Quest for the right Drug
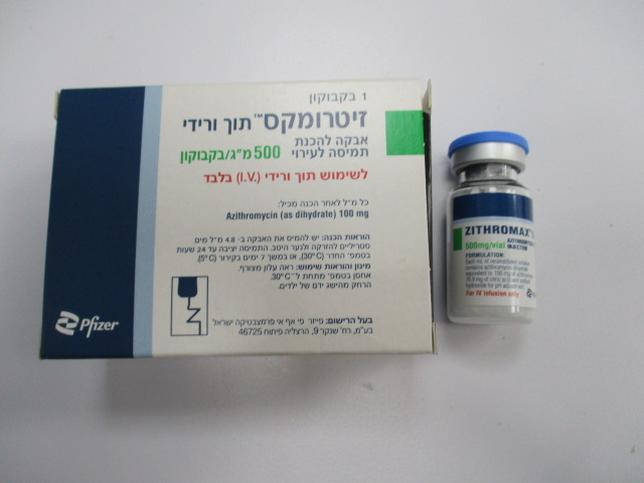
זיטרומקס תוך ורידי ZITHROMAX I.V. (AZITHROMYCIN AS DIHYDRATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה להכנת תמיסה לאינפוזיה : POWDER FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
5 WARNINGS AND PRECAUTIONS 5.1 Hypersensitivity Serious allergic reactions, including angioedema, anaphylaxis, and dermatologic reactions including Acute Generalized Exanthematous Pustulosis (AGEP), Stevens-Johnson Syndrome, and toxic epidermal necrolysis have been reported in patients on azithromycin therapy. [see Contraindications (4.1)] Fatalities have been reported. Cases of Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) have also been reported. Despite initially successful symptomatic treatment of the allergic symptoms, when symptomatic therapy was discontinued, the allergic symptoms recurred soon thereafter in some patients without further azithromycin exposure. These patients required prolonged periods of observation and symptomatic treatment. The relationship of these episodes to the long tissue half-life of azithromycin and subsequent prolonged exposure to antigen is unknown at present. If an allergic reaction occurs, the drug should be discontinued and appropriate therapy should be instituted. Physicians should be aware that the allergic symptoms may reappear after symptomatic therapy has been discontinued. 5.2 Hepatotoxicity Abnormal liver function, hepatitis, cholestatic jaundice, hepatic necrosis, and hepatic failure have been reported, some of which have resulted in death. Discontinue azithromycin immediately if signs and symptoms of hepatitis occur. 5.3 Infantile hypertrophic pyloric stenosis (IHPS) Following the use of azithromycin in neonates (treatment up to 42 days of life), IHPS has been reported. Direct parents and caregivers to contact their physician if vomiting or irritability with feeding occurs. 5.4 QT Prolongation Prolonged cardiac repolarization and QT interval, imparting a risk of developing cardiac arrhythmia and torsades de pointes, have been seen with treatment with macrolides, including azithromycin. Cases of torsades de pointes have been spontaneously reported during postmarketing surveillance in patients receiving azithromycin. Providers should consider the risk of QT prolongation, which can be fatal when weighing the risks and benefits of azithromycin for at-risk groups including: • patients with known prolongation of the QT interval, a history of torsades de pointes, congenital long QT syndrome, bradyarrhythmias or uncompensated heart failure • patients on drugs known to prolong the QT interval • patients with ongoing proarrhythmic conditions such as uncorrected hypokalemia or hypomagnesemia, clinically significant bradycardia, and in patients receiving Class IA (quinidine, procainamide) or Class III (dofetilide, amiodarone, sotalol) antiarrhythmic agents. Elderly patients may be more susceptible to drug-associated effects on the QT interval. 5.5 Cardiovascular Death Some observational studies have shown an approximately two-fold increased short-term potential risk of acute cardiovascular death in adults exposed to azithromycin relative to other antibacterial drugs, including amoxicillin. The five- day cardiovascular mortality observed in these studies ranged from 20 to 400 per million azithromycin treatment courses. This potential risk was noted to be greater during the first five days of azithromycin use and does not appear to be limited to those patients with preexisting cardiovascular diseases. The data in these observational studies are insufficient to establish or exclude a causal relationship between acute cardiovascular death and azithromycin use. Consider balancing this potential risk with treatment benefits when prescribing ZITHROMAX. 5.6 Clostridium difficile-Associated Diarrhea Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including ZITHROMAX® I.V., and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile. C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antibacterial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibacterial use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents. If CDAD is suspected or confirmed, ongoing antibacterial use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated. 5.7 Exacerbation of Myasthenia Gravis Exacerbations of symptoms of myasthenia gravis and new onset of myasthenic syndrome have been reported in patients receiving azithromycin therapy. 5.8 Infusion Site Reactions ZITHROMAX® I.V. for injection should be reconstituted and diluted as directed and administered as an intravenous infusion over not less than 60 minutes. [see Dosage and Administration (2)] Local IV site reactions have been reported with the intravenous administration of azithromycin. The incidence and severity of these reactions were the same when 500 mg azithromycin was given over 1 hour (2 mg/mL as 250 mL infusion) or over 3 hr (1 mg/mL as 500 mL infusion) [see Adverse Reactions (6)]. All volunteers who received infusate concentrations above 2.0 mg/mL experienced local IV site reactions and, therefore, higher concentrations should be avoided. 