Quest for the right Drug
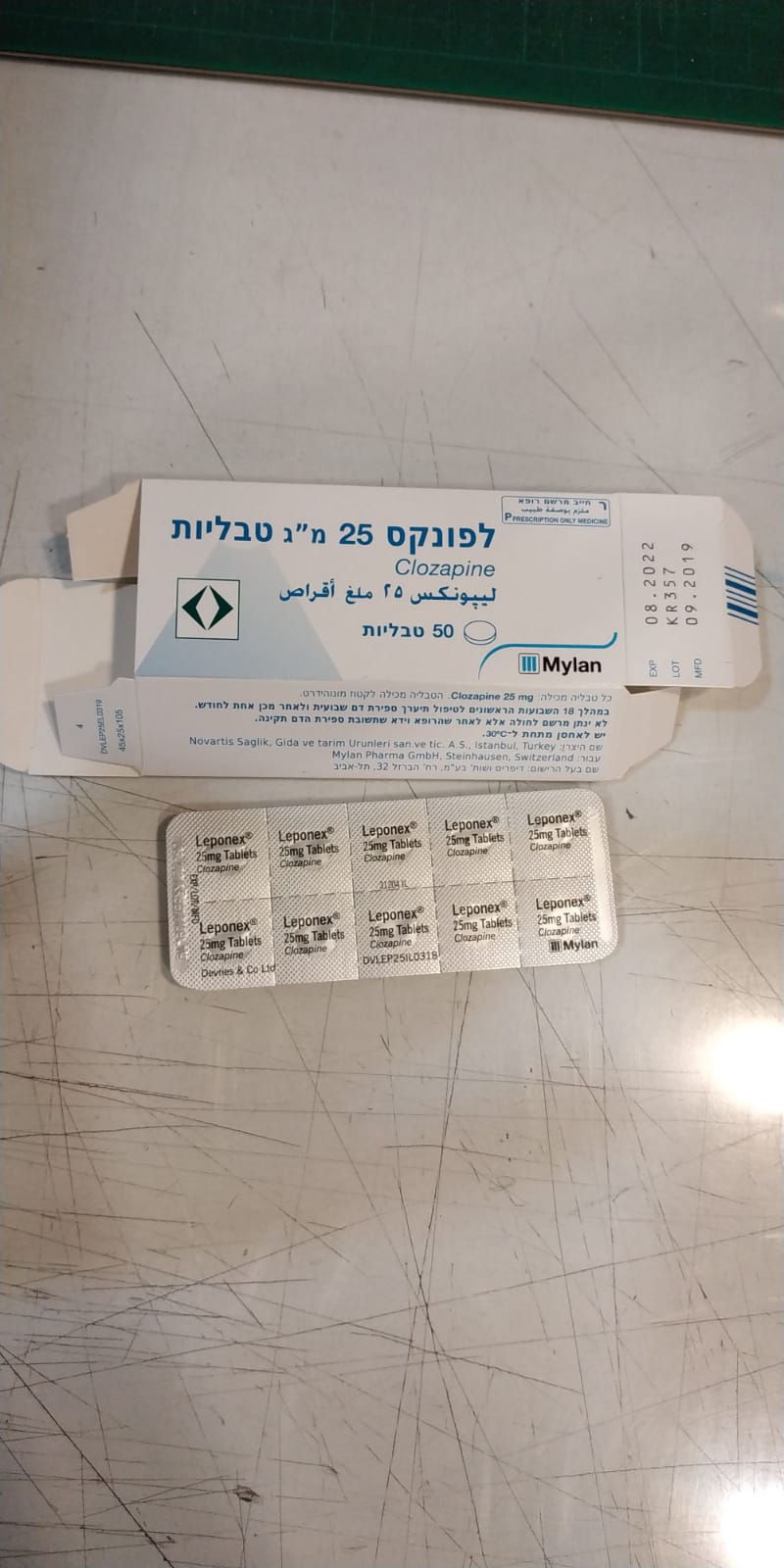
לפונקס 25 מ"ג טבליות LEPONEX 25 MG TABLETS (CLOZAPINE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
Warnings Potentially severe adverse effects of Leponex therapy are granulocytopenia and agranulocytosis, which occur with an estimated frequency of 3% and 0.7%, respectively. Agranulocytosis can be life-threatening. Agranulocytosis Agranulocytosis is defined as a drop in the number of neutrophils below 1,000 per mm3. The cumulative incidence of agranulocytosis is about 1% and the reported mortality ratio (as a result of infection) ranges between 0.1% and 0.3%. When the level of neutrophils is below 500 per mm3, the immune-resistance becomes very low, resulting in an increased risk of a lethal infection (in the instance of Benign Ethnic Neutropenia – BEN, below 500 per mm3). The prevalence of the effect varies depending upon the duration of the treatment. Most cases will appear during the first 18 weeks of treatment, but there have also been instances when the effect occurred later on. In patients with no BEN diagnosis, if ANC count falls to between 1,000 and 1,500 per mm3, haematological monitoring should be performed 3 times a week until value rises above 1,500 per mm3. If ANC count falls between 500 and 999 per mm3, clozapine is to be discontinued and haematological monitoring should be performed daily until value rises above 1,000 per mm3. Once neutrophils rise back above 1,000 per mm3, treatment with clozapine may be resumed, with monitoring 3 times a week until the level reaches 1,500 per mm3. If ANC count falls below 500 mm3, clozapine is to be discontinued immediately and haematological monitoring should be performed daily until value rises above 1,000 per mm3. In any case, do not restart treatment (rechallenge) until neutrophils return to a value of at least 1,500 per mm3 and consult with a hematologist. In patients with a BEN diagnosis, if ANC count falls to between 500 and 999 per mm3, haematological monitoring should be performed 3 times a week until value rises above 1,000 per mm3. If ANC count falls below 500 mm3, clozapine is to be discontinued immediately and haematological monitoring should be performed daily until value rises above 500 per mm3. In any case, do not restart treatment (rechallenge) until neutrophils return to a value of at least 1,000 per mm3 and consult with a hematologist. For detailed summary, see table 2. If the neutrophils fall below 1,500 per mm3, or below 1,000 in case of a BEN diagnosis, strict monitoring must be performed as described below: 1. A prescription must not be issued to a patient until after the treating physician has verified that the results of blood count result are normal. Subsequent blood count data, including the dates of the tests, must be centralized in a monitoring table in the patient’s file. The prescription for the medicine shall record a quantity according to the dosage and the date of the check. 2. In any instance of any febrile illness (such as a throat inflammation, tonsil inflammation, systemic inflammation or the appearance of fever for any reason), a CBC must be performed immediately (explain this to patients before starting the treatment). 3. If thrombocytes fall below 50,000 per mm3, discontinue the medicine and consult with a hematologist about the possibility of trying another therapeutic attempt. 4. If the number of neutrophils falls below the previous value by more than 50%, repeat the test within 4 days (see table 2 below). 5. Keep in mind that Benign Ethnic Neutropenia (BEN) exists among particular ethnic populations (such as among people of Yemenite or Ethiopian origin). In such instance, the baseline neutrophil count is low (typically lower than the norm by 500 – i.e., between 1,500 and 3,000). If BEN is suspected, consult with a hematologist and add the diagnosis to the patient’s list of diagnoses. BEN is not a contraindication to treatment with clozapine. 