Quest for the right Drug
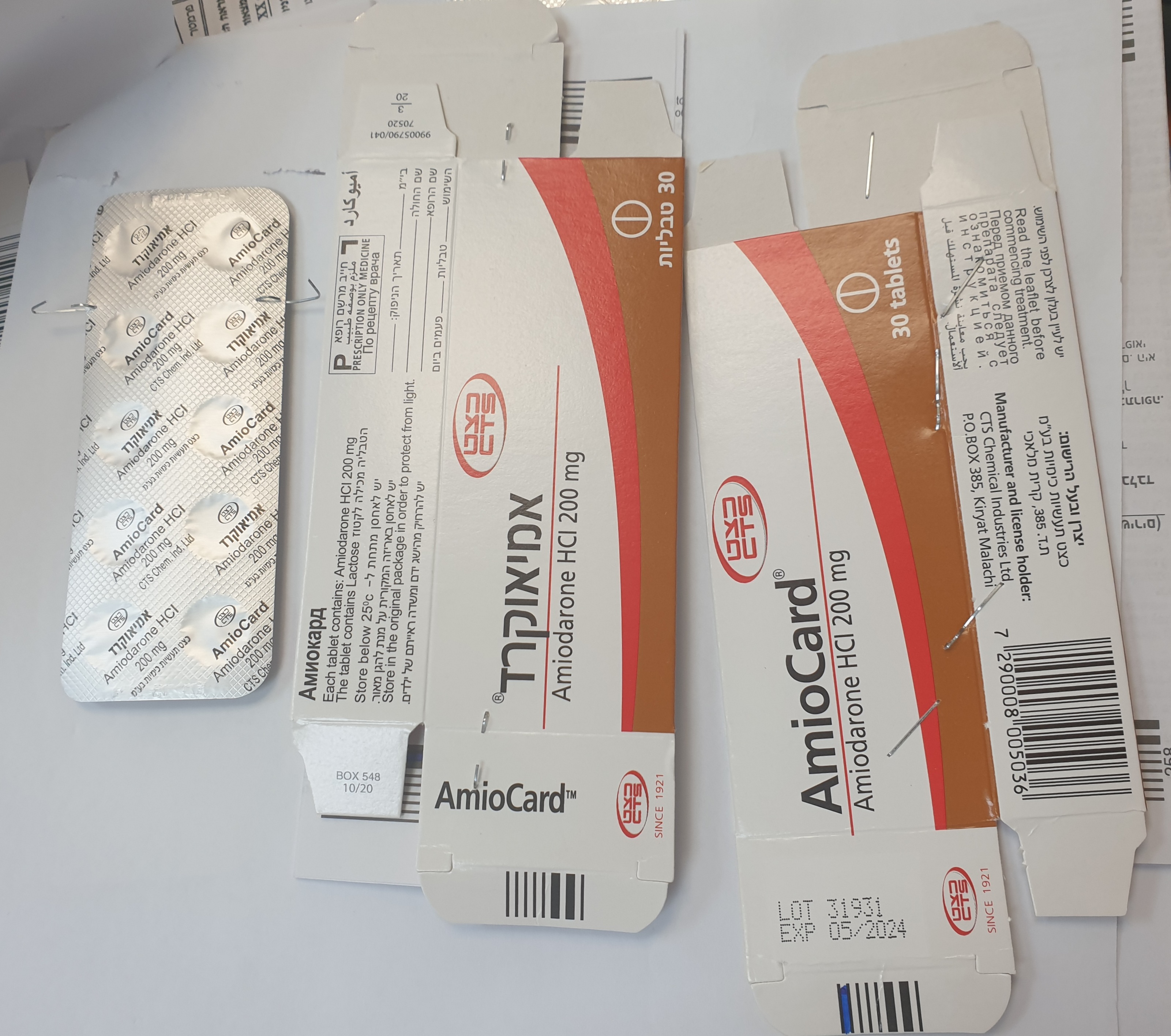
אמיאוקרד AMIOCARD (AMIODARONE HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Amiodarone can cause serious adverse reactions affecting the eyes, heart, lung, liver, thyroid gland, skin and peripheral nervous system (see section 4.8). Because these reactionsmay be delayed, patients on long-term treatment should be carefully supervised and reviewed regularly. As undesirable effects are usually dose-related, the minimum effective maintenance dose should be given. Before surgery, the anaesthetist should be informed that the patient is taking amiodarone (see sections 4.5 and 4.8). Cardiac disorders (see section 4.8): Too high a dosage may lead to severe bradycardia and to conduction disturbances with the appearance of an idioventricular rhythm, particularly in elderly patients or during digitalis therapy. In these circumstances, AMIOCARD treatment should be withdrawn. If necessary, beta- adrenostimulants or glucagon may be given. Because of the long half-life of amiodarone, if bradycardia is severe and symptomatic the insertion of a pacemaker should be considered. AMIOCARD is not contra-indicated in patients with latent or manifest heart failure but caution should be exercised as, occasionally, existing heart failure may be worsened. In such cases, AMIOCARD may be used with other appropriate therapies. The pharmacological action of amiodarone induces ECG changes: QT prolongation (related to prolonged repolarisation) with the possible development of U-waves and deformed T- waves; these changes do not reflect toxicity. In the elderly, heart rate may decrease markedly. Treatment should be discontinued in case of onset of 2nd or 3rd degree A-V block, sino-atrial block, or bifascicular block. Amiodarone has a low pro-arrhythmic effect. Onsets of new arrhythmias or worsening of treated arrhythmias, sometimes fatal, have been reported. It is important, but difficult, to differentiate a lack of efficacy of the drug from a proarrhythmic effect, whether or not this is associated with a worsening of the cardiac condition. Proarrhythmic effects generally occur inthe context of QT prolonging factors such as drug interactions and/or electrolytic disorders (see sections 4.5. and 4.8). Despite QT interval prolongation, amiodarone exhibits a low torsadogenic activity. Before starting amiodarone, it is recommended to perform an ECG and serum potassium measurement. Monitoring of ECG is recommended during treatment. Amiodarone may increase the defibrillation threshold and/or pacing threshold in patients with an implantable cardioverter defibrillator or a pacemaker, which may adversely affect the efficacy of the device. Regular tests are recommended to ensure the proper function of the device after initiation of treatment or change in posology. Severe Bradycardia and heart block (see section 4.5): Life-threatening cases of bradycardia and heart block have been observed when sofosbuvir- containing regimens are used in combination with amiodarone. Bradycardia has generally occurred within hours to days, but later cases have been mostly observed up to 2 weeks after initiating HCV treatment. Amiodarone should only be used in patients on sofosbuvir- containing regimen when other alternative anti-arrhythmic treatments are not tolerated or are contraindicated. Should concomitant use of amiodarone be considered necessary, it is