Quest for the right Drug
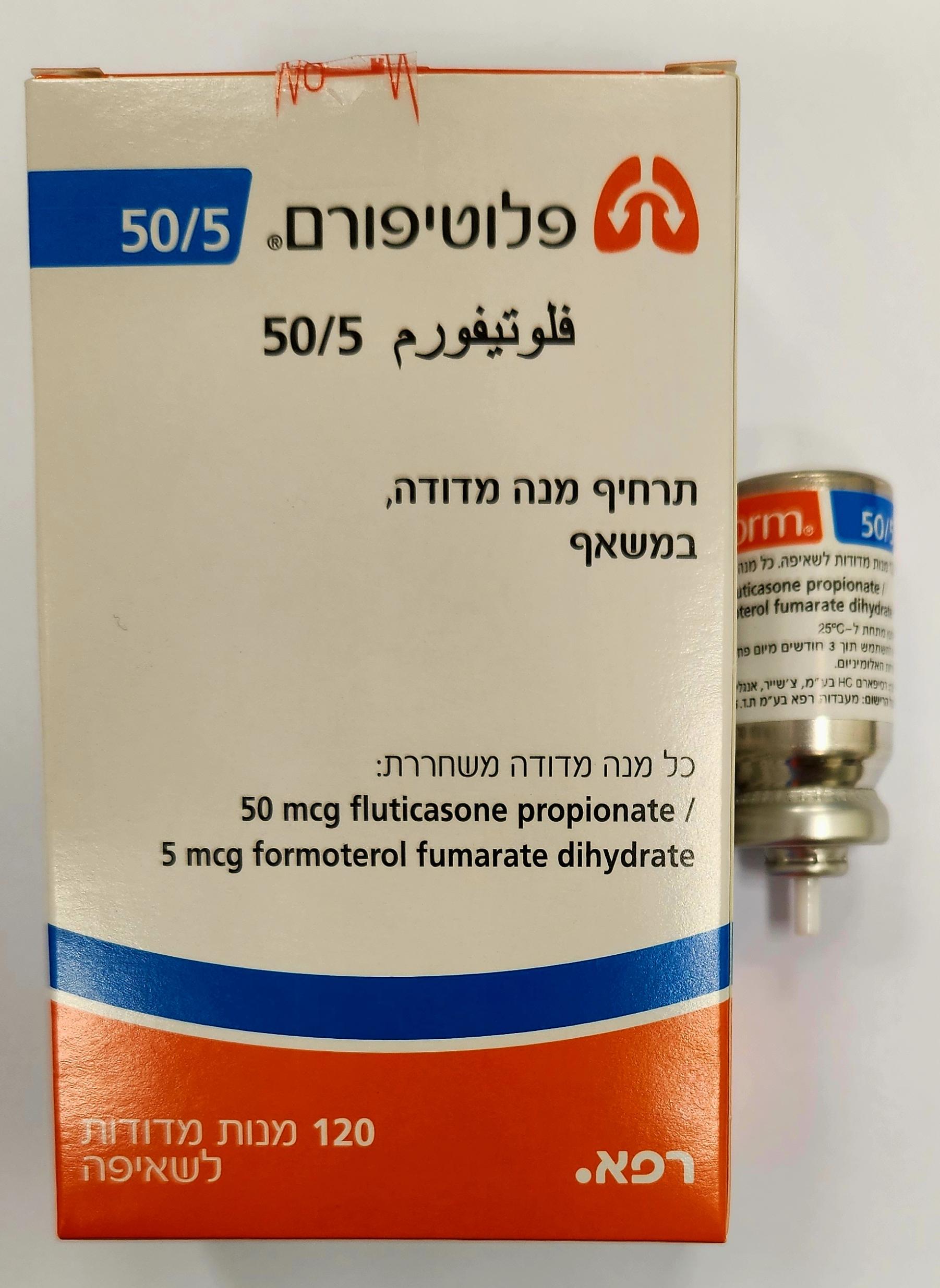
פלוטיפורם 50/5 FLUTIFORM 50/5 (FLUTICASONE PROPIONATE, FORMOTEROL FUMARATE DIHYDRATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
שאיפה : INHALATION
צורת מינון:
תרחיף בלחץ לשאיפה : PRESSURISED SUSPENTION FOR INHALATION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Flutiform 50/5 inhaler is indicated in adults, adolescents and children 5 years and above. Flutiform 125 /5 inhaler is indicated in adults and adolescents aged 12 years and above. Flutiform 250 /10 inhaler is indicated in adults aged 18 years and above only. The management of asthma should normally follow a stepwise programme and patients’ responses should be monitored clinically and by lung function tests. Flutiform inhaler should not be used to treat acute asthma symptoms for which a fast and short- acting bronchodilator is required. Patients should be advised to have their medicine to be used for relief in an acute asthma attack available at all times. The prophylactic use of Flutiform inhaler in exercise-induced asthma has not been studied. For such use, a separate rapid-acting bronchodilator should be considered. Patients should be reminded to take their Flutiform inhaler maintenance dose as prescribed, even when asymptomatic. Patients should not be initiated on Flutiform inhaler during an exacerbation, or if they have significantly worsening or acutely deteriorating asthma. Serious asthma-related adverse events and exacerbations may occur during treatment with Flutiform inhaler. Patients should be asked to continue treatment but to seek medical advice if asthma symptoms remain uncontrolled or worsen after initiation on Flutiform inhaler. Flutiform inhaler should not be used as the first treatment for asthma. If increasing use of short-acting bronchodilators to relieve asthma is required, if short-acting bronchodilators become less effective, or ineffective or if asthma symptoms persist, the patient should be reviewed by their doctor as soon as possible as any of these may indicate a deterioration in asthma control and their treatment may need to be changed. Sudden and progressive deterioration in control of asthma is potentially life-threatening and the patient should undergo urgent medical assessment. Consideration should be given to increasing corticosteroid therapy. The patient should also be medically reviewed when the current dosage of Flutiform inhaler has failed to give adequate control of asthma. Consideration should be given to additional corticosteroid therapies. Once asthma symptoms are controlled, consideration may be given to gradually reducing the dose of Flutiform inhaler. Regular review of patients as treatment is stepped down is important. The lowest effective dose of Flutiform inhaler should be used (see section 4.2). Treatment with Flutiform inhaler should not be stopped abruptly in patients with asthma due to risk of exacerbation. Therapy should be down-titrated under the supervision of a prescriber. An exacerbation of the clinical symptoms of asthma may be due to an acute respiratory tract bacterial infection and treatment may require appropriate antibiotics, increased inhaled corticosteroids and a short course of oral corticosteroids. A rapid-acting inhaled bronchodilator should be used as rescue medication. As with all inhaled medication containing corticosteroids, Flutiform inhaler should be administered with caution in patients with pulmonary tuberculosis, quiescent tuberculosis or patients with fungal, viral or other infections of the airway. Any such infections must always be adequately treated if Flutiform inhaler is being used. Flutiform inhaler should be used with caution in patients with