6. If the number of leukocytes falls below the previous value by 50% (even if they don’t reach a pathological level), consult with a hematologist. Keep in mind that a drop in the number of neutrophils is of the highest importance. When neutrophils drop below 1,500 /mm³, follow-up according to table 2. Table 2: Neutrophil monitoring scale: Neutropenia With BEN Level of Monitoring instructions actions severity diagnosis neutrophils no no BEN Higher than Once a week for 18 Neutropenia 1500 mm³ weeks. Subsequently, once a month BEN Higher than 1000³ mild Neutropenia no BEN Between Monitoring 3 times a After the value rises back 1000 and week until value rises above 1,500 per mm3, 1499 per back above 1,500 per resume normal monitoring mm³ mm3 frequency BEN Normal level, no special monitoring is necessary Moderate no BEN Between 500 Daily monitoring until Discontinue treatment with Neutropenia and 999 per value rises back clozapine. mm³ above 1,000 per mm3 Once neutrophils rise back above 1,000 per mm3, treatment with clozapine may be resumed, with monitoring 3 times a week until the level reaches 1,500 per mm3. Subsequently, monitoring according to the duration of the treatment. BEN Monitoring 3 times a Continue treatment with week until value rises clozapine. back above 1000 per After neutrophils rise back mm3 above 1,000 per mm3, resume normal monitoring frequency Acute no BEN below 500 Daily monitoring until Immediately discontinue Neutropenia per mm³ value rises back clozapine. above 1,000 per mm3 In any case, do not restart treatment (rechallenge) until neutrophils return to a value of at least 1,500 per mm3 and consult with a hematologist BEN Daily monitoring until Immediately discontinue value rises back clozapine. above 500 per mm3 In any case, do not restart treatment (rechallenge) until neutrophils return to a value of at least 1000 per mm3 and consult with a hematologist The incidence of agranulocytosis and the fatality rate in those developing agranulocytosis have decreased markedly since the institution of white blood cell (WBC) and absolute neutrophil count (ANC) monitoring. The precautionary measures stated below are therefore mandatory. Leponex must therefore only be used in schizophrenic patients in whom there is a demonstrated lack of response or inadequate response to other antipsychotic agents or who experience severe extrapyramidal side effects (in particular tardive dyskinesia) with other antipsychotic agents. Leponex may also be used in schizophrenic and schizoaffective patients who are at long- term risk of recurrent suicidal behaviour, based on their clinical history or current clinical picture. Patients with a history of drug-induced blood dyscrasia should on no account be treated with Leponex (see “Contraindications”). Prescribing physicians must comply fully with the required safety measures. At each consultation, a patient receiving Leponex should be reminded to contact the treating physician immediately if any kind of infection begins to develop. Particular attention should be paid to flu-like complaints or other symptoms such as fever or sore throat that indicate a possible infection. In such cases, a blood cell count must be performed immediately. Special precautions Haematology In view of the risk of agranulocytosis, the following precautionary measures are mandatory: Drugs known to have a substantial potential to suppress bone marrow function must not be used concomitantly with Leponex. Concomitant use of Leponex with depot antipsychotics must also be avoided because these potentially myelotoxic agents are only slowly eliminated from the body in emergency situations, e.g. in the event of granulocytopenia. Patients with a history of primary bone marrow disorders should only be given Leponex if the benefit outweighs the risk. They should be examined by a haematologist prior to therapy. The agreement of a haematologist must be obtained before giving Leponex to patients with a low white blood cell (WBC) count caused by benign ethnic neutropenia. Other situations required Immediate discontinuation of Leponex treatment are: Severe / life-threatening side effects and Patient who does not perform the routine blood tests. If possible, the patient should be admitted to a specialist haematology unit, where protective isolation and administration of GM-CSF (granulocyte/macrophage colony-stimulating factor) or G-CSF (granulocyte colony-stimulating factor) may be indicated. It is recommended that treatment with colony-stimulating factor be stopped once the ANC has again risen above 1.0 × 109/litre (1,000/mm3). In the event of infection, antibiotic therapy must be initiated immediately due to the risk of septic shock. In patients in whom Leponex has been discontinued due to white blood cell deficiencies, Leponex treatment may be restarted (rechallenged) only as described in table 2 above, including consulting a haematologist