recommended that patients undergo cardiac monitoring in an in-patient setting for the first 48 hours of coadministration, after which outpatient or self-monitoring of the heart rate should occur on a daily basis through at least the first 2 weeks of treatment. Due to the long half-life of amiodarone, cardiac monitoring as outlined above should also be carried out for patients who have discontinued amiodarone within the past few months and areto be initiated on sofosbuvir- containing regimen. All patients receiving amiodarone in combination with sofosbuvir-containing regimen should be warned of the symptoms of bradycardia and heart block and should be advised to seek medical advice urgently should they experience them. Primary graft dysfunction (PGD) post cardiac transplant: In retrospective studies, amiodarone use in the transplant recipient prior to heart transplant has been associated with an increased risk of PGD. PGD is a life-threatening complication of heart transplantation that presents as left, right or biventricular dysfunction occurring within the first 24 hours of transplant surgery for which there is no identifiable secondary cause (see section 4.8). Severe PGD may be irreversible. For patients who are on the heart transplant waiting list, consideration should be given to use an alternative antiarrhythmic drug as early as possible before transplant. Endocrine disorders (see section 4.8): Amiodarone may induce hypothyroidism or hyperthyroidism, particularly in patients with a personal history of thyroid disorders. Clinical and biological [including ultrasensitive TSH (usTSH)] monitoring should be performed prior to therapy in all patients. Monitoringshould be carried out during treatment, at six-monthly intervals, and for several months following its discontinuation. This is particularly important in the elderly. In patients whosehistory indicates an increased risk of thyroid dysfunction, regular assessment is recommended. Serum usTSH level should be measured when thyroid dysfunction is suspected. Amiodarone contains iodine and thus may interfere with radio-iodine uptake. However, thyroid function tests (free-T3, free-T4, usTSH) remain interpretable. Amiodarone inhibits peripheral conversion of levothyroxine (T4) to triiodothyronine (T3) and may cause isolated biochemical changes (increase in serum free-T4, free-T3 being slightly decreased or even normal) in clinically euthyroid patients. There is no reason in such cases to discontinue amiodarone treatment if there is no clinical or further biological (usTSH) evidence ofthyroid disease. Hypothyroidism: Hypothyroidism should be suspected if the following clinical signs occur: weight gain, cold intolerance, reduced activity, excessive bradycardia. The diagnosis is supported by an increase in serum usTSH and an exaggerated TSH response to TRH. T3 and T4 levels may be low. Euthyroidism is usually obtained within 3 months following the discontinuation of treatment. In life-threatening situations, amiodarone therapy can be continued, incombination with levothyroxine. The dose of levothyroxine is adjusted according to TSH levels. Hyperthyroidism: Hyperthyroidism may occur during amiodarone treatment, or, up to several months after discontinuation. Clinical features, such as weight loss, asthenia, restlessness, increase in heart rate, onset of arrhythmia, angina, congestive heart failure should alert the physician. The