Quest for the right Drug
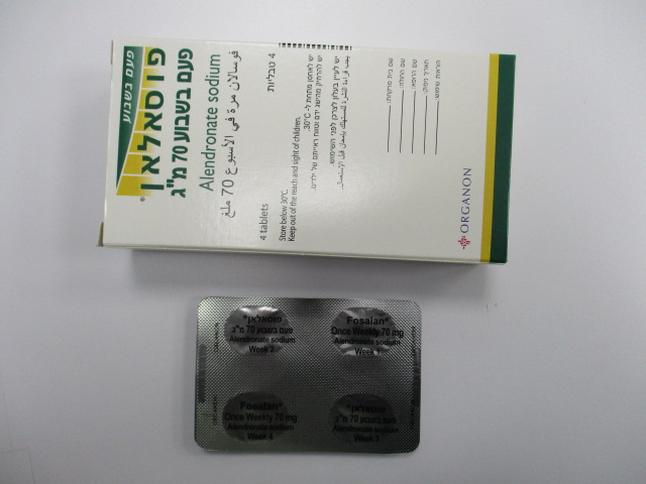
פוסאלאן פעם בשבוע 70 מ"ג FOSALAN ONCE-WEEKLY 70 MG (ALENDRONATE AS SODIUM)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
5 WARNINGS AND PRECAUTIONS 5.1 Upper Gastrointestinal Adverse Reactions FOSALAN, like other bisphosphonates administered orally, may cause local irritation of the upper gastrointestinal mucosa. Because of these possible irritant effects and a potential for worsening of the underlying disease, caution should be used when FOSALAN is given to patients with active upper gastrointestinal problems (such as known Barrett's esophagus, dysphagia, other esophageal diseases, gastritis, duodenitis, or ulcers). Esophageal adverse experiences, such as esophagitis, esophageal ulcers and esophageal erosions, occasionally with bleeding and rarely followed by esophageal stricture or perforation, have been reported in patients receiving treatment with oral bisphosphonates including FOSALAN. In some cases these have been severe and required hospitalization. Physicians should therefore be alert to any signs or symptoms signaling a possible esophageal reaction and patients should be instructed to discontinue FOSALAN and seek medical attention if they develop dysphagia, odynophagia, retrosternal pain or new or worsening heartburn. The risk of severe esophageal adverse experiences appears to be greater in patients who lie down after taking oral bisphosphonates including FOSALAN and/or who fail to swallow oral bisphosphonates including FOSALAN with the recommended full glass (not less than 200 ml) of water, and/or who continue to take oral bisphosphonates including FOSALAN after developing symptoms suggestive of esophageal irritation. Therefore, it is very important that the full dosing instructions are provided to, and understood by, the patient [see Dosage and Administration (2.3)]. In patients who cannot comply with dosing instructions due to mental disability, therapy with FOSALAN should be used under appropriate supervision. There have been post-marketing reports of gastric and duodenal ulcers with oral bisphosphonate use, some severe and with complications, although no increased risk was observed in controlled clinical trials [see Adverse Reactions (6.2)]. 5.2 Mineral Metabolism Hypocalcemia must be corrected before initiating therapy with FOSALAN [see Contraindications (4)]. Other disorders affecting mineral metabolism (such as vitamin D deficiency) should also be effectively treated. In patients with these conditions, serum calcium and symptoms of hypocalcemia should be monitored during therapy with FOSALAN. Presumably due to the effects of FOSALAN on increasing bone mineral, small, asymptomatic decreases in serum calcium and phosphate may occur. 5.3 Musculoskeletal Pain In post-marketing experience, severe and occasionally incapacitating bone, joint, and/or muscle pain has been reported in patients taking bisphosphonates that are approved for the prevention and treatment of osteoporosis [see Adverse Reactions (6.2)]. This category of drugs includes FOSALAN (alendronate). Most of the patients were postmenopausal women. The time to onset of symptoms varied from one day to several months after starting the drug. Discontinue use if severe symptoms develop. Most patients had relief of symptoms after stopping. A subset had recurrence of symptoms when rechallenged with the same drug or another bisphosphonate. In placebo-controlled clinical studies of FOSALAN, the percentages of patients with these symptoms were similar in the FOSALAN and placebo groups. 