Quest for the right Drug
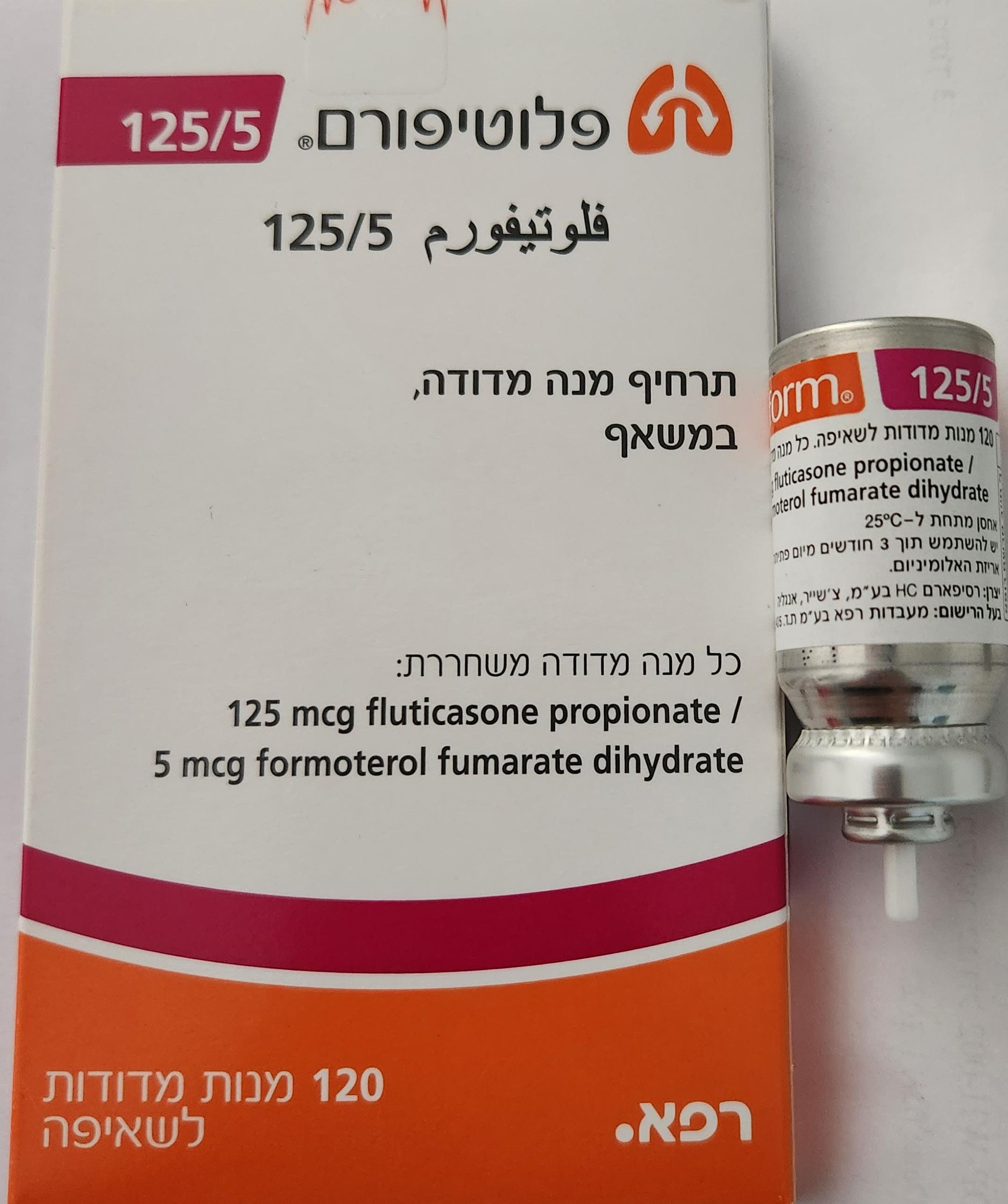
פלוטיפורם 125/5 FLUTIFORM 125/5 (FLUTICASONE PROPIONATE, FORMOTEROL FUMARATE DIHYDRATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
שאיפה : INHALATION
צורת מינון:
תרחיף בלחץ לשאיפה : PRESSURISED SUSPENTION FOR INHALATION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic Group: Drugs for obstructive airways adrenergics in combination with corticosteroids or other drugs excl. anticholinergics ATC code: R03AK11 Mechanism of Action and Pharmacodynamic Effects Flutiform inhaler contains both fluticasone propionate and formoterol fumarate. The mechanisms of action are described below for the individual components. These drugs represent two classes of medications (a synthetic corticosteroid and a selective, long-acting β2 adrenergic receptor agonist) and as with other inhaled corticosteroid and long-acting β2 adrenergic agonist combinations additive effects are seen in terms of a reduction in asthma exacerbations. Fluticasone propionate Fluticasone propionate is a synthetic, trifluorinated glucocorticoid with potent anti-inflammatory activity in the lungs when given by inhalation. Fluticasone propionate reduces symptoms and exacerbations of asthma with less adverse effects than when corticosteroids are administered systemically. Formoterol fumarate Formoterol fumarate is a long-acting selective β2 adrenergic receptor agonist. Inhaled formoterol fumarate acts locally in the lung as a bronchodilator. The onset of bronchodilating effect is rapid, within 1 - 3 minutes, and the duration of effect is at least 12 hours after a single dose. Flutiform inhaler In 12-week clinical trials in adults and adolescents, the addition of formoterol to fluticasone propionate improved asthma symptoms and lung function and reduced exacerbations. Therapeutic effect of Flutiform inhaler exceeded that of fluticasone propionate alone. There are no long-term data comparing Flutiform inhaler with fluticasone propionate. In an 8-week clinical trial the effect on lung function with Flutiform inhaler was at least equal to that of the combination of fluticasone propionate and formoterol fumarate when administered as separate inhalers. Long-term comparative data of Flutiform inhaler versus fluticasone propionate and formoterol fumarate are not available. There were no signs of attenuation of therapeutic effects of Flutiform inhaler in trials lasting up to 12 months including adult and adolescent patients. Dose-response trends for Flutiform inhaler were evident for symptom-based endpoints, with incremental benefits from high versus low dose Flutiform inhaler being most likely in patients with more severe asthma. Paediatric population In a 12-week double-blind study 512 children aged 5 – 11 years were randomised to Flutiform inhaler (2 inhalations of 50/5 micrograms twice daily), fluticasone/salmeterol or fluticasone monotherapy. Flutiform inhaler (2 inhalations of 50/5 micrograms twice daily) was superior to fluticasone monotherapy and non-inferior to fluticasone/salmeterol with regards to change from baseline in pre-dose FEV1 to post dose FEV1 over 12 weeks and 4-hour FEV1 AUC at Week 12. Flutiform inhaler (2 inhalations of 50/5 micrograms twice daily) was not superior to fluticasone monotherapy in change in pre-dose FEV1 over the 12-week treatment but was non-inferior to fluticasone/salmeterol on this endpoint. In a second 12-week paediatric study including a 6-month extension phase for long-term safety 210 children aged 4 - 12 years were treated with a maintenance dose of Flutiform inhaler (2 inhalations of 50/5 micrograms twice daily) or with fluticasone/salmeterol. Flutiform inhaler (2 inhalations of 50/5 micrograms twice daily) was non-inferior to fluticasone/salmeterol. Two hundred and five patients subsequently completed the 6-month extension phase during which they received Flutiform inhaler (2 inhalations of 50/5 micrograms twice daily). Flutiform inhaler was safe and well tolerated.