Quest for the right Drug
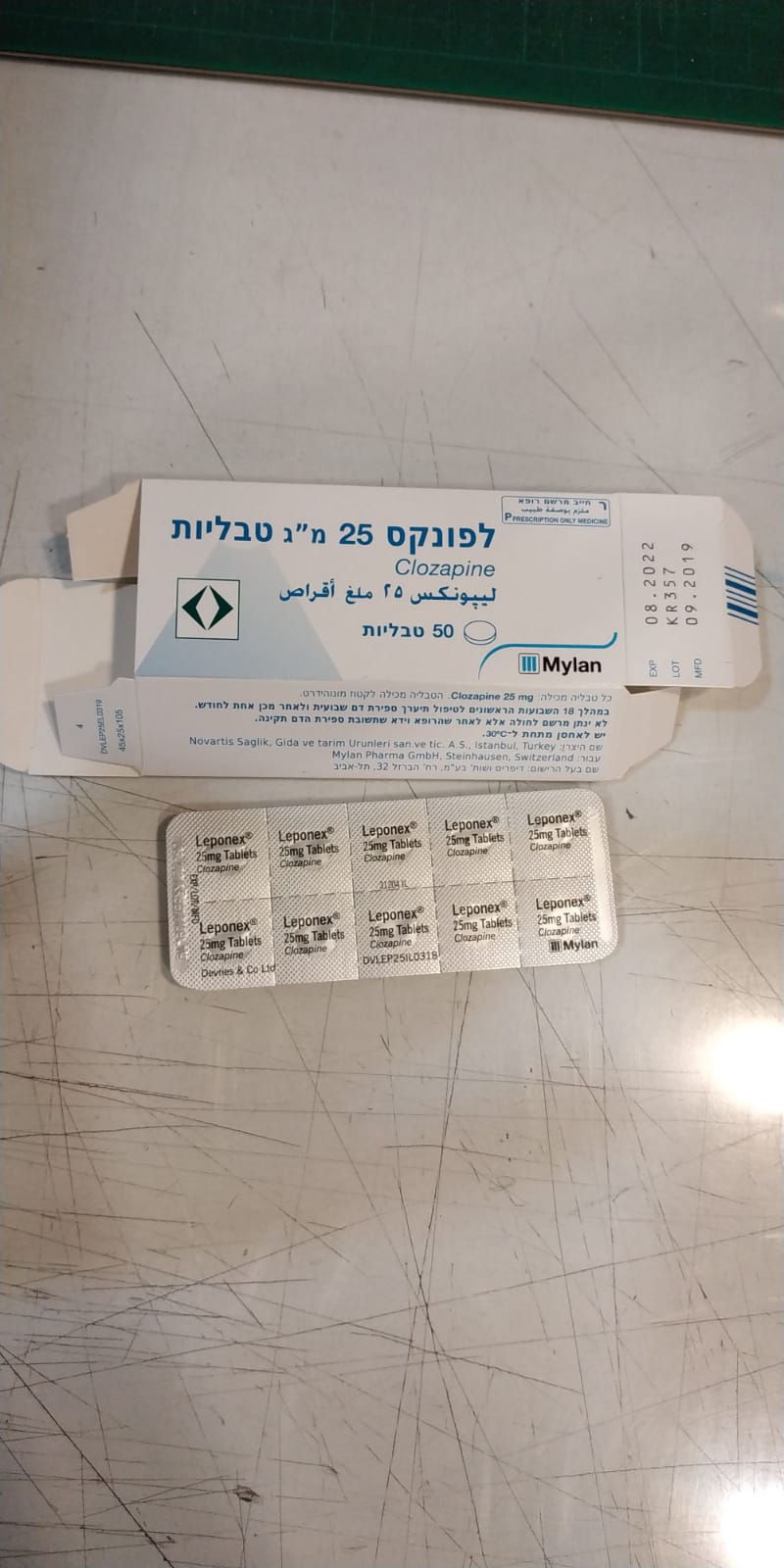
לפונקס 25 מ"ג טבליות LEPONEX 25 MG TABLETS (CLOZAPINE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Posology : מינונים
4.2 Posology and method of administration Posology/Administration The dosage must be adjusted individually. For each patient, the lowest effective dose should be used. Cautious titration and a divided dosage regimen are necessary to minimise the risk of hypotension, seizures and sedation. The total daily amount may be divided into unequal doses, the largest of which should be taken at bedtime. Prior to initiating treatment with clozapine tablets, a baseline ANC must be at least 2,000 per mm3 for the general population; and must be at least 1,500 per mm3 for patients with documented Benign Ethnic Neutropenia (BEN). Dose adjustment is indicated in patients who are also receiving medicinal products that have pharmacokinetic interactions with Leponex, such as benzodiazepines, carbamazepine or selective serotonin re-uptake inhibitors (see “Interactions”). Prescribing physicians should comply fully with the required safety measures. At each consultation, a patient receiving Leponex should be reminded to contact the treating physician immediately if any kind of infection begins to develop. Particular attention should be paid to flu-like complaints such as fever or sore throat and to other evidence of infection, which may be indicative of neutropenia (see “Warnings and precautions”). Patients and their caregivers must be informed that, in the event of any of these symptoms, they must have a blood cell count performed immediately. Method of Administration Leponex is administered orally. Prerequisite actions and tests before starting treatment 1. Medical examination, including a comprehensive psychiatric evaluation. • If the patient is a minor, the psychiatric evaluation must be performed by a pediatric psychiatrist. Additionally, the primary physician (pediatrician, family physician, community internist) must also perform a comprehensive examination. 2. Requisite baseline tests • Electrocardiogram (ECG) – including QTc interval. • Metabolic indicators – weight, BMI, blood pressure, level of fats in blood, level of lipids, fasting blood glucose, HbBA1C, complete blood count, including a differential blood count and platelets. • Kidney function and liver function. 3. The requisite baseline tests must be performed within a maximum of 10 days prior to the initial dispensing of the medicine. 4. The treating psychiatrist must explain the proposed integrated therapy program to the patient and instruct the patient to report any febrile illness or throat inflammation to the treating physician, since it will then become necessary to verify with an updated complete blood count (hereinafter: CBC) that there has been no drop in white blood cells. 5. It is recommended that, upon the initial treatment attempt with clozapine, all other antipsychotic medicines that the patient is taking should be gradually discontinued (clozapine monotherapy). Course of treatment A repeat prescription for clozapine may be issued by a treating psychiatrist or by a primary physician (family physician or pediatrician, community internist), provided that psychiatric monitoring is concurrently maintained. The clinical situation should be monitored monthly by a psychiatrist until the optimal dosage is reached. Requisite supervision and the dispensing of prescriptions 1. Leponex will be provided in community pharmacies or hospitals. 2. The first prescription (initiation of treatment) shall be dispensed only if the prescription was issued by a psychiatrist, and within a maximum of 10 days after the performance of the blood count. 3. The medicinal product shall be dispensed only according to a prescription that also specifies, in addition to the regular details, the following details (structurally, manually or as physically or digitally stamped): a. Confirmation that the blood count is normal, including the date of performance; b. Start date of the treatment with clozapine; c. Name of the examining physician. 4. During the first 18 weeks of treatment, the medicinal product shall be dispensed solely for one week of treatment. As of week 19 of the treatment, the medicinal product shall be dispensed solely for one month of treatment. 