Quest for the right Drug
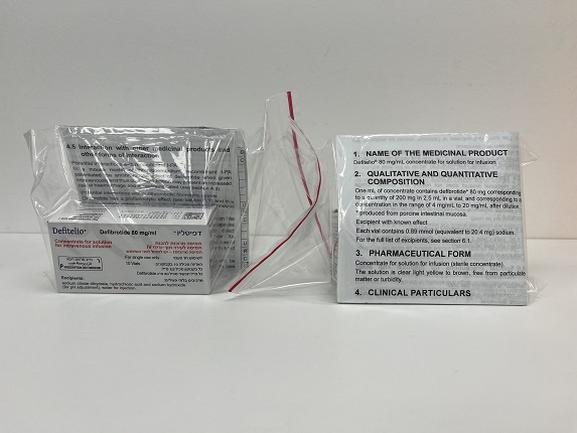
דפיטליו DEFITELIO (DEFIBROTIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תרכיז להכנת תמיסה לאינפוזיה : CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: other antithrombotic agents; ATC code: B01AX01. Mechanism of action Defibrotide is an oligonucleotide mixture with demonstrated antithrombotic, fibrinolytic, anti-adhesive and anti-inflammatory actions. The mechanism of action is multifactorial. It primarily acts through reducing excessive endothelial cell (EC) activation (endothelial dysfunction), modulating endothelial homeostasis as well as restoring thrombo-fibrinolytic balance. However, the exact mechanism of action of defibrotide is not fully elucidated. Defibrotide has demonstrated antithrombotic and fibrinolytic effects in vitro and in vivo by: increasing systemic tissue factor pathway inhibitor (TFPI), tissue plasminogen activator (t-PA) and thrombomodulin (TM) expression; decreasing von Willebrand factor (vWF) and plasminogen activator inhibitor-1 (PAI-1) expression; and enhancing the enzymatic activity of plasmin to hydrolyse fibrin clots. In vitro and in vivo studies have demonstrated that defibrotide inhibits leukocyte and platelet adhesion to endothelium by: suppressing P-selectin and vascular cell adhesion molecule-1 (VCAM)-1; interfering with lymphocyte function-associated antigen 1-intercell adhesion molecule (LFA-1-ICAM) mediated leukocyte transmigration; and increasing nitric oxide (NO), Prostaglandin I2 (PGI2) and Prostaglandin E2 (PGE2). In vitro defibrotide demonstrates anti-inflammatory effects that attenuate the release and production of reactive oxygen species and inflammatory mediators such as interleukin 6, thromboxane A2, leukotriene B4 and tumour necrosis factor-α (TNF-α). Defibrotide protects ECs from damage and promotes tissue homeostasis by decreasing fludarabine-mediated apoptosis of EC while maintaining its anti-leukemic effect and by inhibiting the expression of heparanase, shown in in vitro and in vivo studies respectively. Clinical efficacy and safety Treatment of VOD The efficacy and safety of defibrotide in the treatment of severe VOD were studied in a pivotal Phase 3 historical-controlled study (2005-01). Forty-four children and 58 adult patients with severe VOD post-HSCT, were treated with Defitelio® 25 mg/kg/day intravenous by infusion, and compared with 32 historical control patients. Median length of therapy in those treated with Defitelio® was 22 days. A significantly higher proportion of patients in the Defitelio® treated group achieved a complete response defined as total bilirubin less than 2 mg/dL and resolution of MOF (multiple organ failure); Day+100 complete response was 23.5% (24/102) with Defitelio® versus 9.4% (3/32) in the historical control (p=0.013). In addition, Day+100 survival rate was improved in the Defitelio® group with 38.2% (39/102) of the patients surviving versus 25.0% (8/32) in the historical control group (p=0.034). The efficacy data from this pivotal study are supported and confirmed with data from a dose-finding study (25 mg/kg arm) and the Open Label Treatment-IND study, as presented in Tables 1. Table 1: Treatment study results: Complete response and survival rate of severe VOD at day+100 Individual studies Historically controlled trial Dose-finding Open Label (25mg/kg/day) (25mg/kg/day treatment IND Defibrotide Historical arm) (25mg/kg/day) treated group Control Complete 23.5% 9.4% response by 43% 39.3% (24/102) (3/32) Day+100 (32/75) (201/512) p= 0.0131 Individual studies Historically controlled trial Dose-finding Open Label (25mg/kg/day) (25mg/kg/day treatment IND Defibrotide Historical arm) (25mg/kg/day) treated group Control Survival by 38.2%* 