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Fluticasone propionate: Absorption Following inhalation, systemic absorption of fluticasone propionate occurs mainly through the lungs and has been shown to be linearly related to dose over the dose range 500 to 2000 micrograms. Absorption is initially rapid then prolonged. Published studies using oral dosing of labelled and unlabelled drug have demonstrated that the absolute oral systemic bioavailability of fluticasone propionate is negligible (<1%) due to a combination of incomplete absorption from the GI tract and extensive first-pass metabolism. Distribution Following intravenous administration, fluticasone propionate is extensively distributed in the body. The initial disposition phase for fluticasone propionate is rapid and consistent with its high lipid solubility and tissue binding. The volume of distribution averages 4.2 L/kg. The percentage of fluticasone propionate bound to human plasma proteins averages 91%. Fluticasone propionate is weakly and reversibly bound to erythrocytes and is not significantly bound to human transcortin. Biotransformation The total clearance of fluticasone propionate is high (average, 1,093 mL/min), with renal clearance accounting for less than 0.02% of the total. The very high clearance rate indicates extensive hepatic clearance. The only circulating metabolite detected in man is the 17β-carboxylic acid derivative of fluticasone propionate, which is formed through the cytochrome P450 3A4 isoform subfamily (CYP 3A4) pathway. This metabolite has less affinity (approximately 1/2000) than the parent drug for the glucocorticoid receptor of human lung cytosol in vitro. Other metabolites detected in vitro using cultured human hepatoma cells have not been detected in man. Elimination 87 - 100% of an oral dose is excreted in the faeces, up to 75% as parent compound. There is also a non-active major metabolite. Following intravenous dosing, fluticasone propionate shows polyexponential kinetics and has a terminal elimination half-life of approximately 7.8 hours. Less than 5% of a radiolabelled dose is excreted in the urine as metabolites, and the remainder is excreted in the faeces as parent drug and metabolites. Formoterol fumarate: Data on the plasma pharmacokinetics of formoterol were collected in healthy volunteers after inhalation of doses higher than the recommended range and in COPD patients after inhalation of therapeutic doses. Absorption Following inhalation of a single 120 microgram dose of formoterol fumarate by healthy volunteers, formoterol was rapidly absorbed into plasma, reaching a maximum concentration of 91.6 pg/ml within 5 minutes of inhalation. In COPD patients treated for 12 weeks with formoterol fumarate 12 or 24 micrograms b.i.d. the plasma concentrations of formoterol ranged between 4.0 and 8.9 pg/ml and 8.0 and 17.3 pg/ml respectively at 10 minutes, 2 hours and 6 hours post inhalation. Studies investigating the cumulative urinary excretion of formoterol and/or its (RR) and (SS)-enantiomers, after inhalation of dry powder (12 - 96 micrograms) or aerosol formulations (12-96 micrograms), showed that absorption increased linearly with the dose. After 12 weeks administration of 12 micrograms or 24 micrograms formoterol powder b.i.d., the urinary excretion of unchanged formoterol