5.4 Osteonecrosis of the Jaw Osteonecrosis of the jaw (ONJ), which can occur spontaneously, is generally associated with tooth extraction and/or local infection with delayed healing, and has been reported in patients taking bisphosphonates, including FOSALAN. Known risk factors for osteonecrosis of the jaw include invasive dental procedures (e.g., tooth extraction, dental implants, boney surgery), diagnosis of cancer, concomitant therapies (e.g., chemotherapy, corticosteroids, angiogenesis inhibitors), poor oral hygiene, and co-morbid disorders (e.g., periodontal and/or other pre-existing dental disease, anemia, coagulopathy, infection, ill- fitting dentures) and smoking. The risk of ONJ may increase with duration of exposure to bisphosphonates. For patients requiring invasive dental procedures, discontinuation of bisphosphonate treatment may reduce the risk for ONJ. Clinical judgment of the treating physician and/or oral surgeon should guide the management plan of each patient based on individual benefit/risk assessment. Patients who develop osteonecrosis of the jaw while on bisphosphonate therapy should receive care by an oral surgeon. In these patients, extensive dental surgery to treat ONJ may exacerbate the condition. Discontinuation of bisphosphonate therapy should be considered based on individual benefit/risk assessment. 5.5 Osteonecrosis of the external auditory canal Osteonecrosis of the external auditory canal has been reported with bisphosphonates, mainly in association with long-term therapy. Possible risk factors for osteonecrosis of the external auditory canal include steroid use and chemotherapy and/or local risk factors such as infection or trauma. The possibility of osteonecrosis of the external auditory canal should be considered in patients receiving bisphosphonates who present with ear symptoms such as pain or discharge, or chronic ear infections 5.6 Atypical Subtrochanteric and Diaphyseal Femoral Fractures Atypical, low-energy, or low trauma fractures of the femoral shaft have been reported in bisphosphonate- treated patients. These fractures can occur anywhere in the femoral shaft from just below the lesser trochanter to above the supracondylar flare and are transverse or short oblique in orientation without evidence of comminution. Causality has not been established as these fractures also occur in osteoporotic patients who have not been treated with bisphosphonates. Atypical femur fractures most commonly occur with minimal or no trauma to the affected area. They may be bilateral and many patients report prodromal pain in the affected area, usually presenting as dull, aching thigh pain, weeks to months before a complete fracture occurs. A number of reports note that patients were also receiving treatment with glucocorticoids (e.g. prednisone) at the time of fracture. Any patient with a history of bisphosphonate exposure who presents with thigh or groin pain should be suspected of having an atypical fracture and should be evaluated to rule out an incomplete femur fracture. Patients presenting with an atypical fracture should also be assessed for symptoms and signs of fracture in the contralateral limb. Interruption of bisphosphonate therapy should be considered, pending a risk/benefit assessment, on an individual basis. 5.7 Renal Impairment FOSALAN is not recommended for patients with creatinine clearance less than 35 mL/min. 6 ADVERSE REACTIONS 6.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice. Treatment of Osteoporosis in Postmenopausal Women Daily Dosing The safety of FOSALAN in the treatment of postmenopausal osteoporosis was assessed in four clinical trials that enrolled 7453 women aged 44-84 years. Study 1 and Study 2 were identically designed, three- year, placebo-controlled, double-blind, multicenter studies (United States and Multinational n=994); Study 3 was the three-year vertebral fracture cohort of the Fracture Intervention Trial [FIT] (n=2027) and Study 4 was the four-year clinical fracture cohort of FIT (n=4432). Overall, 3620 patients were exposed to placebo and 3432 patients exposed to FOSALAN. Patients with pre-existing gastrointestinal disease and concomitant use of non-steroidal anti-inflammatory drugs were included in these clinical trials. In Study 1 and Study 2 all women received 500 mg elemental calcium as carbonate. In Study 3 and Study 4 all women with dietary calcium intake less than 1000 mg per day received 500 mg calcium and 250 international units Vitamin D per day. Among patients treated with alendronate 10 mg or placebo in Study 1 and Study 2, and all patients in Study 3 and Study 4, the incidence of all-cause mortality was 1.8% in the placebo group and 1.8% in the FOSALAN group. The incidence of serious adverse event was 30.7% in the placebo group and 30.9% in the