Quest for the right Drug
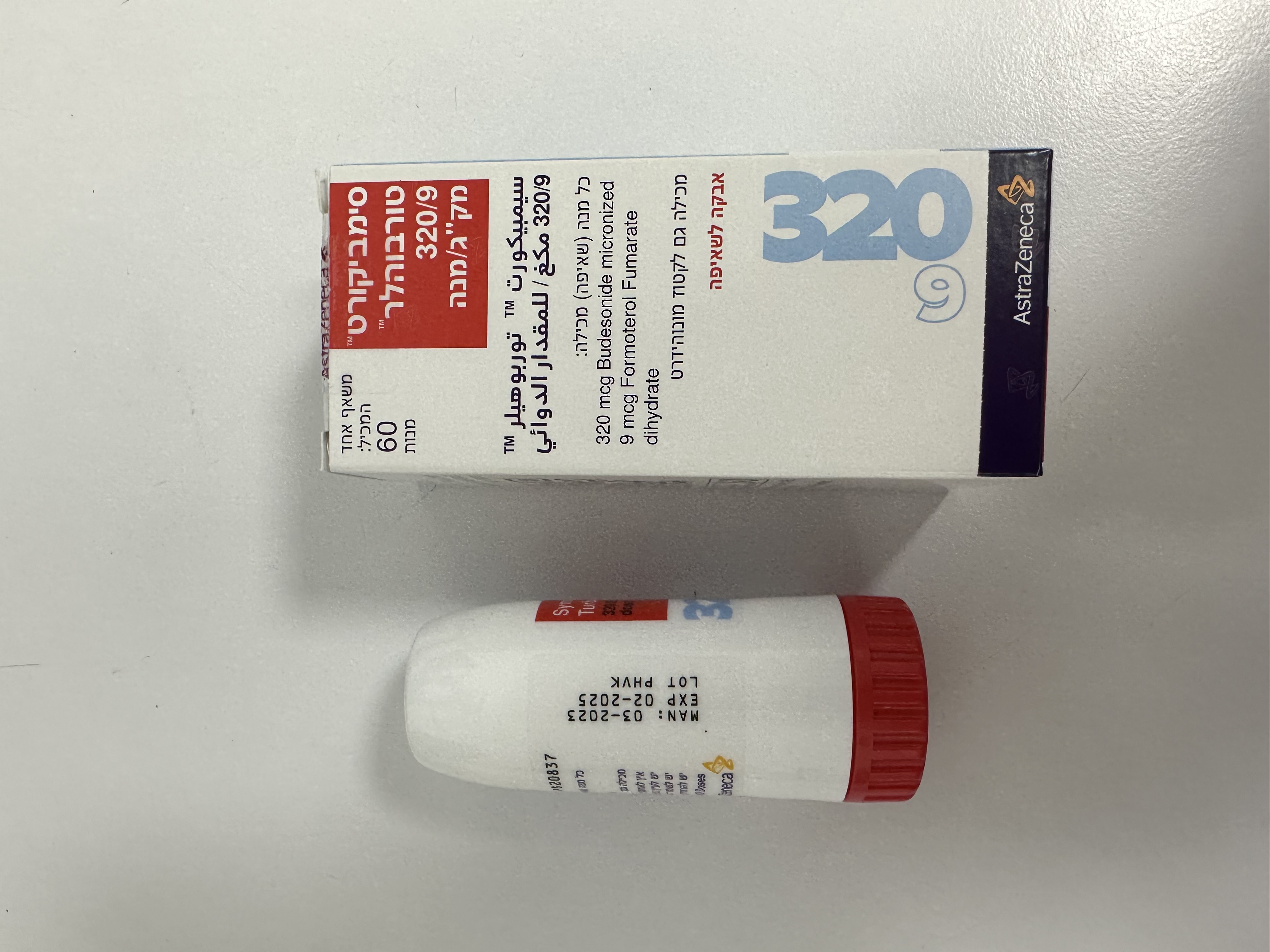
סימביקורט טורבוהלר 320/9 מק"ג/מנה SYMBICORT TURBUHALER 320/9 MCG/DOSE (BUDESONIDE MICRONIZED, FORMOTEROL FUMARATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
שאיפה : INHALATION
צורת מינון:
אבקה לשאיפה : POWDER FOR INHALATION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Drugs for obstructive airway diseases: Adrenergics, Inhalants. ATC-code: R03AK07. Mechanisms of action and Pharmacodynamic effects Symbicort Turbuhaler 320/9 mcg/dose contains formoterol and budesonide, which have different modes of action and show additive effects in terms of reduction of asthma exacerbations. The mechanisms of action of the two substances, respectively are discussed below. Budesonide Budesonide is a glucocorticosteroid which when inhaled has a dose-dependent anti- inflammatory action in the airways, resulting in reduced symptoms and fewer asthma exacerbations. Inhaled budesonide has less severe adverse effects than systemic corticosteroids. The exact mechanism responsible for the anti-inflammatory effect of glucocorticosteroids is unknown. Formoterol Formoterol is a selective β2 adrenoceptor-agonist that when inhaled results in rapid and long-acting relaxation of bronchial smooth muscle in patients with reversible airways obstruction. The bronchodilating effect is dose-dependent, with an onset of effect within 1-3 minutes. The duration of effect is at least 12 hours after a single dose. Clinical efficacy and safety Asthma Clinical studies in adults have shown that the addition of formoterol to budesonide improved asthma symptoms and lung function, and reduced exacerbations. In two 12-week studies the effect on lung function of budesonide/formoterol was equal to that of the free combination of budesonide and formoterol, and exceeded that of budesonide alone. All treatment arms used a short-acting beta2-agonist as needed. There was no sign of attenuation of the anti-asthmatic effect over time. Two 12-week paediatric studies have been performed in which 265 children aged 6-11 years were treated with a maintenance dose of budesonide/formoterol (2 inhalations of 80 micrograms /4.5 micrograms/inhalation twice daily), and a short-acting β2 adrenoceptor-agonist as needed. In both studies, Lung function was improved and the treatment was well tolerated compared to the corresponding dose of budesonide alone. COPD In two 12-month studies, the effect on lung function and the rate of exacerbation (defined as courses of oral steroids and/or course of antibiotics and/or hospitalisations) in patients with moderate to severe COPD was evaluated. The inclusion criteria for both studies was pre-bronchodilator FEVI <50% predicted normal. Median post- bronchodilator FEVI at inclusion in the trials was 42% predicted normal. The mean number of exacerbations per year (as defined above) was significantly reduced with budesonide/formoterol as compared with treatment with formoterol alone or placebo (mean rate 1.4 compared with 1.8-1.9 in the placebo/formoterol group). The mean number of days on oral corticosteroids/patient during the 12 months was slightly reduced in the budesonide/formoterol group (7-8 days/patient/year compared with 11- 12 and 9-12 days in the placebo and formoterol groups, respectively). For changes in lung-function parameters, such as FEV1, budesonide/formoterol was not superior to treatment with formoterol alone.