diagnosis is supported by a decrease in serum usTSH level, an elevated T3 and a reduced TSHresponse to thyrotropin releasing hormone. Elevation of reverse T3 (rT3) may also be found. In the case of hyperthyroidism, therapy should be withdrawn. Clinical recovery usually occurswithin a few months, although severe cases, sometimes resulting in fatalities, have been reported. Clinical recovery precedes the normalisation of thyroid function tests. Courses of anti-thyroid drugs have been used for the treatment of severe thyroid hyperactivity; large doses may be required initially. These may not always be effective and concomitant high dose corticosteroid therapy (e.g. 1 mg/kg prednisolone) may be required for several weeks. Eye disorders (see section 4.8): If blurred or decreased vision occurs, complete ophthalmologic examination including fundoscopy should be promptly performed. Appearance of optic neuropathy and/or optic neuritis requires amiodarone withdrawal due to the potential progression to blindness.Unless blurred or decreased vision occurs, opthamological examination is recommended annually. Hepato-biliary disorders (see section 4.8): Amiodarone may be associated with a variety of hepatic effects, including cirrhosis, hepatitis, jaundice and hepatic failure. Some fatalities have been reported, mainly following long-term therapy, although rarely they have occurred soon after starting treatment particularly after amiodarone. It is advisable to monitor liver function particularly transaminases before treatment and six monthly thereafter. Amiodarone dose should be reduced or the treatment discontinued if the transaminases increase exceeds three times the normal range. At the beginning of therapy, elevation of serum transaminases which can be in isolation (1.5to 3 times normal) may occur. These may return to normal with dose reduction, or sometimes spontaneously. Isolated cases of acute liver disorders with elevated serum transaminases and/or jaundice may occur; in such cases treatment should be discontinued. There have been reports of chronic liver disease. Alteration of laboratory tests which maybe minimal (transaminases elevated 1.5 to 5 times normal) or clinical signs (possiblehepatomegaly) during treatment for longer than 6 months should suggest this diagnosis. Routine monitoring of liver function tests is therefore advised. Abnormal clinical andlaboratory test results usually regress upon cessation of treatment, but fatal cases have been reported. Histological findings may resemble pseudo-alcoholic hepatitis, but they can be variable and include cirrhosis. Although there have been no literature reports on the potentiation of hepatic adverse effects ofalcohol, patients should be advised to moderate their alcohol intake while taking AMIOCARD. Nervous system disorders (see section 4.8): Amiodarone may induce peripheral sensorimotor neuropathy and/or myopathy. Both these conditions may be severe, although recovery usually occurs within several months after amiodarone withdrawal, but may sometimes be incomplete. Respiratory, thoracic and mediastinal disorders (see section 4.8): Onset of dyspnoea or non-productive cough may be related to pulmonary toxicity (hypersensitivity pneumonitis, alveolar/interstitial pneumonitis or fibrosis, pleuritis, bronchiolitis obliterans organising pneumonitis. Presenting features can include dyspnoea (which may be severe and unexplained