FOSALAN group. The percentage of patients who discontinued the study due to any clinical adverse event was 9.5% in the placebo group and 8.9% in the FOSALAN group. Adverse reactions from these studies considered by the investigators as possibly, probably, or definitely drug related in greater than or equal to 1% of patients treated with either FOSALAN or placebo are presented in Table 1. Table 1: Osteoporosis Treatment Studies in Postmenopausal Women Adverse Reactions Considered Possibly, Probably, or Definitely Drug Related by the Investigators and Reported in Greater Than or Equal to 1% of Patients United States/Multinational Fracture Intervention Trial Studies FOSALAN* Placebo FOSALAN† Placebo % % % % (n=196) (n=397) (n=3236) (n=3223) Gastrointestinal abdominal pain 6.6 4.8 1.5 1.5 nausea 3.6 4.0 1.1 1.5 dyspepsia 3.6 3.5 1.1 1.2 constipation 3.1 1.8 0.0 0.2 diarrhea 3.1 1.8 0.6 0.3 flatulence 2.6 0.5 0.2 0.3 acid regurgitation 2.0 4.3 1.1 0.9 esophageal ulcer 1.5 0.0 0.1 0.1 vomiting 1.0 1.5 0.2 0.3 dysphagia 1.0 0.0 0.1 0.1 abdominal distention 1.0 0.8 0.0 0.0 gastritis 0.5 1.3 0.6 0.7 Musculoskeletal musculoskeletal (bone, muscle or joint) pain 4.1 2.5 0.4 0.3 muscle cramp 0.0 1.0 0.2 0.1 Nervous System/Psychiatric headache 2.6 1.5 0.2 0.2 dizziness 0.0 1.0 0.0 0.1 Special Senses taste perversion 0.5 1.0 0.1 0.0 * 10 mg/day for three years † 5 mg/day for 2 years and 10 mg/day for either 1 or 2 additional years Rash and erythema have occurred. Gastrointestinal Adverse Reactions: One patient treated with FOSALAN (10 mg/day), who had a history of peptic ulcer disease and gastrectomy and who was taking concomitant aspirin, developed an anastomotic ulcer with mild hemorrhage, which was considered drug related. Aspirin and FOSALAN were discontinued and the patient recovered. In the Study 1 and Study 2 populations, 49-54% had a history of gastrointestinal disorders at baseline and 54-89% used nonsteroidal anti-inflammatory drugs or aspirin at some time during the studies. [See Warnings and Precautions (5.1).] Laboratory Test Findings: In double-blind, multicenter, controlled studies, asymptomatic, mild, and transient decreases in serum calcium and phosphate were observed in approximately 18% and 10%, respectively, of patients taking FOSALAN versus approximately 12% and 3% of those taking placebo. However, the incidences of decreases in serum calcium to less than 8.0 mg/dL (2.0 mM) and serum phosphate to less than or equal to 2.0 mg/dL (0.65 mM) were similar in both treatment groups. Weekly Dosing The safety of FOSALAN 70 mg once weekly for the treatment of postmenopausal osteoporosis was assessed in a one-year, double-blind, multicenter study comparing FOSALAN 70 mg once weekly and FOSALAN 10 mg daily. The overall safety and tolerability profiles of once weekly FOSALAN 70 mg and FOSALAN 10 mg daily were similar. The adverse reactions considered by the investigators as possibly, probably, or definitely drug related in greater than or equal to 1% of patients in either treatment group are presented in Table 2. Table 2: Osteoporosis Treatment Studies in Postmenopausal Women Adverse Reactions Considered Possibly, Probably, or Definitely Drug Related by the Investigators and Reported in Greater Than or Equal to 1% of Patients Once Weekly FOSALAN FOSALAN 70 mg 10 mg/day % % (n=519) (n=370) Gastrointestinal abdominal pain 3.7 3.0 dyspepsia 2.7 2.2 acid regurgitation 1.9 2.4 nausea 1.9 2.4 abdominal distention 1.0 1.4 constipation 0.8 1.6 flatulence 0.4 1.6 gastritis 0.2 1.1 gastric ulcer 0.0 1.1 Musculoskeletal musculoskeletal (bone, 2.9 3.2 muscle, joint) pain muscle cramp 0.2 1.1 Concomitant Use with Estrogen/Hormone Replacement Therapy In two studies (of one and two years’ duration) of postmenopausal osteoporotic women (total: n=853), the safety and tolerability profile of combined treatment with FOSALAN 10 mg once daily and estrogen ± progestin (n=354) was consistent with those of the individual treatments. Osteoporosis in Men In two placebo-controlled, double-blind, multicenter studies in men (a two-year study of FOSALAN 10 mg/day and a one-year study of once weekly FOSALAN 70 mg) the rates of discontinuation of therapy due to