Quest for the right Drug
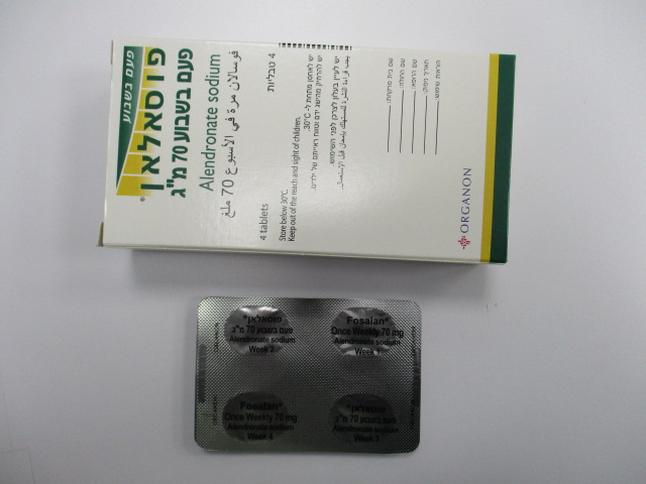
פוסאלאן פעם בשבוע 70 מ"ג FOSALAN ONCE-WEEKLY 70 MG (ALENDRONATE AS SODIUM)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
12.2 Pharmacodynamics Alendronate is a bisphosphonate that binds to bone hydroxyapatite and specifically inhibits the activity of osteoclasts, the bone-resorbing cells. Alendronate reduces bone resorption with no direct effect on bone formation, although the latter process is ultimately reduced because bone resorption and formation are coupled during bone turnover. Osteoporosis in Postmenopausal Women Osteoporosis is characterized by low bone mass that leads to an increased risk of fracture. The diagnosis can be confirmed by the finding of low bone mass, evidence of fracture on x-ray, a history of osteoporotic fracture, or height loss or kyphosis, indicative of vertebral (spinal) fracture. Osteoporosis occurs in both males and females but is most common among women following the menopause, when bone turnover increases and the rate of bone resorption exceeds that of bone formation. These changes result in progressive bone loss and lead to osteoporosis in a significant proportion of women over age 50. Fractures, usually of the spine, hip, and wrist, are the common consequences. From age 50 to age 90, the risk of hip fracture in white women increases 50-fold and the risk of vertebral fracture 15- to 30-fold. It is estimated that approximately 40% of 50-year-old women will sustain one or more osteoporosis-related fractures of the spine, hip, or wrist during their remaining lifetimes. Hip fractures, in particular, are associated with substantial morbidity, disability, and mortality. Daily oral doses of alendronate (5, 20, and 40 mg for six weeks) in postmenopausal women produced biochemical changes indicative of dose-dependent inhibition of bone resorption, including decreases in urinary calcium and urinary markers of bone collagen degradation (such as deoxypyridinoline and cross- linked N-telopeptides of type I collagen). These biochemical changes tended to return toward baseline values as early as 3 weeks following the discontinuation of therapy with alendronate and did not differ from placebo after 7 months. Long-term treatment of osteoporosis with FOSALAN 10 mg/day (for up to five years) reduced urinary excretion of markers of bone resorption, deoxypyridinoline and cross-linked N-telopeptides of type l collagen, by approximately 50% and 70%, respectively, to reach levels similar to those seen in healthy premenopausal women. Similar decreases were seen in patients in osteoporosis prevention studies who received FOSALAN 5 mg/day. The decrease in the rate of bone resorption indicated by these markers was evident as early as one month and at three to six months reached a plateau that was maintained for the entire duration of treatment with FOSALAN. In osteoporosis treatment studies FOSALAN 10 mg/day decreased the markers of bone formation, osteocalcin and bone specific alkaline phosphatase by approximately 50%, and total serum alkaline phosphatase by approximately 25 to 30% to reach a plateau after 6 to 12 months. In osteoporosis prevention studies FOSALAN 5 mg/day decreased osteocalcin and total serum alkaline phosphatase by approximately 40% and 15%, respectively. Similar reductions in the rate of bone turnover were observed in postmenopausal women during one-year studies with once weekly FOSALAN 70 mg for the treatment of osteoporosis and once weekly FOSALAN 35 mg for the prevention of osteoporosis. These data indicate that the rate of bone turnover reached a new steady-state, despite the progressive increase in the total amount of alendronate deposited within bone. As a result of inhibition of bone resorption, asymptomatic reductions in serum calcium and phosphate concentrations were also observed following treatment with FOSALAN. In the long-term studies, reductions from baseline in serum calcium (approximately 2%) and phosphate (approximately 4 to 6%) were evident the first month after the initiation of FOSALAN 10 mg. No further decreases in serum calcium were observed for the five-year duration of treatment; however, serum phosphate returned toward prestudy levels during years three through five. Similar reductions were observed with FOSALAN 5 mg/day. In one-year studies with once weekly FOSALAN 35 and 70 mg, similar reductions were observed at 6 and 12 months. The reduction in serum phosphate may reflect not only the positive bone mineral balance due to FOSALAN but also a decrease in renal phosphate reabsorption. Osteoporosis in Men Treatment of men with osteoporosis with FOSALAN 10 mg/day for two years reduced urinary excretion of cross-linked N-telopeptides of type I collagen by approximately 60% and bone-specific alkaline phosphatase by approximately 40%. Similar reductions were observed in a one-year study in men with osteoporosis receiving once weekly FOSALAN 70 mg.