5. If treatment with clozapine is initiated during hospitalization – supervision and administration of the medicinal product will be performed by the hospital ward and, upon the patient’s discharge, the supervision must be continued in the community. It is important to inform primary physicians about the treatment with clozapine and about the stage of supervision. 6. If treatment is initiated in the community (mental health clinic, psychiatric stabilizing facility, home hospitalization, etc.), the supervision and administration of the medicinal product will be performed in that framework. Inform primary physicians about the treatment and supervision. 7. During the first 18 weeks of treatment, the psychiatrist must perform weekly monitoring of the CBC and issue the weekly prescriptions accordingly. If a psychiatrist is unavailable, the family physician or pediatrician or community internist may perform the monitoring of the CBC and issue the prescription, in coordination with and according to the instructions of the psychiatrist. The treating physician must be informed of the blood test results within 48 hours. The supervision and clinical monitoring of the efficacy and safety of the patient’s treatment must be performed at least once a month by the psychiatrist. 8. Subsequent to the first 18 weeks of treatment, the monthly prescription must be issued by a psychiatrist, subject to the results of the CBC that was taken not more than seven days earlier. If a psychiatrist is unavailable, a family physician or pediatrician may issue the prescription, in coordination with and according to the instructions of the psychiatrist. The supervision and clinical monitoring of the efficacy and safety of the patient’s treatment must be performed at least once every 3 months by the psychiatrist. Table 1: Summary table of requisite monitoring Test Basic First 18 weeks After 6 Follow up after 1 year After 1 After 3 months month months CBC X Every week, later-on every month every month every month Glucose in fast X X X Once a year HbA1C X X Once a year Lipids (cholesterol X X Once a year and triglycerides) Blood chemistry X X X Once a year ECG including QTc Every 2 months in the first X Once a year interval 4 months Constipation X Every week X Once a year monitoring BMI X X Once a year Blood pressure and X X X X Once a year pulse Travel abroad 1. Due to the need to constantly monitor anyone taking this medicine, the patient must consult with the treating physician before booking the trip, in order to properly prepare for this. 2. The length of the vacation should be restricted according to the dates of performance of the requisite tests. 3. If a patient needs to be absent from Israel for a prolonged period, the patient must organize a schedule of tests and prescriptions at his destination, while coordinating in advance with the treating physician in the destination country. Treatment-resistant schizophrenia Starting therapy Leponex should be started with 12.5 mg (half a 25 mg tablet) once or twice on the first day, followed by one or two 25 mg tablets on the second day. If well tolerated, the daily dose may then be increased slowly in increments of 25 mg to 50 mg in order to achieve a dose level of up to 300 mg/day within few weeks. Thereafter, if required, the daily dose may be further increased in increments of 50 mg to 100 mg at half-weekly or, preferably, weekly intervals. A lower starting dose and slower dose increases are recommended for patients with a history of seizures or with cardiovascular, renal or hepatic disorders. For children and adolescents, begin at a dosage of 12.5 mg and gradually increase the dosage at a pace of 25 mg every 3 to 5 days, depending upon tolerance. Therapeutic dose range In most patients, antipsychotic efficacy can be expected with 300 to 450 mg/day given in divided doses. Some patients may be treated with lower doses, and some patients may require doses up to 600 mg/day. The total daily dose may be divided unevenly, with the larger portion being taken at bedtime. The usual daily dose in the population of children and adolescents is in the range 125 to 475 mg. It is recommended to reach a suitable dosage within a number of weeks, usually 300 mg per 24 hours, and to remain at this dosage for a number of weeks until clinical improvement is reached (if it is not possible to measure the clozapine levels in the blood) and/or until the appearance of side effects: • Male smokers: 400-500 mg per 24 hours. • Male non-smokers: 300-400 mg per 24 hours. • Female smokers: 