Quest for the right Drug
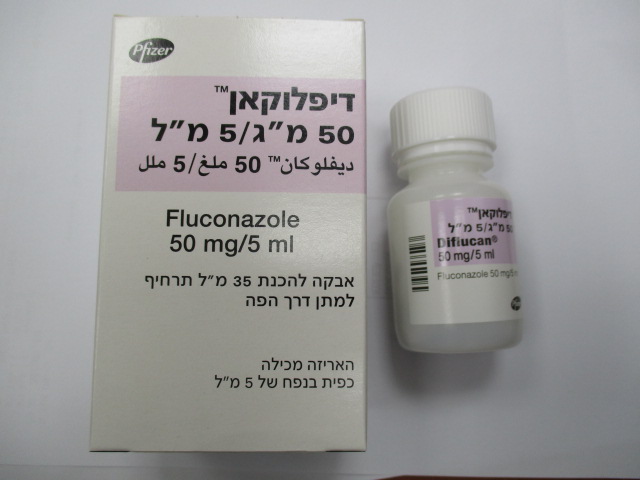
דיפלוקאן 50 מ"ג/5 מ"ל DIFLUCAN 50 MG/5 ML (FLUCONAZOLE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
אבקה להכנת תרחיף : POWDER FOR ORAL SUSPENSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antimycotics for systemic use, triazole derivatives, ATC code: J02AC01. Mechanism of action Fluconazole is a triazole antifungal agent. Its primary mode of action is the inhibition of fungal cytochrome P-450-mediated 14-alpha-lanosterol demethylation, an essential step in fungal ergosterol biosynthesis. The accumulation of 14-alpha-methyl sterols correlates with the subsequent loss of ergosterol in the fungal cell membrane and may be responsible for the antifungal activity of fluconazole. Fluconazole has been shown to be more selective for fungal cytochrome P-450 enzymes than for various mammalian cytochrome P-450 enzyme systems. Fluconazole 50 mg daily given up to 28 days has been shown not to effect testosterone plasma concentrations in males or steroid concentration in females of child-bearing age. Fluconazole 200 mg to 400 mg daily has no clinically significant effect on endogenous steroid levels or on ACTH stimulated response in healthy male volunteers. Interaction studies with antipyrine indicate that single or multiple doses of fluconazole 50 mg do not affect its metabolism. Susceptibility in vitro In vitro, fluconazole displays antifungal activity against clinically common Candida species (including C. albicans, C. parapsilosis, C. tropicalis). C. glabrata shows reduced susceptibility to fluconazole while C. krusei and C. auris are resistant to fluconazole. The MICs and epidemiological cut-off value (ECOFF) of fluconazole for C. guilliermondii are higher than for C. albicans. Fluconazole also exhibits activity in vitro against Cryptococcus neoformans and Cryptococcus gattii as well as the endemic moulds Blastomyces dermatiditis, Coccidioides immitis, Histoplasma capsulatum and Paracoccidioides brasiliensis. Pharmacokinetic/pharmacodynamic relationship In animal studies, there is a correlation between MIC values and efficacy against experimental mycoses due to Candida spp. In clinical studies, there is an almost 1:1 linear relationship between the AUC and the dose of fluconazole. There is also a direct though imperfect relationship between the AUC or dose and a successful clinical response of oral candidosis and to a lesser extent candidaemia to treatment. Similarly cure is less likely for infections caused by strains with a higher fluconazole MIC. Mechanisms of resistance Candida spp have developed a number of resistance mechanisms to azole antifungal agents. Fungal strains which have developed one or more of these resistance mechanisms are known to exhibit high minimum inhibitory concentrations (MICs) to fluconazole which impacts adversely efficacy in vivo and clinically. In usually susceptible species of Candida, the most commonly encountered mechanism of resistance development involves the target enzymes of the azoles, which are responsible for the biosynthesis of ergosterol. Resistance may be caused by mutation, increased production of an enzyme, drug efflux mechanisms, or the development of compensatory pathways. There have been reports of superinfection with Candida species other than C. albicans, which often have inherently reduced susceptibility (C. glabrata) or resistance to fluconazole (e.g. C. krusei, C. auris). Such infections may require alternative antifungal therapy. The resistance mechanisms have not been completely elucidated in some intrinsically resistant (C. krusei) or emerging (C. auris) species of Candida. EUCAST Breakpoints Based on analyses of pharmacokinetic/pharmacodynamic (PK/PD) data, susceptibility in vitro and clinical response EUCAST-AFST (European Committee on Antimicrobial Susceptibility Testing-Subcommittee on Antifungal Susceptibility Testing) has determined breakpoints for fluconazole for Candida species (EUCAST Fluconazole rationale document (2020)-version 3) ; European Committee on Antimicrobial Susceptibility Testing, Antifungal Agents, Breakpoint tables for interpretation of MICs, Version 10.0, valid from 2020-02-04). These have been divided into non-species related breakpoints; which have been determined mainly on the basis of PK/PD data and are independent of MIC distributions of specific species, and species related breakpoints for those species most frequently associated with human infection. These breakpoints are given in the table below: Antifungal