increased by 63 - 73% in adult patients with asthma, by 19 - 38% in adult patients with COPD and by 18 - 84% in children, suggesting a modest and self- limiting accumulation of formoterol in plasma after repeated dosing. Distribution The plasma protein binding of formoterol is 61 - 64% (34% primarily to albumin). There is no saturation of binding sites in the concentration range reached with therapeutic doses. The concentrations of formoterol used to assess the plasma protein binding were higher than those achieved in plasma following inhalation of a single 120 microgram dose. Biotransformation Formoterol is eliminated primarily by metabolism, direct glucuronidation being the major pathway of biotransformation, with O-demethylation followed by further glucuronidation being another pathway. Minor pathways involve sulphate conjugation of formoterol and deformylation followed by sulphate conjugation. Multiple isozymes catalyze the glucuronidation (UGT1A1, 1A3, 1A6, 1A7, 1A8, 1A9, 1A10, 2B7 and 2B15) and O-demethylation (CYP 2D6, 2C19, 2C9 and 2A6) of formoterol, and so consequently the potential for metabolic drug-drug interaction is low. Formoterol did not inhibit cytochrome P450 isozymes at therapeutically relevant concentrations. The kinetics of formoterol is similar after single and repeated administration, indicating no auto- induction or inhibition of metabolism. Elimination In asthmatic and COPD patients treated for 12 weeks with 12 or 24 micrograms formoterol fumarate b.i.d., approximately 10% and 7% of the dose, respectively, were recovered in the urine as unchanged formoterol. In asthmatic children, approximately 6% of the dose was recovered in the urine as unchanged formoterol after multiple dosing of 12 and 24 micrograms. The (R,R) and (S,S)- enantiomers accounted for 40% and 60% respectively of urinary recovery of unchanged formoterol, after single doses (12 to 120 micrograms) in healthy volunteers and after single and repeated doses in asthma patients. After a single oral dose of 3H-formoterol, 59 - 62% of the dose was recovered in the urine and 32 - 34% in the faeces. Renal clearance of formoterol is 150 ml/min. After inhalation, plasma formoterol kinetics and urinary excretion rate data in healthy volunteers indicate a biphasic elimination, with the terminal elimination half-lives of the (R, R) - and (S, S)- enantiomers being 13.9 and 12.3 hours, respectively. Peak excretion occurs rapidly, within 1.5 hours. Approximately 6.4 - 8% of the dose was recovered in the urine as unchanged formoterol, with the (R, R) - and (S, S)-enantiomers contributing 40% and 60%, respectively. Flutiform inhaler - (fluticasone propionate/formoterol fumarate combination): A number of studies have examined the pharmacokinetic characteristics of fluticasone propionate and formoterol fumarate from Flutiform inhaler compared with the individual components, given both together and separately. There is a high variability both within and between the pharmacokinetic studies however, in general there is a trend for the systemic exposure of fluticasone and formoterol to be less from this fixed combination of fluticasone propionate and formoterol fumarate than from the individual components given together. Pharmacokinetic equivalence between Flutiform inhaler and the constituent monoproducts has not been demonstrated. Long-term comparative data of Flutiform inhaler versus fluticasone propionate and formoterol fumarate are not available (see section 5.1) Absorption Flutiform inhaler – fluticasone propionate Following inhalation of a single 250 microgram dose of fluticasone propionate from 2 actuations of Flutiform 125 /5 inhaler by