25.0%* 43.9%* 49.5%* Day+100 p=0.0341 *=Kaplan Meier estimates for time-to-event analysis by Day100 Outcome data available from 611 patients treated with Defitelio® on a compassionate use basis for non-severe and severe VOD post-transplant, are consistent with the controlled clinical studies, with complete response rate 24% (51/212) and survival 37% (78/212) in the subset of patients with severe VOD. Coppell et al in 2010 reported data from a large meta-analysis of 235 patients with severe VOD showing a background mortality rate of severe VOD of 84.3% and that this mortality rate has remained constant over several decades. Data derived from an independent US registry have shown a beneficial effect of Defitelio® in routine clinical practice. At an interim analysis of the on-going registry, data from 96 patients with severe VOD were available. The Day+100 all-cause mortality in patients with severe VOD who were not treated with defibrotide was 69%, and 61% in those patients who received defibrotide. These data are from an open label registry and the subjects were not randomised. Additional information is shown in the following Table 2. Table 2: US Registry data Non-defibrotide treated Defibrotide treated 55 41 Alive at Day +100 17 (31%) 16 (39%) VOD resolved by Day +100 16 (29%) 21 (51%) Prophylaxis A controlled randomised prophylaxis study (Study 2004-000592-33) was conducted in the paediatric patients undergoing HSCT. Patients (n=356) were randomised to receive 25 mg/kg/day from the start of conditioning or were randomised to receive no prophylaxis. A 40% reduction in the overall incidence of VOD in the Defitelio® prophylaxis arm (from 19.9% in the control arm to 12.2% in the Defitelio® arm), has been shown. The use of Defitelio® rescue treatment for all patients who developed VOD meant that the study was not designed to assess any survival advantage and none was seen in this study. In secondary analyses on the subset of patients undergoing allogeneic transplants, Defitelio® prophylaxis was also associated with a lower incidence and less Grade 2 to 4 severity of acute graft versus host disease (aGvHD) by Day+100. A separate prophylaxis study (Study 15-007) using the same dose of Defitelio® 25mg/kg/day by intravenous infusion was conducted in paediatrics (n=198) as well as adults (n=174) post HSCT. The most common primary diseases of patients were acute lymphoblastic leukemia (n=100) 26.9%, acute myelogenous leukemia (n=96) 25.8%, or neuroblastoma (n=57) 15.3%. Patients were randomised to Defitelio® plus best supportive (BSC) care or BSC alone. The primary endpoint of VOD-free survival by Day +30 post-HSCT was not met; there was no difference when Defitelio® plus BSC was compared with BSC alone. The Kaplan-Meier estimates (95% CIs) of VOD-free survival by Day +30 post-HSCT were 66.8% in the Defitelio® prophylaxis arm (57.8%, 74.4%) and 72.5% (62.3%, 80.4%) in the BSC alone. The p-value from the stratified log rank test that compared VOD-free survival over time between the two treatment arms was 0.8504. By Day +30 post-HSCT, there were 10/190 or 5.7% deaths in Defitelio® plus BSC and 5/182 or 2.9% deaths in the BSC alone. Similar proportions of participants in the Defitelio® plus BSC against the those receiving BSC alone only experienced TEAEs (99.4% vs 100%, respectively), serious TEAEs (40.9% vs 35.1%, respectively). Paediatric population In the clinical studies performed in the treatment of VOD, over 55% (780 patients) were under the age of 18 years. Safety and efficacy information in children are available from three clinical studies for the treatment of VOD: the Phase 3 pivotal treatment study (2005-01), the Treatment-IND study (2006- 05) and the dose-finding study (99-118). Safety in