Species-related breakpoints (S) in mg/L Non-species related breakpointsA S in mg/L Candida Candida Candida Candida Candida Candida albicans dubliniensis glabrata krusei parapsilosis tropicalis Fluconazole 2/4 2/4 0.001*/16 -- 2/4 2/4 2/4 S = Susceptible, R = Resistant A = Non-species related breakpoints have been determined mainly on the basis of PK/PD data and are independent of MIC distributions of specific species. They are for use only for organisms that do not have specific breakpoints. -- = Susceptibility testing not recommended as the species is a poor target for therapy with the medicinal product. * = The entire C. glabrata is in the I category. MICs against C. glabrata should be interpreted as resistant when above 16 mg/L. Susceptible category (≤0.001 mg/L) is simply to avoid misclassification of "I" strains as "S" strains. I - Susceptible, increased exposure: A microorganism is categorised as Susceptible, increased exposure when there is a high likelihood of therapeutic success because exposure to the agent is increased by adjusting the dosing regimen or by its concentration at the site of infection.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties The pharmacokinetic properties of fluconazole are similar following administration by the intravenous or oral route. Absorption After oral administration fluconazole is well absorbed, and plasma levels (and systemic bioavailability) are over 90% of the levels achieved after intravenous administration. Oral absorption is not affected by concomitant food intake. Peak plasma concentrations in the fasting state occur between 0.5 and 1.5 hours post-dose. Plasma concentrations are proportional to dose. Ninety percent steady state levels are reached by day 4-5 with multiple once daily dosing. Administration of a loading dose (on day 1) of twice the usual daily dose enables plasma levels to approximate to 90% steady-state levels by day 2. Distribution The apparent volume of distribution approximates to total body water. Plasma protein binding is low (11-12%). Fluconazole achieves good penetration in all body fluids studied. The levels of fluconazole in saliva and sputum are similar to plasma levels. In patients with fungal meningitis, fluconazole levels in the CSF are approximately 80% the corresponding plasma levels. High skin concentration of fluconazole, above serum concentrations, are achieved in the stratum corneum, epidermis-dermis and eccrine sweat. Fluconazole accumulates in the stratum corneum. At a dose of 50 mg once daily, the concentration of fluconazole after 12 days was 73 µg/g and 7 days after cessation of treatment the concentration was still 5.8 µg/g. At the 150 mg once-a-week dose, the concentration of fluconazole in stratum corneum on day 7 was 23.4 µg/g and 7 days after the second dose was still 7.1 µg/g. Concentration of fluconazole in nails after 4 months of 150 mg once-a-week dosing was 4.05 µg/g in healthy and 1.8 µg/g in diseased nails; and, fluconazole was still measurable in nail samples 6 months after the end of therapy. Biotransformation Fluconazole is metabolised only to a minor extent. Of a radioactive dose, only 11% is excreted in a changed form in the urine. Fluconazole is a moderate inhibitor of the isozymes CYP2C9 and CYP3A4 (see section 4.5). Fluconazole is also a strong inhibitor of the isozyme CYP2C19. Elimination Plasma elimination half-life for fluconazole is approximately 30 hours. The major route of excretion is renal, with approximately 80% of the administered dose appearing in the urine as unchanged medicinal product. Fluconazole clearance is proportional to creatinine clearance. There is no evidence of circulating metabolites. The long plasma elimination half-life provides the basis for single dose therapy for vaginal candidiasis, once daily and once weekly dosing for other indications. Pharmacokinetics in renal impairment In patients with severe renal insufficiency, (GFR< 20 ml/min) half life increased from 30 to 98 hours. Consequently, reduction of the dose is needed. Fluconazole is removed by haemodialysis and to a lesser extent by peritoneal dialysis. After three hours of haemodialysis session, around 50% of fluconazole is eliminated from blood. Pharmacokinetics during lactation A pharmacokinetic study in ten lactating women, who had temporarily or permanently stopped breast-feeding their infants, evaluated fluconazole concentrations in plasma and breast milk for 48 hours following a single 150 mg dose of Fluconazole. Fluconazole was detected in breast milk at an