300-400 mg per 24 hours. • Female non-smokers: 200-300 mg per 24 hours. Nicotine per se does not affect the level of clozapine in the blood. Therefore, if electronic cigarettes or nicotine substitutes are used, there is no need to adjust the dosage. The timeframe until there is a therapeutic response may be prolonged in some patients. Wait 6 months under optimal treatment before assessing the response to the medicine, because patients who showed no clinical response during the first three months, sometimes showed a Delayed response, within a timeframe of 3-6 months. Maximum dose To obtain full therapeutic benefit, a few patients may require larger doses, in which case judicious increments (not exceeding 100 mg) are permissible up to 900 mg/day. However, the possibility of increased adverse reactions (in particular seizures) occurring at doses over 450 mg/day must be borne in mind (the reason for reaching this dose should be documented). If the level exceeds the maximum level in the blood of 600 ng/ml, consider, according to the clinical situation, reducing the dosage and/or adding an anticonvulsant medicinal product. Factors that could alter the medicine level in the blood: • A febrile illness raises the level of the medicine and could cause poisoning. • Smoking lowers the level of the medicine in the blood. • A sudden stop in smoking could increase the level of the medicine in the blood. A psychiatrist must monitor the clinical situation once a month until the optimal dosage is reached. Maintenance dose After achieving maximum therapeutic benefit, many patients can be maintained effectively on lower doses. Careful downward titration is therefore recommended. Treatment should be maintained for at least 6 months. If the daily dose does not exceed 200 mg, once daily administration in the evening may be appropriate. Ending therapy In the event of planned termination of Leponex therapy, a gradual reduction in dose over a 1- to 2-week period is recommended. If abrupt discontinuation is necessary (e.g. because of leucopenia), the patient should be carefully observed for the recurrence of psychotic symptoms and symptoms related to cholinergic rebound (see “Warnings and precautions”). (e.g. increased sweating, headache, nausea, vomiting and diarrhoea). Re-starting therapy In patients in whom the interval since the last dose of Leponex exceeds 2 days, treatment should be re-initiated with 12.5 mg (half a 25 mg tablet) given once or twice on the first day. If this dose is well tolerated, it may be feasible to titrate the dose to the therapeutic level more quickly than is recommended for initial treatment. However, in any patient who has previously experienced respiratory or cardiac arrest with initial dosing (see “Warnings and precautions”), but was then able to be successfully titrated to a therapeutic dose, re-titration should be done with extreme caution. Even for a patient who already proceeded to monthly CBCs after completing 18 weeks of weekly CBCs, increasing the dosage of the medicine once again requires at least 6 weeks of weekly CBCs after completing the increase in dosage. Subsequently, the monitoring can return to the frequency prior to the discontinuation. If clozapine was discontinued for more than one month, initiate monitoring as if restarting the treatment. Switching from a previous antipsychotic therapy to Leponex It is generally recommended that Leponex should not be used in combination with other antipsychotics. When Leponex therapy is to be initiated in a patient undergoing oral antipsychotic therapy, it is recommended that the dosage of other antipsychotics be reduced or discontinued by gradually tapering it downwards. Based on the clinical circumstances, the prescribing physician should judge whether or not to discontinue the other antipsychotic therapy before initiating treatment with Leponex. Combination treatment with ECT In acute cases of schizophrenia that are resistant to clozapine therapy, electroconvulsive therapy (ECT) may be added. A number of controlled studies and also a meta-analysis have shown benefit in adding ECT for some patients who did not respond adequately to clozapine alone. Before deciding to administer ECT, it is advisable to verify that the clozapine level in the blood is within the therapeutic range. In the event that ECT is added, reducing the clozapine dosage may be considered. Reducing the risk of suicidal behaviour in schizophrenia