any clinical adverse event were 2.7% for FOSALAN 10 mg/day vs. 10.5% for placebo, and 6.4% for once weekly FOSALAN 70 mg vs. 8.6% for placebo. The adverse reactions considered by the investigators as possibly, probably, or definitely drug related in greater than or equal to 2% of patients treated with either FOSALAN or placebo are presented in Table 4. Table 3: Osteoporosis Studies in Men Adverse Reactions Considered Possibly, Probably, or Definitely Drug Related by the Investigators and Reported in Greater Than or Equal to 2% of Patients Two-year Study One-year Study Once Weekly FOSALAN Placebo FOSALAN 70 mg Placebo 10 mg/day % % % % (n=109) (n=58) (n=146) (n=95) Gastrointestinal acid regurgitation 4.1 3.2 0.0 0.0 flatulence 4.1 1.1 0.0 0.0 gastroesophageal 0.7 3.2 2.8 0.0 reflux disease dyspepsia 3.4 0.0 2.8 1.7 diarrhea 1.4 1.1 2.8 0.0 abdominal pain 2.1 1.1 0.9 3.4 nausea 2.1 0.0 0.0 0.0 6.2 Post-Marketing Experience The following adverse reactions have been identified during post-approval use of FOSALAN. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Body as a Whole: hypersensitivity reactions including urticaria and angioedema. Transient symptoms of myalgia, malaise, asthenia and fever have been reported with FOSALAN, typically in association with initiation of treatment. Symptomatic hypocalcemia has occurred, generally in association with predisposing conditions. Peripheral edema. Gastrointestinal: esophagitis, esophageal erosions, esophageal ulcers, esophageal stricture or perforation, and oropharyngeal ulceration. Gastric or duodenal ulcers, some severe and with complications, have also been reported [see Dosage and Administration (2.3); Warnings and Precautions (5.1)]. Localized osteonecrosis of the jaw, generally associated with tooth extraction and/or local infection with delayed healing, has been reported [see Warnings and Precautions (5.4)]. Musculoskeletal: bone, joint, and/or muscle pain, occasionally severe, and incapacitating [see Warnings and Precautions (5.3)]; joint swelling; low-energy femoral shaft and subtrochanteric fractures [see Warnings and Precautions (5.5)]. Nervous System: dizziness and vertigo. Pulmonary: acute asthma exacerbations. Skin: rash (occasionally with photosensitivity), pruritus, alopecia, severe skin reactions, including Stevens-Johnson syndrome and toxic epidermal necrolysis. Special Senses: uveitis, scleritis or episcleritis. Very rare: osteonecrosis of the external auditory canal (bisphosphonate class adverse reaction). Reporting of suspected adverse reaction Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form (https://sideeffects.health.gov.il). 6.3 Driving and using machines FOSALAN may have a moderate influence on the ability to drive and use machines in patients that experience certain adverse reactions (for example blurred vision, dizziness and severe bone muscle or joint pain).
Effects on Driving

פרטי מסגרת הכללה בסל
הוראות לשימוש בתרופות ALENDRONATE SODIUM, RISEDRONATE SODIUM, RALOXIFENE, BAZEDOXIFENE:א. התרופות האמורות יינתנו לטיפול באוסטיאופורוזיס ובהתאם לכללים האלה: 1. למטופלות בכל מקרה של אוסטיאופורוזיס: א. עם שבר אוסטיאופורוטי קיים או בנוכחות תולדות של שבר אוסטיאופורוטי; ב. עם T score (ההפרש בין צפיפות העצם של המטופל לבין צפיפות העצם הממוצעת לאדם באוכלוסיה) השווה ל-3.5 או הנמוך מ-3.5- ;ג. בנשים מעל גיל 60 שנים עם T score השווה ל-2.5 או הנמוך מ-2.5- ;ד. שנגרם מאחת המחלות הידועות כגורמות לו; ה. בכל מקרה של אוסטיאופורוזיס שנגרם כתוצאה מטיפול בתכשיר גלוקוקורטיקואידי. 2. למטופלים בכל מקרה של אוסטיאופורוזיס: א. עם שבר אוסטיאופורוטי קיים או בנוכחות תולדות של שבר אוסטיאופורוטי; ב. מעל גיל 60 עם T score השווה ל-2.5 או הנמוך מ-2.5-; ג. בכל מקרה של אוסטיאופורוזיס שנגרם כתוצאה מטיפול בתכשיר גלוקוקורטיקואידי;. ד. שנגרם מאחת המחלות הידועות כגורמות לו; 3. התרופות יינתנו למטופלים ומטופלות בהתאם לחלוקה זו: א. ALENDRONATE SODIUM, RISEDRONATE SODIUM - למטופלים ולמטופלות;ב. RALOXIFENE, BAZEDOXIFENE - למטופלות בלבד.2. אף אחת מן התרופות האמורות לא תינתן בשילוב עם התרופות האחרות.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| ALENDRONATE | ||||
| אוסטיאופורוזיס |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/2000
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