where stated. It is recommended that the results of blood counts be confirmed by performing counts on two consecutive days. However, Leponex should be discontinued after the first blood count. Leponex prescriptions must be marked “CBC” (= complete blood count) by the prescribing physician. In the event of thrombocytopenia (see “Adverse effects”), Leponex should be discontinued if the platelet count falls below 50 × 109/litre (50,000/mm3). Other precautions Cardiotoxicity Before starting treatment with clozapine, run an ECG and verify that there are no conduction abnormalities. Perform an ECG once every two months during the first four months of treatment; subsequently, once a year according to table 1. The length of the QTc interval must be documented in the patient’s file. The maximum QTc interval is 500 ms. In the event of prolongation, reduce the clozapine dosage and consult with a cardiologist. In the event of a gradual prolongation of QTc, it is recommended to perform ECG monitoring at a frequency of 3 times. Patients with heart disease should be started on a low dose (1 x 12.5 mg on the first day). The dose increase should only be increased slowly and in small increments (see “Dosage/Administration”). Use in patients with severe cardiovascular disorders is contraindicated (see “Contraindications”). Patients with a history of heart disease or abnormal cardiac findings on physical examination should be referred to a specialist for further investigation, which should include an ECG Such patients should only receive Leponex if the expected benefits clearly outweigh the risks. Orthostatic hypotension, with or without syncope, may occur during Leponex therapy. In rare cases (approx. one in 3,000 patients), collapse may be profound and may be accompanied by cardiac and/or respiratory arrest and possible fatal outcome. Such events are most likely during the initial titration phase in association with rapid dose escalation. In isolated cases, they have even occurred after the first dose. Such complications seem to occur more frequently with concomitant use of benzodiazepines or other psychotropic agents (see “Interactions”). Close medical supervision is therefore necessary at the start of Leponex therapy. In patients diagnosed with cardiomyopathy while on Leponex treatment, there is the risk of developing mitral valve incompetence. Mitral valve incompetence has been reported in cases of cardiomyopathy related to Leponex treatment. These cases of mitral valve incompetence were mild or moderate in severity, detected on two-dimensional echocardiography (2D-Echo). Monitoring of standing and supine blood pressure is necessary during the first weeks of treatment in patients with Parkinson’s disease. Myocarditis and cardiomyopathy In instances of a clinical suspicion of myocarditis (symptoms similar to flu, a drop in blood pressure, tachycardia, dyspnea, chest pain, and arrhythmias or symptoms of heart failure), perform an ECG and check the level of troponin, CRP, CBC and CK (creatine kinase). If myocarditis is suspected, immediately refer to an emergency room. The symptoms may occur in rare cases during the first two months of treatment and very rarely thereafter (see “Adverse effects”). If these symptoms occur, particularly during the titration period, diagnostic measures should be initiated as quickly as possible to rule out myocarditis. The symptoms of clozapine-induced myocarditis may also resemble those of myocardial infarction or influenza. There have been reports of myocarditis in the post- marketing period, including cases with a fatal outcome. The incidence of myocarditis as a result of clozapine is wide-ranging and ranges between 0.015-8.5%. There have also been reports of fatal cases of myocardial infarction. The assessment of causality was very difficult due to severe pre-existing cardiac disorders. If myocarditis or cardiomyopathy is suspected, Leponex must be discontinued immediately and the patient referred to a cardiologist without delay. The same signs and symptoms may also occur in the later stages of therapy and may then be associated with cardiomyopathy. In such cases, further investigation is indicated. If the diagnosis of cardiomyopathy is confirmed, Leponex must be discontinued. Patients who have had clozapine-induced myocarditis or cardiomyopathy should not be re-exposed to clozapine. Eosinophilia Cases of eosinophilia (higher than 700 per mm³) during