Quest for the right Drug
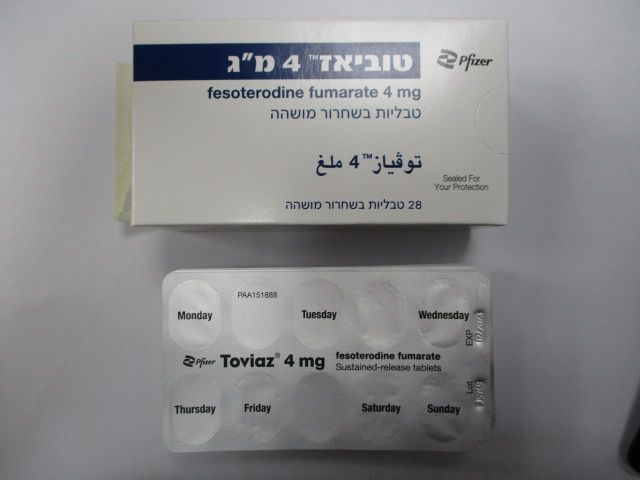
טוביאז 4 מ"ג TOVIAZ 4 MG (FESOTERODINE FUMARATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות עם שחרור מושהה : TABLETS SUSTAINED RELEASE
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Urologicals, Urinary antispasmodics, ATC code: G04BD11. Mechanism of action Fesoterodine is a competitive, specific muscarinic receptor antagonist. It is rapidly and extensively hydrolysed by non-specific plasma esterases to the 5-hydroxymethyl derivative, its primary active metabolite, which is the main active pharmacological principle of fesoterodine. Clinical efficacy and safety The efficacy of fixed doses of fesoterodine 4 mg and 8 mg was evaluated in two Phase 3 randomised, double-blind, placebo-controlled, 12-week studies. Female (79%) and male (21%) patients with a mean age of 58 years (range 19-91 years) were included. A total of 33% of patients were ≥65 years of age and 11% were ≥75 years of age. Fesoterodine treated patients had statistically significant mean reductions in the number of micturitions per 24 hours and in the number of urge incontinence episodes per 24 hours at the end of treatment compared to placebo. Likewise, the response rate (% of patients reporting that their condition has been “greatly improved” or “improved” using a 4-point Treatment Benefit Scale) was significantly greater with fesoterodine compared to placebo. Furthermore, fesoterodine improved the mean change in the voided volume per micturition, and the mean change in the number of continent days per week (see Table 1 below). Table 1: Mean changes from Baseline to end of treatment for primary and selected secondary endpoints Study 1 Study 2 Parameter Placebo Fesoterodine Fesoterodine Active Placebo Fesoterodine Fesoterodine 4 mg 8 mg comparator 4 mg 8 mg Number of micturitions per 24 hours# N=279 N=265 N=276 N=283 N=266 N=267 N=267 Baseline 12.0 11.6 11.9 11.5 12.2 12.9 12.0 Change from -1.02 -1.74 -1.94 -1.69 -1.02 -1.86 -1.94 baseline p-value <0.001 <0.001 0.032 <0.001 Responder rate (treatment response)# N=279 N=265 N=276 N=283 N=266 N=267 N=267 Responder rate 53.4% 74.7% 79.0% 72.4% 45.1% 63.7% 74.2% p-value <0.001 <0.001 <0.001 <0.001 Number of urge incontinence episodes per 24 hours N=211 N=199 N=223 N=223 N=205 N=228 N=218 Baseline 3.7 3.8 3.7 3.8 3.7 3.9 3.9 Change from -1.20 -2.06 -2.27 -1.83 -1.00 -1.77 -2.42 baseline p-value 0.001 <0.001 0.003 <0.001 Number of continent days per week N=211 N=199 N=223 N=223 N=205 N=228 N=218 Baseline 0.8 0.8 0.6 0.6 0.6 0.7 0.7 Change from 2.1 2.8 3.4 2.5 1.4 2.4 2.8 baseline p-value 0.007 <0.001 <0.001 <0.001 Voided volume per micturition (ml) N=279 N=265 N=276 N=283 N=266 N=267 N=267 Baseline 150 160 154 154 159 152 156 Change from 10 27 33 24 8 17 33 baseline p-value <0.001 <0.001 0.150 <0.001 # primary end points Cardiac electrophysiology The effect of fesoterodine 4 mg and 28 mg on the QT interval was thoroughly evaluated in a double-blind, randomised, placebo- and positive-controlled (moxifloxacin 400 mg) parallel group study with once-daily treatment over a period of 3 days in 261 male and female subjects aged 45 to 65 years. Change from baseline in QTc based on the Fridericia correction method did not show any differences between the active treatment and placebo group.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption After oral administration, due to rapid and extensive hydrolysis by non-specific plasma esterases, fesoterodine was not detected in plasma. Bioavailability of the active metabolite is 52%. After single or multiple-dose oral administration of fesoterodine in doses from 4 mg to 28 mg, plasma concentrations of the active metabolite are proportional to the dose. Maximum plasma levels are reached after approximately 5 hours. Therapeutic plasma levels are achieved after the first administration of fesoterodine. No accumulation occurs after multiple-dose administration. Distribution Plasma protein binding of the active metabolite is low with approximately 50% bound to albumin and alpha-1-acid glycoprotein. The mean steady-state volume of distribution following intravenous infusion of the active metabolite is 169 l. Biotransformation After oral administration, fesoterodine is rapidly and extensively hydrolysed to its active metabolite. The active metabolite is further metabolised in the liver to its carboxy, carboxy-N-desisopropyl, and N- desisopropyl metabolite with involvement of CYP2D6 and CYP3A4. None of these metabolites contribute significantly to the antimuscarinic activity of fesoterodine. Mean Cmax and AUC of the active metabolite are 1.7 and 2-fold higher, respectively, in CYP2D6 poor metabolisers as compared to extensive metabolisers. Elimination Hepatic metabolism and renal excretion contribute significantly to the elimination of the active metabolite. After oral administration of fesoterodine, approximately 70% of the administered dose was recovered in urine as the active metabolite (16%), carboxy metabolite (34%), carboxy-N-desisopropyl metabolite (18%), or N-desisopropyl metabolite (1%), and a smaller amount (7%) was recovered in faeces. The terminal half- life of the active metabolite following oral administration is approximately 7 hours and is absorption rate- limited. Age and gender No dose adjustment is recommended in these subpopulations. The pharmacokinetics of fesoterodine are not significantly influenced by age and gender. Paediatric population The pharmacokinetics of fesoterodine have not been evaluated in paediatric patients. Renal impairment In patients with mild or moderate renal impairment (GFR 30 – 80 ml/min), Cmax and AUC of the active metabolite increased up to 1.5 and 1.8-fold, respectively, as compared to healthy subjects. In patients with severe renal impairment (GFR < 30 ml/min), Cmax and AUC are increased 2.0 and 2.3-fold, respectively. Hepatic impairment In patients with moderate hepatic impairment (Child Pugh B), Cmax and AUC of the active metabolite increased 1.4 and 2.1-fold, respectively, as compared to healthy subjects. Pharmacokinetics of fesoterodine in patients with severe hepatic impairment have not been studied.

מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| לטיפול בשלפחות שתן פעילה ביתר | FESOTERODINE, SOLIFENACIN, TOLTERODINE, TROSPIUM |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
23/01/2011
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
