Quest for the right Drug
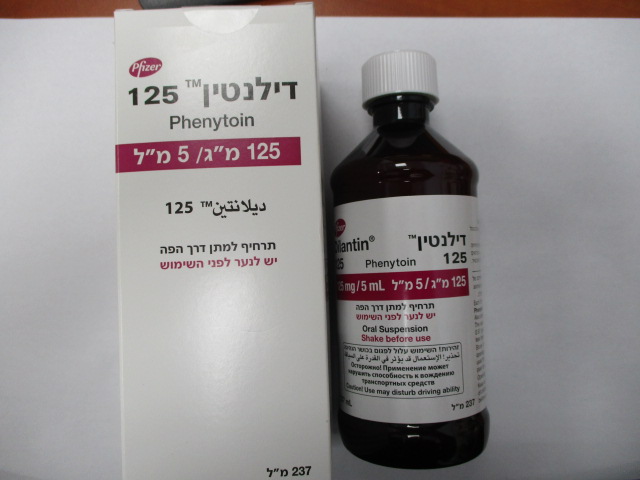
דילנטין 125 DILANTIN 125 (PHENYTOIN)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
תרחיף : SUSPENSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
12.1 Mechanism of Action The precise mechanism by which phenytoin exerts its therapeutic effect has not been established but is thought to involve the voltage-dependent blockade of membrane sodium channels resulting in a reduction in sustained high-frequency neuronal discharges.
Pharmacokinetic Properties
12.2 Pharmacokinetics AbsorptionFor Dilantin, peak levels occur 1½ to 3 hours after administration. Steady-state therapeutic levels are achieved at least 7 to 10 days (5 to 7 half-lives) after initiation of therapy with recommended doses of 300 mg/day. When serum level determinations are necessary, they should be obtained at least 5 to 7 half-lives after treatment initiation, dosage change, or addition or subtraction of another drug to the regimen so that equilibrium or steady-state will have been achieved. Distribution Phenytoin is extensively bound to serum plasma proteins. Elimination The plasma half-life in man after oral administration of phenytoin averages 22 hours, with a range of 7 to 42 hours. Metabolism Phenytoin is primarily metabolized by the hepatic cytochrome P450 enzyme CYP2C9 and to a lesser extent by CYP2C19. Because phenytoin is hydroxylated in the liver by an enzyme system which is saturable at high serum levels, small incremental doses may increase the half-life and produce very substantial increases in serum levels, when these are in the upper range. The steady-state level may be disproportionately increased, with resultant intoxication, from an increase in dosage of 10% or more. In most patients maintained at a steady dosage, stable phenytoin serum levels are achieved. There may be wide interpatient variability in phenytoin serum levels with equivalent dosages. Patients with unusually low levels may be noncompliant or hypermetabolizers of phenytoin. Unusually high levels result from liver disease, variant CYP2C9 and CYP2C19 alleles, or drug interactions which result in metabolic interference. The patient with large variations in phenytoin serum levels, despite standard doses, presents a difficult clinical problem. Serum level determinations in such patients may be particularly helpful. As phenytoin is highly protein bound, free phenytoin levels may be altered in patients whose protein binding characteristics differ from normal. Excretion Most of the drug is excreted in the bile as inactive metabolites which are then reabsorbed from the intestinal tract and excreted in the urine. Urinary excretion of phenytoin and its metabolites occurs partly with glomerular filtration but, more importantly, by tubular secretion. Specific Populations Age: Geriatric Population: Phenytoin clearance tends to decrease with increasing age (20% less in patients over 70 years of age relative to that in patients 20 to 30 years of age). Since phenytoin clearance is decreased slightly in elderly patients, lower or less frequent dosing may be required [see Dosage and Administration (2)]. Sex/Race: Gender and race have no significant impact on phenytoin pharmacokinetics. Renal or Hepatic Impairment: Increased fraction of unbound phenytoin in patients with renal or hepatic disease, or in those with hypoalbuminemia has been reported. Pregnancy: It has been reported in the literature that the plasma clearance of phenytoin generally increased during pregnancy, reached a peak in the third trimester and returned to the level of pre-pregnancy after few weeks or months of delivery. Drug Interaction Studies Phenytoin is primarily metabolized by the hepatic cytochrome P450 enzyme CYP2C9 and to a lesser extent by CYP2C19. Phenytoin is a potent inducer of hepatic drug-metabolizing enzymes [see Drug Interactions (7.1, 7.2)]. 12.5 Pharmacogenomics CYP2C9 activity is decreased in individuals with genetic variants such as the CYP2C9*2 and CYP2C9*3 alleles. Carriers of variant alleles, resulting in intermediate (e.g., *1/*3, *2/*2) or poor metabolism (e.g., *2/*3, *3/*3) have decreased clearance of phenytoin. Other decreased or nonfunctional CYP2C9 alleles may also result in decreased clearance of phenytoin (e.g., *5, *6, *8, *11). The prevalence of the CYP2C9 poor metabolizer phenotype is approximately 2-3% in the White population, 0.5- 4% in the Asian population, and <1% in the African American population. The CYP2C9 intermediate phenotype prevalence is approximately 35% in the White population, 24% in the African American population, and 15-36% in the Asian population [see Warnings and Precautions (5.3) and Use in Specific Populations (8.7)].

שימוש לפי פנקס קופ''ח כללית 1994
Grand mal & psychomotor seizures, trigeminal neuralgia
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
עלון מידע לרופא
31.05.22 - עלון לרופאעלון מידע לצרכן
04.01.16 - עלון לצרכן 24.02.16 - עלון לצרכן 16.08.20 - עלון לצרכן אנגלית 31.05.22 - עלון לצרכן אנגלית 31.05.22 - עלון לצרכן עברית 16.08.20 - עלון לצרכן ערבית 31.05.22 - עלון לצרכן ערבית 28.02.12 - החמרה לעלון 06.05.12 - החמרה לעלון 17.11.14 - החמרה לעלון 13.06.21 - החמרה לעלון 18.04.22 - החמרה לעלוןלתרופה במאגר משרד הבריאות
דילנטין 125