5.9 Development of Drug-Resistant Bacteria Prescribing ZITHROMAX® I.V. in the absence of a proven or strongly suspected bacterial infection is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria. 6 ADVERSE REACTIONS The following clinically significant adverse reactions are described elsewhere in labeling: • Hypersensitivity [see Warnings and Precautions (5.1)] • Hepatotoxicity [see Warnings and Precautions (5.2)] • Infantile Hypertrophic Pyloric Stenosis (IHPS) [see Warnings and Precautions (5.3)] • QT Prolongation [see Warnings and Precautions (5.4)] • Cardiovascular Death [see Warnings and Precautions (5.5)] • Clostridioides difficile-Associated Diarrhea (CDAD) [see Warnings and Precautions (5.6)] • Exacerbation of Myasthenia Gravis [see Warnings and Precautions (5.7) 6.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. In clinical trials of intravenous azithromycin for community-acquired pneumonia, in which 2 to 5 IV doses were given, the reported adverse reactions were mild to moderate in severity and were reversible upon discontinuation of the drug. The majority of patients in these trials had one or more co-morbid diseases and were receiving concomitant medications. Approximately 1.2% of the patients discontinued intravenous ZITHROMAX® I.V. therapy, and a total of 2.4% discontinued azithromycin therapy by either the intravenous or oral route because of clinical or laboratory side effects. In clinical trials conducted in patients with pelvic inflammatory disease, in which 1 to 2 IV doses were given, 2% of women who received monotherapy with azithromycin and 4% who received azithromycin plus metronidazole discontinued therapy due to clinical side effects. Clinical adverse reactions leading to discontinuations from these studies were gastrointestinal (abdominal pain, nausea, vomiting, diarrhea), and rashes; laboratory side effects leading to discontinuation were increases in transaminase levels and/or alkaline phosphatase levels. Overall, the most common adverse reactions associated with treatment in adult patients who received ZITHROMAX® I.V. in studies of community-acquired pneumonia were related to the gastrointestinal system with diarrhea/loose stools (4.3%), nausea (3.9%), abdominal pain (2.7%), and vomiting (1.4%) being the most frequently reported. Approximately 12% of patients experienced a side effect related to the intravenous infusion; most common were pain at the injection site (6.5%) and local inflammation (3.1%). The most common adverse reactions associated with treatment in adult women who received ZITHROMAX® I.V. in trials of pelvic inflammatory disease were related to the gastrointestinal system. Diarrhea (8.5%) and nausea (6.6%) were most commonly reported, followed by vaginitis (2.8%), abdominal pain (1.9%), anorexia (1.9%), rash and pruritus (1.9%). When azithromycin was co-administered with metronidazole in these trials, a higher proportion of women experienced adverse reactions of nausea (10.3%), abdominal pain (3.7%), vomiting (2.8%), infusion site reaction, stomatitis, dizziness, or dyspnea (all at 1.9%). Adverse reactions that occurred with a frequency of 1% or less included the following: Gastrointestinal: Dyspepsia, flatulence, mucositis, oral moniliasis, and gastritis. Nervous system: Headache, somnolence. Allergic: Bronchospasm. Special senses: Taste perversion. Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il 6.2 Postmarketing Experience The following adverse reactions have been identified during post-approval use of azithromycin. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Adverse reactions reported with azithromycin during the post-marketing period in adult and/or pediatric patients for which a causal relationship may not be established include: Allergic: Arthralgia, edema, urticaria and angioedema. Cardiovascular: Arrhythmias including ventricular tachycardia and hypotension. There have been reports of QT prolongation and torsade's de pointes, and cardiovascular death. Gastrointestinal: Anorexia, constipation, dyspepsia, flatulence, vomiting/diarrhea, pseudomembranous colitis, pancreatitis, oral candidiasis, pyloric stenosis, and reports of tongue discoloration. General: Asthenia, paresthesia, fatigue, malaise and anaphylaxis (including fatalities). Genitourinary: Interstitial nephritis and acute renal failure and vaginitis. Hematopoietic: Thrombocytopenia. Liver/biliary: Abnormal liver function, hepatitis, cholestatic jaundice, hepatic necrosis, and hepatic failure. [see Warnings and Precautions (5.2)] Nervous system: Convulsions, dizziness/vertigo, headache, somnolence, hyperactivity, nervousness, agitation and syncope. Psychiatric: Aggressive reaction and anxiety. Skin/appendages: Pruritus, serious skin reactions including, erythema multiforme, AGEP, Stevens-Johnson syndrome, toxic epidermal necrolysis, and DRESS. Special senses: Hearing disturbances including hearing loss, deafness and/or tinnitus and reports of taste/smell perversion and/or loss. 6.3 Laboratory Abnormalities Significant abnormalities (irrespective of drug relationship) occurring during the clinical trials were reported as follows: • elevated ALT (SGPT), AST (SGOT), creatinine (4 to 6%) • elevated LDH, bilirubin (1 to 3%) • leukopenia, neutropenia, decreased platelet count, and elevated serum alkaline phosphatase (less than 1%) When follow-up was provided, changes in laboratory tests appeared to be reversible. In multiple-dose clinical trials involving more than 750 patients treated with ZITHROMAX® I.V., less than 2% of patients discontinued azithromycin therapy because of treatment-related liver enzyme abnormalities.
Effects on Driving

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