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption The fixed-dose combination of budesonide and formoterol, and the corresponding monoproducts have been shown to be bioequivalent with regard to systemic exposure of budesonide and formoterol, respectively. In spite of this, a small increase in cortisol suppression was seen after administration of the fixed-dose combination compared to the monoproducts. The difference is considered not to have an impact on clinical safety. There was no evidence of pharmacokinetic interactions between budesonide and formoterol. Pharmacokinetic parameters for the respective substances were comparable after the administration of budesonide and formoterol as monoproducts or as the fixed-dose combination. For budesonide, AUC was slightly higher, rate of absorption more rapid and maximal plasma concentration higher after administration of the fixed combination. For formoterol, maximal plasma concentration was similar after administration of the fixed combination. Inhaled budesonide is rapidly absorbed and the maximum plasma concentration is reached within 30 minutes after inhalation. In studies, mean lung deposition of budesonide after inhalation via the powder inhaler ranged from 32% to 44% of the delivered dose. The systemic bioavailability is approximately 49% of the delivered dose. In children 6-16 years of age the lung deposition falls in the same range as in adults for the same given dose. The resulting plasma concentrations were not determined. Inhaled formoterol is rapidly absorbed and the maximum plasma concentration is reached within 10 minutes after inhalation. In studies the mean lung deposition of formoterol after inhalation via the powder inhaler ranged from 28%-49% of the delivered dose. The systemic bioavailability is about 61% of the delivered dose. Distribution and biotransformation Plasma protein binding is approximately 50% for formoterol and 90% for budesonide. Volume of distribution is about 4 L/kg for formoterol and 3 L/kg for budesonide. Formoterol is inactivated via conjugation reactions (active O-demethylated and deformylated metabolites are formed, but they are seen mainly as inactivated conjugates). Budesonide undergoes an extensive degree (approximately. 90%) of biotransformation on first passage through the liver to metabolites of low glucocorticosteroid activity. The glucocorticosteroid activity of the major metabolites, 6-beta-hydroxy-budesonide and 16-alfa-hydroxy-prednisolone, is less than 1% of that of budesonide. There are no indications of any metabolic interactions or any displacement reactions between formoterol and budesonide. Elimination The major part of a dose of formoterol is transformed by liver metabolism followed by renal elimination. After inhalation, 8-13% of the delivered dose of formoterol is excreted unmetabolised in the urine. Formoterol has a high systemic clearance (approximately 1.4 L/min) and the terminal elimination half-life averages 17 hours. Budesonide is eliminated via metabolism mainly catalysed by the enzyme CYP3A4. The metabolites of budesonide are eliminated in urine as such or in conjugated form. Only negligible amounts of unchanged budesonide have been detected in the urine. Budesonide has a high systemic clearance (approximately 1.2 L/min) and the plasma elimination half-life after i.v. dosing averages 4 hours. The pharmacokinetics of budesonide or formoterol in children and patients with renal failure is unknown. The exposure of budesonide and formoterol may be increased in patients with liver disease. Linearity/Non-linearity Systemic exposure for both budesonide and formoterol correlates in a linear fashion to administered dose.

מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| COPD | ||||
| אסטמה |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/2009
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