thyrotoxicosis, phaeochromocytoma, diabetes mellitus, uncorrected hypokalaemia or patients predisposed to low levels of serum potassium, hypertrophic obstructive cardiomyopathy, idiopathic subvalvular aortic stenosis, severe hypertension, aneurysm or other severe cardiovascular disorders, such as ischaemic heart disease, cardiac arrhythmias or severe heart failure. Potentially serious hypokalaemia may result from high doses of β2 agonists. Concomitant treatment of β2 agonists with drugs which can induce hypokalaemia or potentiate a hypokalaemic effect, e.g. xanthine derivatives, steroids and diuretics, may add to a possible hypokalaemic effect of the β2 agonist. Particular caution is recommended in unstable asthma with variable use of rescue bronchodilators, in acute severe asthma as the associated risk may be augmented by hypoxia and in other conditions when the likelihood for hypokalaemia adverse effects is increased. It is recommended that serum potassium levels are monitored during these circumstances. Caution must be observed when treating patients with existing prolongation of the QTc interval. Formoterol itself may induce prolongation of the QTc interval. As for all β2 agonists, additional blood sugar controls should be considered in diabetic patients. Care should be taken when transferring patients to Flutiform inhaler therapy, particularly if there is any reason to suppose that adrenal function is impaired from previous systemic steroid therapy. As with other inhalation therapy paradoxical bronchospasm may occur with an immediate increase in wheezing and shortness of breath after dosing. Paradoxical bronchospasm responds to a rapid- acting inhaled bronchodilator and should be treated straight away. Flutiform inhaler should be discontinued immediately, the patient assessed and alternative therapy instituted if necessary. Visual disturbance may be reported with systemic and topical corticosteroid use. If a patient presents with symptoms such as blurred vision or other visual disturbances, the patient should be considered for referral to an ophthalmologist for evaluation of possible causes which may include cataract, glaucoma or rare diseases such as central serous chorioretinopathy (CSCR) which have been reported after use of systemic and topical corticosteroids. Systemic effects may occur with any inhaled corticosteroid, particularly at high doses prescribed for long periods. These effects are much less likely to occur than with oral corticosteroids. Possible systemic effects include Cushing's syndrome, Cushingoid features, adrenal suppression, growth retardation in children and adolescents, decrease in bone mineral density, cataract glaucoma and more rarely, a range of psychological or behavioural effects including psychomotor hyperactivity, sleep disorders, anxiety, depression or aggression (particularly in children). It is important, therefore, that the patient is reviewed regularly and the dose of inhaled corticosteroid is reduced to the lowest dose at which effective control of asthma is maintained. Prolonged treatment of patients with high doses of inhaled corticosteroids may result in adrenal suppression and acute adrenal crisis. Children and adolescents <16 years taking high doses of fluticasone propionate (typically ≥ 1000 micrograms/day) may be at particular risk. Very rare cases of adrenal suppression and acute adrenal crisis have also been described with doses of fluticasone propionate between 500 and less than 1000 micrograms. Situations, which could potentially trigger acute adrenal crisis include trauma, surgery, infection or any rapid reduction in dosage. Presenting symptoms are typically vague and may include anorexia, abdominal pain, weight loss, tiredness, headache, nausea, vomiting, hypotension, decreased