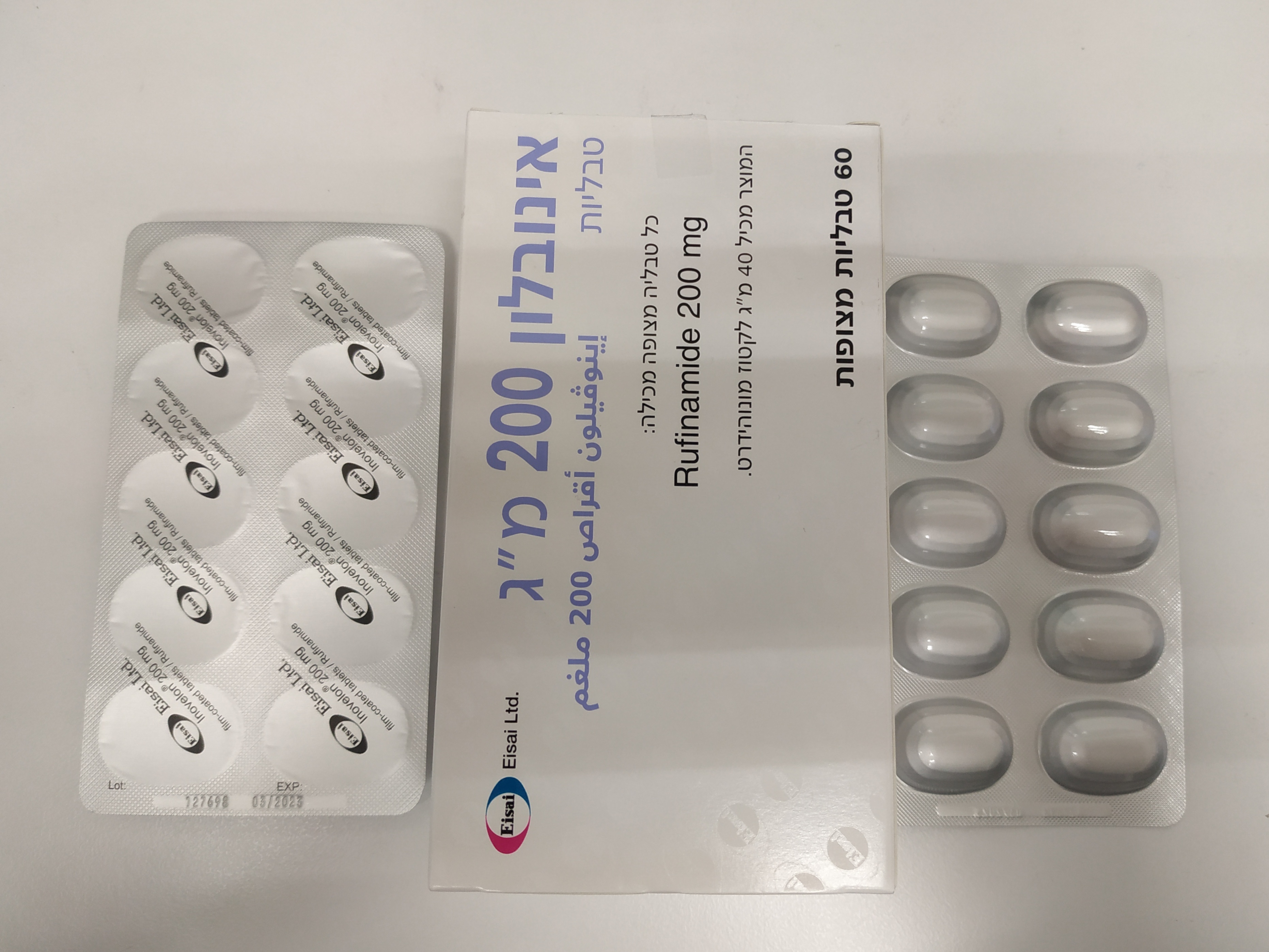
אינובלון טבליות 200 מ"ג INOVELON 200 MG TABLETS (RUFINAMIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: anti-epileptics, carboxamide derivatives; ATC-code: N03AF03. Mechanism of action Rufinamide modulates the activity of sodium channels, prolonging their inactive state. Rufinamide is active in a range of animal models of epilepsy. Clinical experience Inovelon tablets was administered in a double blind, placebo-controlled study, at doses of up to 45 mg/kg/day for 84 days, to 139 patients with inadequately controlled seizures associated with Lennox-Gastaut Syndrome (including both atypical absence seizures and drop attacks). Male and female patients (between 4 and 30 years of age) were eligible if they had a history of multiple seizure types, which had to include atypical absence seizures and drop attacks (i.e., tonic–atonic or astatic seizures); were being treated with 1 to 3 concomitant fixed-dose antiepileptic medicinal products; a minimum of 90 seizures in the month before the 28-day baseline period; an EEG within 6 months of study entry demonstrating a pattern of slow spike-and-wave complexes (2.5 Hz); a weight of at least 18 kg; and a CT scan or MRI study confirming the absence of a progressive lesion. All seizures were classified according to the International League Against Epilepsy Revised Classification of Seizures. As it is difficult for caregivers to precisely separate tonic and atonic seizures, the international expert panel of child neurologists agreed to group these seizure types and call them tonic–atonic seizures or “drop attacks”. As such, drop attacks were used as one of the primary end points. A significant improvement was observed for all three primary variables: the percentage change in total seizure frequency per 28 days during the maintenance phase relative to baseline (-35.8% on Inovelon tablets vs. –1.6% on placebo, p= 0.0006), the number of tonic-atonic seizures (- 42.9% on Inovelon tablets vs. 2.2% on placebo, p = 0.0002), and the seizure severity rating from the Global Evaluation performed by the parent/guardian at the end of the double-blind phase (much or very much improved in 32.2% on Inovelon tablets vs. 14.5% on the placebo arm, p=0.0041). Additionally, Inovelon tablets (rufinamide oral suspension) was administered in a multicentre, open-label study comparing the addition of rufinamide to the addition of any other AED of the investigator’s choice to the existing regimen of 1 to 3 AEDs in paediatric patients, 1 to less than 4 years of age with inadequately controlled LGS. In this study, 25 patients were exposed to rufinamide as adjunctive therapy for 24 weeks at a dose of up to 45 mg/kg/day, in 2 divided doses. A total of 12 patients received any other AED at the investigator’s discretion in the control arm. The study was mainly designed for safety and not adequately powered to show a difference with regards to the seizure efficacy variables. The adverse event profile was similar to that in children 4 years of age and older, adolescents, and adults. In addition, the study investigated the cognitive development, behaviour and language development of subjects treated with rufinamide compared to subjects receiving any-other-AED. The Least Square mean change of the Child Behaviour Checklist (CBCL) Total Problems score after 2 years of treatment were 53.75 for the any other AED group and 56.35 for the rufinamide group (LS mean difference [95% CI] +2.60 [-10.5,15.7]; p=0.6928), and the difference between treatments was -2.776 (95% CI: -13.3, 7.8, p=0.5939). Population pharmacokinetic/pharmacodynamic modelling demonstrated that the reduction of total and tonic-atonic seizure frequencies, the improvement of the global evaluation of seizure severity and the increase in probability of reduction of seizure frequency were dependent on rufinamide concentrations.