average concentration of approximately 98% of those in maternal plasma. The mean peak breast milk concentration was 2.61 mg/L at 5.2 hours post-dose. The estimated daily infant dose of fluconazole from breast milk (assuming mean milk consumption of 150 ml/kg/day) based on the mean peak milk concentration is 0.39 mg/kg/day, which is approximately 40% of the recommended neonatal dose (<2 weeks of age) or 13% of the recommended infant dose for mucosal candidiasis. Pharmacokinetics in children Pharmacokinetic data were assessed for 113 paediatric patients from 5 studies; 2 single-dose studies, 2 multiple-dose studies, and a study in premature neonates. Data from one study were not interpretable due to changes in formulation pathway through the study. Additional data were available from a compassionate use study. After administration of 2-8 mg/kg fluconazole to children between the ages of 9 months to 15 years, an AUC of about 38 µgh/ml was found per 1 mg/kg dose units. The average fluconazole plasma elimination half-life varied between 15 and 18 hours and the distribution volume was approximately 880 ml/kg after multiple doses. A higher fluconazole plasma elimination half-life of approximately 24 hours was found after a single dose. This is comparable with the fluconazole plasma elimination half-life after a single administration of 3 mg/kg i.v. to children of 11 days-11 months old. The distribution volume in this age group was about 950 ml/kg. Experience with fluconazole in neonates is limited to pharmacokinetic studies in premature newborns. The mean age at first dose was 24 hours (range 9-36 hours) and mean birth weight was 0.9 kg (range 0.75-1.10 kg) for 12 pre-term neonates of average gestation around 28 weeks. Seven patients completed the protocol; a maximum of five 6 mg/kg intravenous infusions of fluconazole were administered every 72 hours. The mean half-life (hours) was 74 (range 44-185) on day 1 which decreased, with time to a mean of 53 (range 30-131) on day 7 and 47 (range 27-68) on day 13. The area under the curve (microgram.h/ml) was 271 (range 173-385) on day 1 and increased with a mean of 490 (range 292-734) on day 7 and decreased with a mean of 360 (range 167-566) on day 13. The volume of distribution (ml/kg) was 1183 (range 1070-1470) on day 1 and increased, with time, to a mean of 1184 (range 510-2130) on day 7 and 1328 (range 1040-1680) on day 13. Pharmacokinetics in elderly A pharmacokinetic study was conducted in 22 subjects, 65 years of age or older receiving a single 50 mg oral dose of fluconazole. Ten of these patients were concomitantly receiving diuretics. The Cmax was 1.54 µg/ml and occurred at 1.3 hours post-dose. The mean AUC was 76.4 ± 20.3 µgh/ml, and the mean terminal half-life was 46.2 hours. These pharmacokinetic parameter values are higher than analogous values reported for normal young male volunteers. Coadministration of diuretics did not significantly alter AUC or Cmax. In addition, creatinine clearance (74 ml/min), the percent of medicinal product recovered unchanged in urine (0-24 hr, 22%) and the fluconazole renal clearance estimates (0.124 ml/min/kg) for the elderly were generally lower than those of younger volunteers. Thus, the alteration of fluconazole disposition in the elderly appears to be related to reduced renal function characteristics of this group.

פרטי מסגרת הכללה בסל
התרופה תינתן: 1. לטיפול בחולה הסובל מקריפטוקוקוזיס, כולל דלקת קרום מוח קריפטוקוקאלית. 2. לטיפול בחולה הסובל מקנדידיאזיס מוקוזאלית. 3. לחולה העובר השתלת מוח עצם, או מטופל בכימותרפיה ציטוטוקסית או מטופל בהקרנות - לצורך טיפולי או מניעתי של קנדידיאזיס.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| לחולה העובר השתלת מוח עצם, או מטופל בכימותרפיה ציטוטוקסית או מטופל בהקרנות - לצורך טיפולי או מניעתי של קנדידיאזיס. | 01/03/2002 | |||
| לטיפול בחולה הסובל מקנדידיאזיס מוקוזאלית. | 01/03/2002 | |||
| לטיפול בחולה הסובל מקריפטוקוקוזיס, כולל דלקת קרום מוח קריפטוקוקאלית | 01/03/2002 |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/03/2002
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
09.08.22 - עלון לצרכן אנגלית 09.08.22 - עלון לצרכן עברית 09.08.22 - עלון לצרכן ערבית 06.12.22 - עלון לצרכן עברית 06.03.23 - עלון לצרכן אנגלית 06.03.23 - עלון לצרכן עברית 06.03.23 - עלון לצרכן ערבית 20.05.24 - עלון לצרכן עברית 04.07.24 - עלון לצרכן אנגלית 12.07.24 - עלון לצרכן ערבית 05.09.19 - החמרה לעלון 14.10.20 - החמרה לעלון 15.07.21 - החמרה לעלון 20.12.21 - החמרה לעלון 04.08.22 - החמרה לעלון 06.12.22 - החמרה לעלוןלתרופה במאגר משרד הבריאות
דיפלוקאן 50 מ"ג/5 מ"ל