and schizoaffective disorder The dosage and administration recommendations described in the preceding section (Dosage and administration) regarding the use of Leponex in patients with treatment-resistant schizophrenia should also be followed when treating patients with schizophrenia or schizoaffective disorder at risk for recurrent suicidal behaviour. A course of treatment with Leponex of at least two years is recommended in order to maintain the reduction of risk for suicidal behaviour. It is recommended that the patient’s risk of suicidal behaviour be reassessed after two years of treatment and that thereafter the decision to continue treatment with Leponex be re-visited at regular intervals, based on thorough assessments of patient’s risk for suicidal behaviour during treatment. Special Populations Cardiovascular disorders In patients suffering from cardiovascular disorders (note: severe cardiovascular disorders are contraindications) the initial dose should be 12.5 mg given once on the first day, and dosage increase should be slow and in small increments. Renal impairment In patients with mild to moderate renal impairment the initial dose should be 12.5 mg given once on the first day, and dosage increase should be slow and in small increments. Hepatic impairment Patients with hepatic impairment should receive Leponex with caution along with regular monitoring of liver function tests (see “Warnings and precautions”). Pediatrics No pediatric studies have been performed. The safety and efficacy of Leponex in children and adolescents under the age of 16 have not been established. Patients 60 years of age and older It is recommended that treatment in patients 60 years and older is initiated at a particularly low dose (12.5 mg given once on the first day) with subsequent dose increments restricted to 25 mg/day. Measuring the clozapine level in the blood 1. Determining the medicine level in a patient’s blood enables the physician to ascertain whether the medicinal product is indeed within the effective therapeutic range, to avoid prescribing an unnecessarily high dosage, to examine treatment adherence and to detect resistant cases in which another increase in dosage is warranted. Determining the level is particularly important in instances when patients are taking a number of medicines, some of which might have a pharmacokinetic interaction with clozapine. 2. It is recommended to check the clozapine level in the blood 4-6 days after reaching the target dosage. It is advisable to take the sample about 12 hours after the latest dose is taken. 3. The recommended therapeutic level is within the range of 350 ng/ml and up to 600 ng/ml. 4. Factors affecting the medicine level in the blood: • Clozapine is metabolized in the liver (mainly cytochrome A21 and some A43) into two metabolites, with only one of them being active (norclozapine). The level of clozapine in the blood is influenced by medicinal products that affect these cytochromes (such as fluvoxamine, TCAs and cimetidine). • The level of the medicinal product in the blood is also influenced by gender (females metabolize less) and age (young people metabolize more), BMI, the genetics of metabolism, smoking, diet and more. 5. It is recommended to measure the level of clozapine in the blood throughout the treatment with clozapine in the following instances: • Inadequate clinical response to the treatment at a dosage of between 400 and 600 mg. • When unexpected side effects (such as a seizure) appear. • If a patient changed his/her smoking habits during the treatment. • After adding another medicine to the therapy that could affect the clozapine levels, such as fluvoxamine, TCAs (Tricyclic antidepressants), cimetidine. • Patients after bariatric surgery. • When the patient has pneumonia or other significant infection • In the appearance of symptoms suspicious of poisoning 6. Additional emphases about the need for measuring the level of the medicine in the blood: • When the clinical response at a dosage of up to 600 ng/ml is inadequate, the dosage may be gradually increased up to the level of 1,000 ng/ml, while monitoring the side effects.

שימוש לפי פנקס קופ''ח כללית 1994
Schizophrenia in patients unresponsive to or intolerant of conventional antipsychotic drugs. התרופה תימצא רק בבתי חולים ותנופק לחולים אמבולטורים רק באמצעותם
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה אשפוזית לפי החלטת משרד הבריאות
מידע נוסף