Pharmacokinetic Properties
12.3 Pharmacokinetics Absorption Relative to an intravenous reference dose, the mean oral bioavailability of alendronate in women was 0.64% for doses ranging from 5 to 70 mg when administered after an overnight fast and two hours before a standardized breakfast. Oral bioavailability of the 10 mg tablet in men (0.59%) was similar to that in women when administered after an overnight fast and 2 hours before breakfast. A study examining the effect of timing of a meal on the bioavailability of alendronate was performed in 49 postmenopausal women. Bioavailability was decreased (by approximately 40%) when 10 mg alendronate was administered either 0.5 or 1 hour before a standardized breakfast, when compared to dosing 2 hours before eating. In studies of treatment and prevention of osteoporosis, alendronate was effective when administered at least 30 minutes before breakfast. Bioavailability was negligible whether alendronate was administered with or up to two hours after a standardized breakfast. Concomitant administration of alendronate with coffee or orange juice reduced bioavailability by approximately 60%. Distribution Preclinical studies (in male rats) show that alendronate transiently distributes to soft tissues following 1 mg/kg intravenous administration but is then rapidly redistributed to bone or excreted in the urine. The mean steady-state volume of distribution, exclusive of bone, is at least 28 L in humans. Concentrations of drug in plasma following therapeutic oral doses are too low (less than 5 ng/mL) for analytical detection. Protein binding in human plasma is approximately 78%. Metabolism There is no evidence that alendronate is metabolized in animals or humans. Excretion Following a single intravenous dose of [14C]alendronate, approximately 50% of the radioactivity was excreted in the urine within 72 hours and little or no radioactivity was recovered in the feces. Following a single 10 mg intravenous dose, the renal clearance of alendronate was 71 mL/min (64, 78; 90% confidence interval [CI]), and systemic clearance did not exceed 200 mL/min. Plasma concentrations fell by more than 95% within 6 hours following intravenous administration. The terminal half-life in humans is estimated to exceed 10 years, probably reflecting release of alendronate from the skeleton. Based on the above, it is estimated that after 10 years of oral treatment with FOSALAN (10 mg daily) the amount of alendronate released daily from the skeleton is approximately 25% of that absorbed from the gastrointestinal tract. Specific Populations Gender: Bioavailability and the fraction of an intravenous dose excreted in urine were similar in men and women. Geriatric: Bioavailability and disposition (urinary excretion) were similar in elderly and younger patients. No dosage adjustment is necessary in elderly patients. Race: Pharmacokinetic differences due to race have not been studied. Renal Impairment: Preclinical studies show that, in rats with kidney failure, increasing amounts of drug are present in plasma, kidney, spleen, and tibia. In healthy controls, drug that is not deposited in bone is rapidly excreted in the urine. No evidence of saturation of bone uptake was found after 3 weeks dosing with cumulative intravenous doses of 35 mg/kg in young male rats. Although no formal renal impairment pharmacokinetic study has been conducted in patients, it is likely that, as in animals, elimination of alendronate via the kidney will be reduced in patients with impaired renal function. Therefore, somewhat greater accumulation of alendronate in bone might be expected in patients with impaired renal function. No dosage adjustment is necessary for patients with creatinine clearance 35 to 60 mL/min. FOSALAN is not recommended for patients with creatinine clearance less than 35 mL/min due to lack of experience with alendronate in renal failure. Hepatic Impairment: As there is evidence that alendronate is not metabolized or excreted in the bile, no studies were conducted in patients with hepatic impairment. No dosage adjustment is necessary. Drug Interactions Intravenous ranitidine was shown to double the bioavailability of oral alendronate. The clinical significance of this increased bioavailability and whether similar increases will occur in patients given oral H2-antagonists is unknown. In healthy subjects, oral prednisone (20 mg three times daily for five days) did not produce a clinically meaningful change in the oral bioavailability of alendronate (a mean increase ranging from 20 to 44%). Products containing calcium and other multivalent cations are likely to interfere with absorption of alendronate.

פרטי מסגרת הכללה בסל
הוראות לשימוש בתרופות ALENDRONATE SODIUM, RISEDRONATE SODIUM, RALOXIFENE, BAZEDOXIFENE:א. התרופות האמורות יינתנו לטיפול באוסטיאופורוזיס ובהתאם לכללים האלה: 1. למטופלות בכל מקרה של אוסטיאופורוזיס: א. עם שבר אוסטיאופורוטי קיים או בנוכחות תולדות של שבר אוסטיאופורוטי; ב. עם T score (ההפרש בין צפיפות העצם של המטופל לבין צפיפות העצם הממוצעת לאדם באוכלוסיה) השווה ל-3.5 או הנמוך מ-3.5- ;ג. בנשים מעל גיל 60 שנים עם T score השווה ל-2.5 או הנמוך מ-2.5- ;ד. שנגרם מאחת המחלות הידועות כגורמות לו; ה. בכל מקרה של אוסטיאופורוזיס שנגרם כתוצאה מטיפול בתכשיר גלוקוקורטיקואידי. 2. למטופלים בכל מקרה של אוסטיאופורוזיס: א. עם שבר אוסטיאופורוטי קיים או בנוכחות תולדות של שבר אוסטיאופורוטי; ב. מעל גיל 60 עם T score השווה ל-2.5 או הנמוך מ-2.5-; ג. בכל מקרה של אוסטיאופורוזיס שנגרם כתוצאה מטיפול בתכשיר גלוקוקורטיקואידי;. ד. שנגרם מאחת המחלות הידועות כגורמות לו; 3. התרופות יינתנו למטופלים ומטופלות בהתאם לחלוקה זו: א. ALENDRONATE SODIUM, RISEDRONATE SODIUM - למטופלים ולמטופלות;ב. RALOXIFENE, BAZEDOXIFENE - למטופלות בלבד.2. אף אחת מן התרופות האמורות לא תינתן בשילוב עם התרופות האחרות.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| ALENDRONATE | ||||
| אוסטיאופורוזיס |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/2000
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