treatment with clozapine (usually during the first month of treatment) have been associated with myocarditis (approximately 14%), pancreatitis, hepatitis, colitis, pericarditis/pericardial effusion or nephritis. This phenomenon can be part of a drug hypersensitivity syndrome (DRESS – Drug Reaction with Eosinophilia and Systemic Symptoms). Therefore, if eosinophilia appears, assess the systemic sensitivity symptoms (the appearance of a rash, allergic reactions, myocarditis or acute inflammatory reaction in any other organ) and, if there are, discontinue treatment with clozapine. Eosinophilia associated with clozapine, without inflammatory systemic effects, usually subside spontaneously, and therefore, the treatment may be continued while monitoring the ECG and performing weekly CBCs until the eosinophil count returns to normal. If the eosinophil count remains high for a number of weeks, even without systemic involvement, consult with a hematologist about further treatment or resume treatment with clozapine. QT prolongation As with other antipsychotic agents, caution is advised in patients with known cardiovascular disease or a family history of QT prolongation. As with other antipsychotic agents, caution is advised when prescribing Leponex in conjunction with drugs known to increase the QTc interval. Cerebrovascular events An approximately 3-fold increase in the risk of cerebrovascular events has been seen in the dementia population with some atypical antipsychotic agents. The reason for this increased risk is not known. An increased risk cannot be ruled out for other antipsychotic agents or for other patient populations. Leponex should therefore be used with particular caution in patients with risk factors for stroke. Seizures Leponex may lower the seizure threshold. The seizure ratio associated with clozapine is about 1% at a dosage of 150-300 mg per day and exceeds 3% at a dosage higher than 450 mg per day. At a dosage of higher than 600 mg per day (and when the level in the blood exceeds 600 ng/ml), the seizure ratio is higher. A correlation exists between the level of the medicine in the blood and the risk of seizures. A seizure episode is not an indication that clozapine should be discontinued. Consider adding an anticonvulsant medication. Alternatively, the clozapine dosage may be reduced. In any case, avoid administering carbamazepine. For patients with a history of seizures, consider administering preventive anticonvulsant treatment before starting treatment with clozapine. Patients with a history of epilepsy must be closely monitored during Leponex therapy since dose-related seizures have been reported (see “Interactions”). In such cases, the dose should be reduced. and If a patient has epilepsy, make sure that an anticonvulsant is used at a therapeutic level and consult with a neurologist if needed. In the event of a clozapine-induced seizure, it is recommended to determine the clozapine level in the blood 12 hours after the latest dose, to suspend continuing the medicine by 24 hours and, if there are no further muscular contractions, reduce the next dose to half a dose. If there are any doubts about continuation of the treatment or if there is a possibility that the seizures are not associated with clozapine, it is recommended to consult with a neurologist. In patients with a history of seizures, treatment should be started with a single dose of 12.5 mg on the first day and the dose increase should be slow and in small increments (see “Dosage/Administration”). Fever During Leponex therapy, patients may experience transient temperature elevations above 38°C, with the peak incidence in the first three weeks of treatment. This fever is generally benign. Occasionally, it may be associated with an increase or decrease in the white blood cell (WBC) count. Patients with fever should be carefully evaluated to rule out the possibility of an underlying infection or the development of agranulocytosis. Neuroleptic malignant syndrome (NMS) must be considered as a possible cause in patients presenting with high fever. If NMS is diagnosed, Leponex treatment should be immediately stopped and the necessary therapeutic measures initiated. At each consultation with the physician, the patient must be reminded of the importance of contacting the treating physician immediately at the first sign of fever, sore throat or other flu- like symptoms and especially of an infection which may