level of consciousness, hypoglycaemia, and seizures. Additional systemic corticosteroid treatment should be considered during periods of stress or elective surgery. The benefits of inhaled fluticasone propionate therapy should minimise the need for oral steroids, but patients transferring from oral steroids may remain at risk of impaired adrenal reserve for a considerable time. Patients who have required high dose emergency corticosteroid therapy in the past may also be at risk. This possibility of residual impairment should always be borne in mind in emergency and elective situations likely to produce stress, and appropriate corticosteroid treatment must be considered. The extent of the adrenal impairment may require specialist advice before elective procedures. In situations of possible impaired adrenal function hypothalamic pituitary adrenocortical (HPA) axis function should be monitored regularly. There is an increased risk of systemic side effects when combining fluticasone propionate with potent CYP3A4 inhibitors (see section 4.5). The patient should be made aware that this fixed-dose combination inhaler is a prophylactic therapy and as such has to be used regularly even when asymptomatic for optimum benefit. Use of a spacer device may lead to a possible increase in pulmonary deposition and a potential increase in systemic absorption and systemic adverse events. As the fractions of fluticasone and formoterol which reach systemic circulation are primarily eliminated via hepatic metabolism, an increased exposure can be expected in patients with severe hepatic impairment. Patients should be advised that Flutiform inhaler contains 2 mg of alcohol (ethanol) in each dose (2 inhalations). The amount in each dose is equivalent to less than 1 ml of beer or 1 ml of wine. The small amount of alcohol in this medicinal product will not have any noticeable effects. Paediatric population It is recommended that the height of children receiving prolonged treatment with inhaled corticosteroids is regularly monitored. If growth is slowed, therapy should be reviewed with the aim of reducing the dose of inhaled corticosteroid, if possible, to the lowest dose at which effective control of asthma is maintained. In addition, consideration should be given to referring the patient to a paediatric respiratory specialist. Possible systemic effects as reported for the individual components of Flutiform inhaler include Cushing's syndrome, Cushingoid features, adrenal suppression and growth retardation in children and adolescents. Children may also experience anxiety, sleep disorders and behavioural changes, including hyperactivity and irritability (see section 4.8). Limited data are available in respect of the use of Flutiform inhaler in children under 5 years of age. Flutiform inhaler is NOT recommended for use in children under 5 years of age.
Effects on Driving
4.7 Effects on ability to drive and use machines Flutiform inhaler has no or negligible influence on the ability to drive and use machines.

מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| אסטמה | ||||
| אסטמה | ||||
| אסטמה | ||||
| אסטמה | ||||
| אסטמה | ||||
| אסטמה | ||||
| אסטמה | ||||
| אסטמה | ||||
| אסטמה | ||||
| אסטמה |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
12/01/2014
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
08.08.22 - עלון לצרכן אנגלית 08.08.22 - עלון לצרכן עברית 08.08.22 - עלון לצרכן ערבית 07.06.23 - עלון לצרכן עברית 12.02.24 - עלון לצרכן עברית 05.04.24 - עלון לצרכן אנגלית 05.04.24 - עלון לצרכן עברית 05.04.24 - עלון לצרכן ערבית 29.03.21 - החמרה לעלון 19.04.21 - החמרה לעלון 07.06.23 - החמרה לעלון 12.02.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
פלוטיפורם 50/5