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption Maximum plasma levels are reached approximately 6 hours after administration. Peak concentration (Cmax) and plasma AUC of rufinamide increase less than proportionally with doses in both fasted and fed healthy subjects and in patients, probably due to dose-limited absorption behaviour. After single doses food increases the bioavailability (AUC) of rufinamide by approximately 34% and the peak plasma concentration by 56%. Distribution In in-vitro studies, only a small fraction of rufinamide (34%) was bound to human serum proteins with albumin accounting for approximately 80% of this binding. This indicates minimal risk of drug-drug interactions by displacement from binding sites during concomitant administration of other substances. Rufinamide was evenly distributed between erythrocytes and plasma. Biotransformation Rufinamide is almost exclusively eliminated by metabolism. The main pathway of metabolism is hydrolysis of the carboxylamide group to the pharmacologically inactive acid derivative CGP 47292. Cytochrome P450-mediated metabolism is very minor. The formation of small amounts of glutathione conjugates cannot be completely excluded. Rufinamide has demonstrated little or no significant capacity in-vitro to act as a competitive or mechanism-based inhibitor of the following human P450 enzymes: CYP1A2, CYP2A6, CYP2C9, CYP2C19, CYP2D6, CYP2E1, CYP3A4/5 or CYP4A9/11-2. Elimination The plasma elimination half-life is approximately 6-10 hours in healthy subjects and patients with epilepsy. When given twice daily at 12-hourly intervals, rufinamide accumulates to the extent predicted by its terminal half-life, indicating that the pharmacokinetics of rufinamide are time-independent (i.e. no autoinduction of metabolism). In a radiotracer study in three healthy volunteers, the parent compound (rufinamide) was the main radioactive component in plasma, representing about 80% of the total radioactivity, and the metabolite CGP 47292 constituting only about 15%. Renal excretion was the predominant route of elimination for active substance related material, accounting for 84.7% of the dose. Linearity/non-linearity: The bioavailability of rufinamide is dependent on dose. As dose increases the bioavailability decreases. Pharmacokinetics in special patient groups Sex Population pharmacokinetic modelling has been used to evaluate the influence of sex on the pharmacokinetics of rufinamide. Such evaluations indicate that sex does not affect the pharmacokinetics of rufinamide to a clinically relevant extent. Renal impairment The pharmacokinetics of a single 400 mg dose of rufinamide were not altered in subjects with chronic and severe renal failure compared to healthy volunteers. However, plasma levels were reduced by approximately 30% when haemodialysis was applied after administration of rufinamide, suggesting that this may be a useful procedure in case of overdose (see sections 4.2 and 4.9). Hepatic impairment No studies have been performed in patients with hepatic impairment and therefore Inovelon tablets should not be administered to patients with severe hepatic impairment (see section 4.2). Elderly A pharmacokinetic study in older healthy volunteers did not show a significant difference in pharmacokinetic parameters compared with younger adults. Children ( 1-12 years) Children generally have lower clearance of rufinamide than adults, and this difference is related to body size with rufinamide clearance increasing with body weight. A recent population PK analysis of rufinamide on data pooled from 139 subjects (115 LGS patients and 24 healthy subjects), including 83 paediatric LGS patients (10 patients aged 1 to < 2 years, 14 patients aged 2 to < 4 years, 14 patients aged 4 to < 8 years, 21 patients aged 8 to < 12 years and 24 patients aged 12 to < 18 years) indicated that when rufinamide is dosed on a mg/kg/day basis in LGS subjects aged 1 to < 4 years, comparable exposure to that in LGS patients aged ≥ 4 years, in which efficacy has been demostrated, is achieved. Studies in new-born infants or infants and toddlers under 1 year of age have not been conducted.

פרטי מסגרת הכללה בסל
התרופה תינתן כטיפול משלים בתסמונת Lennox Gastaut.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| התרופה תינתן כטיפול משלים בתסמונת Lennox Gastaut. |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
23/01/2011
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