be indicative of neutropenia. In such cases, a differential blood count must be performed immediately. Risk of thromboembolism Immobilisation must be avoided since Leponex may cause sedation and weight gain, thus increasing the risk of thromboembolism. Falls Leponex may cause seizures, somnolence, postural hypotension and motor and sensory instability that may lead to falls and resulting bone fractures or other injuries. An overall assessment of fall risk must be performed when initiating antipsychotic therapy in patients with illnesses, conditions or medications that may exacerbate these effects. This assessment should be repeated regularly in patients receiving long-term antipsychotic therapy. Anticholinergic effects Leponex possesses anticholinergic properties, which may lead to adverse effects throughout the body. Close monitoring is therefore required in the presence of prostatic enlargement and narrow-angle glaucoma. On account of its anticholinergic properties, Leponex may cause varying degrees of impairment to intestinal peristalsis, ranging from constipation to faecal impaction, intestinal obstruction, paralytic ileus, megacolon, bowel perforation and intestinal infarction/ischaemia. On rare occasions, these cases have been fatal (see “Adverse effects”). The reported incidence of constipation among clozapine patients is about 31% and of the development of ileus is 4%-8%. The mortality rate among patients who develop paralytic ileus is 20%-25%. Therefore, ask the patient every week during the first 18 weeks and subsequently, every month, about constipation or a decrease in the frequency of bowel movements (and document responses in the patient’s medical file). When necessary, an oral or osmotic laxative may be added or an enema may be used sporadically. Particular caution is necessary in patients with a history of colonic disease or a history of lower abdominal surgery, receiving concomitant medications known to cause constipation (especially those with anticholinergic properties, e.g. various antipsychotic agents, antidepressants and antiparkinsonian agents), as these may exacerbate the situation. It is vital that constipation be recognised and actively treated. Special precautions should be observed when considering co-administration with benzodiazepines (or other centrally-acting drugs; see “Interactions”). Metabolic changes Atypical antipsychotic drugs, including Leponex, were associated with metabolic changes, which raise the cardiovascular/cerebrovascular risk. These metabolic changes may include hyperglycaemia, dyslipidaemia and weight gain. While atypical antipsychotic drugs may cause some metabolic changes, each drug has its own specific risk profile within its drug class. Treatment with clozapine leads to weight gain at a higher ratio than with all other antipsychotics and to a higher incidence of metabolic symptoms. Hyperglycaemia. Cases of diabetes mellitus, severe hyperglycaemia and even ketoacidosis or hyperosmolar coma have been reported, even in patients with no prior history of hyperglycaemia or diabetes mellitus. No causal relationship to Leponex has been established, although blood glucose levels returned to normal in most patients following discontinuation of Leponex. Re-exposure was positive in a small number of cases. The effect of Leponex on glucose metabolism in patients with pre-existing diabetes mellitus has not been studied. Patients with diabetes mellitus starting on antipsychotic drugs should have their blood sugar levels regularly monitored. Patients with risk factors of diabetes mellitus (e.g. excess weight, a family history of diabetes) starting on atypical antipsychotic drugs should have their fasting blood sugar levels tested prior to and regularly during treatment. The possibility of impaired glucose tolerance should be considered in patients treated with Leponex who develop hyperglycaemia with symptoms such as polydipsia, polyuria, polyphagia or weakness. Patients, who develop symptoms of hyperglycaemia during treatment with atypical antipsychotic drugs, should have their fasting blood sugar levels tested. In some cases, hyperglycaemia may return to normal after stopping treatment with atypical antipsychotic drugs. In other cases, hyperglycaemia may require further treatment despite stopping using atypical antipsychotic drugs. Discontinuation of Leponex should be considered in patients with significant treatment-related