healthy volunteers, fluticasone propionate was rapidly absorbed into the plasma, reaching a mean maximum plasma fluticasone concentration of 32.8 pg/ml within 45 minutes of inhalation. In asthma patients who received single doses of fluticasone propionate from Flutiform inhaler, mean maximum plasma concentrations of 15.4 pg/ml and 27.4 pg/ml were achieved within 20 minutes and 30 minutes for 100 microgram/10 microgram (2 actuations of Flutiform 50 /5 inhaler) and 250 microgram/10 microgram (2 actuations of Flutiform 125 /5 inhaler) doses respectively. In multiple dose studies in healthy volunteers, Flutiform inhaler doses of 100 microgram/10 microgram, 250 microgram/10 microgram and 500 microgram/20 microgram resulted in mean maximum plasma fluticasone concentrations of 21.4, 25.9 to 34.2 and 178 pg/ml respectively. The data for the 100 microgram/10 microgram and 250 microgram/10 microgram doses were generated by use of a device without a spacer and the data for the 500 microgram/20 microgram dose were generated by use of a device with a spacer. Use of an AeroChamber Plus® spacer increases mean systemic (which equates to pulmonary absorption) bioavailability of fluticasone by 35% in healthy volunteers compared to administration of Flutiform inhaler via a pMDI alone. Flutiform inhaler – formoterol fumarate Following a single dose of Flutiform inhaler in healthy volunteers, a dose of 20 micrograms of formoterol fumarate from 2 actuations of Flutiform 250 /10 inhaler resulted in a mean maximum plasma formoterol concentration of 9.92 pg/ml within 6 minutes of inhalation. Following multiple doses, 20 micrograms of formoterol fumarate from 2 actuations of Flutiform 250 /10 inhaler resulted in a mean maximum plasma formoterol concentration of 34.4 pg/ml. Use of an AeroChamber Plus® spacer decreases mean systemic bioavailability of formoterol by 25% in healthy volunteers compared to administration of Flutiform inhaler via a pMDI alone. This is likely to be due to a reduction in absorption from the gastrointestinal tract when the spacer is used, offsetting the expected corresponding increase in pulmonary absorption. Distribution There is currently no plasma protein binding information specific to fluticasone propionate or formoterol fumarate from Flutiform inhaler. Biotransformation There are currently no data relating to the metabolism of fluticasone propionate or formoterol fumarate specifically from the inhalation of Flutiform inhaler. Elimination Fluticasone propionate Following inhalation of fluticasone propionate from 2 actuations of Flutiform 250 /10 inhaler, fluticasone propionate has a terminal elimination half-life of approximately 14.2 h. Formoterol fumarate Following inhalation of formoterol fumarate from 2 actuations of Flutiform 250 /10 inhaler, formoterol fumarate has a terminal elimination half-life of approximately 6.5 h. Less than 2% of a single dose of formoterol fumarate from Flutiform inhaler is excreted in the urine.

מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| אסטמה | ||||
| אסטמה | ||||
| אסטמה | ||||
| אסטמה | ||||
| אסטמה | ||||
| אסטמה | ||||
| אסטמה | ||||
| אסטמה | ||||
| אסטמה | ||||
| אסטמה |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
12/01/2014
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
08.08.22 - עלון לצרכן אנגלית 08.08.22 - עלון לצרכן עברית 08.08.22 - עלון לצרכן ערבית 07.06.23 - עלון לצרכן עברית 12.02.24 - עלון לצרכן עברית 05.04.24 - עלון לצרכן אנגלית 05.04.24 - עלון לצרכן עברית 05.04.24 - עלון לצרכן ערבית 29.03.21 - החמרה לעלון 19.04.21 - החמרה לעלון 07.06.23 - החמרה לעלון 12.02.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
פלוטיפורם 125/5