paediatric patients was also investigated in two additional prophylaxis studies (Study 2004-000592-33 & 15-007) described in section ‘Prophylaxis’ above. Safety and efficacy in children aged less than 1 month have not yet been established. Cardiac electrophysiology Based on the results of the QTc study, conducted in healthy subjects at therapeutic and supra-therapeutic doses, it can be concluded that Defitelio® has no significant or clinically relevant QTc-prolonging potential at doses up to 2.4 times higher than therapeutically indicated. Defitelio® might be considered free of proarrhythmic toxicity related to QT changes.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption and distribution In 52 healthy volunteers, after a single 6.25 mg/kg dose of Defitelio® given as a 2-hour infusion, the pharmacokinetic parameters were as follows: Table 3: Defitelio® pharmacokinetic parameters after intravenous infusion of 6.25 mg/kg to healthy subjects Parameter Defitelio® PK Parameters Mean ± SD Cmax (µg/mL) 17.3 ± 3.83 tmax (h)# 2.00 (1.00-2.00) AUCt (µg/mL*h) 26.9 ± 8.53 AUC (µg/mL*h) 48.1 ± 6.49 Vd (mL) 9934 ± 3807 CL (L/h) 10.4 ± 1.77 Kel (1/h) 1.25 ± 0.66 t1/2 (h) 0.71 ± 0.35 # median (min-max) Maximum plasma concentrations peaked at the end of the infusion period and declined thereafter with a rapid clearance and most of samples were undetectable 3.5 hours after the start of the infusion. Pharmacokinetic modelling simulation analysis showed that Defitelio® plasma concentrations do not accumulate upon multiple dose administration and with doses up to 4-fold the therapeutic dose. Volume of distribution is around 10 L. In vitro studies demonstrate that 93% of Defitelio® is bound to plasma proteins. Elimination After administration of the therapeutic dose (6.25 mg/kg) to healthy subjects, an average of 9.48% of the total dose administered is excreted in urine as unchanged defibrotide in 24 hours, with the majority excreted during the first collection interval of 0-4 hours (approximately 98%). Metabolism Defibrotide does not inhibit or induce CYP450s. Special populations Renal impairment Six patients with an estimated glomerular filtration rate <30 mL/min/1.73m2 (calculated using the Modification of Diet in Renal Disease equation) and not currently on dialysis were compared to 6 healthy subjects with similar baseline demographics. Defitelio® 6.25 mg/kg was administered intravenously over 2 hours to subjects every 6 hours. Compared to healthy controls, subjects with renal impairment demonstrated 1.6– and 1.4-fold increases in AUC and Cmax, respectively and a half-life of about twice that of healthy subjects. The amount of defibrotide excreted in urine over 24 hrs was about 5% of the total dose administered in those with renal impairment versus about 12% in healthy subjects. Almost all renal excretion occurs within the first 4 hours. Accumulation of defibrotide over 4 doses was not found. Difference in exposure is not considered clinically relevant and so dose adjustment is not advised for patients with renal impairment (see section 4.2). In a sub-study it was shown that haemodialysis did not remove defibrotide (see section 4.2) Hepatic impairment No formal pharmacokinetic studies have been performed in hepatic impaired patients. Defitelio® has been used in clinical studies in patients with hepatic impairment without dose adjustment with no major safety issues identified (see section 4.2).

פרטי מסגרת הכללה בסל
התרופה תינתן לחולים שעברו השתלת מח עצם (HSCT) ופיתחו מחלה חסימתית של ורידי הכבד(VOD – veno occlusive disease) בדרגת חומרה קשה (severe) (דרגת חומרה תוגדר על פי הנחיותקליניות מקובלות).
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
15/01/2015
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