hyperglycaemia. Diabetes Diabetes may develop among clozapine patients at a higher incidence than among the general population. Consequently, monitor the BMI, monitor metabolic indicators and monitor the fasting glucose levels and HbA1C (at a community mental health center or in documented coordination with the family physician) as specified in table 1. In the event of significant changes in metabolic indicators, it is recommended to consider adding treatment for the metabolic side effect and, in extreme cases, to consider whether treatment with clozapine should continue, after consultation between the treating psychiatrist and the family physician, and while weighing benefit against risk. Dyslipidaemia Patients treated with atypical antipsychotic drugs, including Leponex, experienced undesired weight changes. Clinical monitoring, including baseline and regular follow-ups, is recommended. Weight gain Patients treated with atypical antipsychotic drugs, including Leponex, experienced weight gain. Clinical monitoring of weight is recommended. Depression If a patient develops major depression during treatment with clozapine, antidepressants having no interactions with other medicinal products may be used while taking clozapine (such as sertraline, citalopram, escitalopram or venlafaxine). Special patient groups Hepatic disorders Patients with stable pre-existing liver disease may receive Leponex, but hepatic function must be regularly monitored. Liver function tests must be performed immediately in any patient developing symptoms of possible hepatic dysfunction (e.g. nausea, vomiting, loss of appetite) during Leponex treatment. If the elevation of the values is clinically relevant or if symptoms of jaundice occur, treatment with Leponex must be discontinued. It may only be resumed when the results of liver function tests return to normal. Close monitoring is necessary in such cases. Renal disorders Patients with mild to moderate renal impairment should be started on a low dose (1 x 12.5 mg on the first day) (see “Dosage/Administration”). Elderly patients (≥60 years) It is recommended that treatment be initiated at a lower dose in elderly patients (see “Dosage/Administration”). Orthostatic hypotension may occur in patients treated with Leponex. There have been rare reports of tachycardia, which may be sustained. Elderly patients (≥60 years), particularly those with impaired cardiovascular function, may be more susceptible than others to these effects. Some elderly patients may also be particularly susceptible to the anticholinergic effects of Leponex (e.g. urinary retention and constipation). Psychosis/behavioural disorders in elderly patients with dementia The risk of mortality was higher with atypical antipsychotic agents than with placebo in elderly patients (≥60 years) with dementia-related psychosis/behavioural disorders. Analysis of 17 placebo-controlled studies showed a mortality risk in this patient population that was 1.6 to 1.7 times higher than with placebo. Risk factors for higher mortality with antipsychotic agents are: sedation, cardiovascular disease (e.g. arrhythmias, sudden cardiac death) or pulmonary disease (e.g. pneumonia, with or without aspiration). Leponex is not approved for the treatment of psychosis/behavioural disorders in elderly patients (≥60 years) with dementia. Rebound / withdrawal symptoms If abrupt discontinuation of Leponex treatment is required (e.g. leukopenia), patients should be carefully monitored for recurrence of psychotic symptoms and symptoms associated with cholinergic rebound such as sweating, headache, nausea, vomiting and diarrhoea. Lactose Patients with rare hereditary problems of galactose intolerance, total lactose deficiency or glucose-galactose malabsorption should not take this medicine.
Effects on Driving
4.7 Effects on ability to drive and use machines Leponex impairs the patient’s reactions and the ability to drive and to use tools or machines. Leponex has a sedative effect and may reduce the seizure threshold. Patients should therefore refrain from activities such as driving or using machinery, particularly during the first weeks of treatment.

שימוש לפי פנקס קופ''ח כללית 1994
Schizophrenia in patients unresponsive to or intolerant of conventional antipsychotic drugs. התרופה תימצא רק בבתי חולים ותנופק לחולים אמבולטורים רק באמצעותם
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה אשפוזית לפי החלטת משרד הבריאות
מידע נוסף