by the current cardiac status), non-productive cough and deterioration in general health (fatigue, weight loss and fever). The onset is usually slowbut may be rapidly progressive. Whilst the majority of cases have been reported with long term therapy, a few have occurred soon after starting treatment. Patients should be carefully evaluated clinically and consideration given to chest X-rays before starting therapy. During treatment, if pulmonary toxicity is suspected, this should be repeated and associated with lung function testing including, where possible, measurement of transfer factor. However, initial radiological changes may be difficult to distinguish from pulmonary venous congestion and high-definitions computerised tomography scans may therefore be more useful than chest x-rays in confirming a diagnosis. Pulmonary toxicity has usually been reversible following early withdrawal of amiodarone therapy, with or without corticosteroid therapy. Clinical symptoms often resolve within a few weeks followed by slower radiological and lung function improvement. Some patients can deteriorate despite discontinuing AMIOCARD. Skin and subcutaneous tissue disorders (see section 4.8): Patients should be instructed to avoid exposure to sun and to use protective measures duringtherapy as patients taking AMIOCARD can become unduly sensitive to sunlight, which may persist after several months of discontinuation of AMIOCARD. In most cases symptoms are limited to tingling, burning and erythema of sun-exposed skin but severe phototoxic reactions with blistering may be seen. Severe bullous reactions: Life-threatening or even fatal cutaneous reactions Stevens-Johnson syndrome (SJS), Toxic Epidermal Necrolysis (TEN) (see section 4.8). If symptoms or signs of SJS, TEN (e.g., progressive skin rash often with blisters or mucosal lesions) are present amiodarone treatment should be discontinued immediately. Drug interactions (see section 4.5): Concomitant use of amiodarone is not recommended with the following drugs: beta- blockers, heart rate lowering calcium channel inhibitors (verapamil, diltiazem), stimulant laxative agents which may cause hypokalaemia. Increased plasma levels of flecainide have been reported with co-administration of amiodarone. The flecainide dose should be reduced accordingly and the patient closely monitored. Important Information about the ingredients of AMIOCARD Lactose AMIOCARD contains lactose. Patients with rare hereditary problems of galactose intolerance, the Lapp lactase deficiency or glucose-galactose malabsorption should not take this medicine.
Effects on Driving
4.7 Effects on ability to drive and use machines The ability to drive or to operate machinery may be impaired in patients with clinical symptoms of amiodarone-induced eye disorders.

שימוש לפי פנקס קופ''ח כללית 1994
Ventricular & supraventricular arrhythmias not responding to other treatments, tachyarrhythmias associated with Wolff-Parkinson-White syndrome
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
עלון מידע לצרכן
01.08.21 - עלון לצרכן אנגלית 01.08.21 - עלון לצרכן עברית 01.08.21 - עלון לצרכן ערבית 11.10.22 - עלון לצרכן אנגלית 11.10.22 - עלון לצרכן עברית 11.10.22 - עלון לצרכן ערבית 12.06.23 - עלון לצרכן אנגלית 12.06.23 - עלון לצרכן עברית 12.06.23 - עלון לצרכן ערבית 13.05.12 - החמרה לעלון 19.10.15 - החמרה לעלון 01.08.21 - החמרה לעלון 11.10.22 - החמרה לעלוןלתרופה במאגר משרד הבריאות
אמיאוקרד