Quest for the right Drug
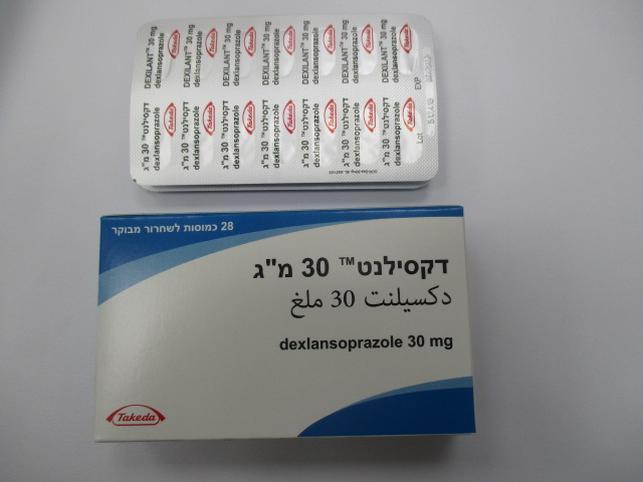
דקסילנט 30 מ"ג DEXILANT 30 MG (DEXLANSOPRAZOLE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
קפסולות בשחרור מושהה : MODIFIED RELEASE CAPSULES
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Indications : התוויות
2 THERAPEUTIC INDICATIONS Dexilant 30 mg is indicated in adults and in adolescents aged 12 to 17 years for the following: • Maintenance of healed erosive reflux oesophagitis and maintenance of relief of heartburn • Short-term treatment of heartburn and acid regurgitation associated with symptomatic non-erosive gastro-oesophageal reflux disease (GORD). Dexilant 60 mg is indicated in adults and in adolescents aged 12 to 17 years for the following: • Treatment of erosive reflux oesophagitis 3 DOSAGE AND ADMINISTRATION 3.1 Recommended Dosage in Adults and adolescents aged 12 to 17 years DEXILANT is available as capsules in 30 mg and 60 mg strengths for adult and adolescents aged 12 to 17 years use. Directions for use in each indication are summarized in Table 1. Table 1. Recommended DEXILANT Capsules dosage regimen by indication in Adults and adolescents aged 12 to 17 years Dosage of DEXILANT Indication Duration Capsules Treatment of One 60 mg capsule once erosive reflux Up to 8 weeks daily oesophagitis Maintenance of healed erosive reflux Controlled studies did not oesophagitis One 30 mg capsule once extend beyond 6 months in and daily adults and 16 weeks in maintenance of patients 12 to 17 years of relief of age heartburn Symptomatic One 30 mg capsule once non-erosive daily 4 weeks gastro- oesophageal reflux disease (GORD) 3.2 Dosage Adjustment in Patients with Hepatic Impairment For the treatment of erosive reflux oesophagitis For patients with moderate hepatic impairment (Child-Pugh Class B), the recommended dosage is 30 mg DEXILANT once daily for up to eight weeks. DEXILANT is not recommended in patients with severe hepatic impairment (Child- Pugh Class C) [see Use in Specific Populations (9.5)]. 3.3 Important Administration Information • Take without regard to food. • Missed doses: If a dose is missed, administer as soon as possible. However, if the next scheduled dose is due, do not take the missed dose, and take the next dose on time. Do not take two doses at one time to make up for a missed dose. • Swallow whole; do not chew. • For patients who have trouble swallowing capsules, DEXILANT capsules can be opened and administered with applesauce as follows: 1. Place one tablespoonful of applesauce into a clean container. 2. Open capsule. 3. Sprinkle intact granules on applesauce. 4. Swallow applesauce and granules immediately. Do not chew granules. Do not save the applesauce and granules for later use. • Alternatively, the capsule can be administered with water via oral syringe or nasogastric (NG) tube. Administration with Water in an Oral Syringe 1. Open the capsule and empty the granules into a clean container with 20 mL of water. 2. Withdraw the entire mixture into a syringe. 3. Gently swirl the syringe in order to keep granules from settling. 4. Administer the mixture immediately into the mouth. Do not save the water and granule mixture for later use. 5. Refill the syringe with 10 mL of water, swirl gently, and administer. 6. Refill the syringe again with 10 mL of water, swirl gently, and administer. Administration with Water via a NG Tube (≥16 French) 1. Open the capsule and empty the granules into a clean container with 20 mL of water. 2. Withdraw the entire mixture into a catheter-tip syringe. 3. Swirl the catheter-tip syringe gently in order to keep the granules from settling, and immediately inject the mixture through the NG tube into the stomach. Do not save the water and granule mixture for later use. 4. Refill the catheter-tip syringe with 10 mL of water, swirl gently, and flush the tube. 5. Refill the catheter-tip syringe again with 10 mL of water, swirl gently, and administer. 4 DOSAGE FORMS AND STRENGTHS DEXILANT modified-release capsules • 30 mg strength is an opaque, blue and gray capsule imprinted with TAP and “30”. • 60 mg strength is an opaque, blue capsule imprinted with TAP and “60”. 5 CONTRAINDICATIONS • DEXILANT is contraindicated in patients with known hypersensitivity to any component of the formulation [see Description (11)]. Hypersensitivity reactions, may include anaphylaxis, anaphylactic shock, angioedema, bronchospasm, acute tubulointerstitial nephritis and urticaria [see Warning and Precautions (6.2), Adverse Reactions (7)] • PPIs, including DEXILANT, are contraindicated with rilpivirine-containing products [see Drug Interactions (8)]. 6 WARNINGS AND PRECAUTIONS 6.1 Presence of Gastric Malignancy In adults, symptomatic response to therapy with DEXILANT does not preclude the presence of gastric malignancy. Consider additional follow-up and diagnostic testing in adult patients who have a suboptimal response or an early symptomatic relapse after completing treatment with a PPI. In older patients, also consider an endoscopy. 6.2 Acute Tubulointerstitial Nephritis Acute tubulointerstitial nephritis (TIN) has been observed in patients taking PPIs and may occur at any point during PPI therapy. Patients may present with varying signs and symptoms from symptomatic hypersensitivity reactions to non-specific symptoms of decreased renal function (e.g., malaise, nausea, anorexia). In reported case series, some patients were diagnosed on biopsy and in the absence of extra-renal manifestations (e.g., fever, rash or arthralgia). Discontinue DEXILANT and evaluate patients with suspected acute TIN [see Contraindications (5)]. 6.3 Clostridium difficile - Associated Diarrhea Published observational studies suggest that PPI therapy like DEXILANT may be associated with an increased risk of Clostridium difficile associated diarrhea, especially in hospitalized patients. This diagnosis should be considered for diarrhea that does not improve [see Adverse Reactions (7.2)]. Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated. 6.4 Bone Fracture Several published observational studies suggest that PPI therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist or spine. The risk of fracture was increased in patients who received high-dose, defined as multiple daily doses, and long-term PPI therapy (a year or longer). Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the conditions being treated. Patients at risk for osteoporosis-related fractures should be managed according to established treatment guidelines [see Dosage and Administration (3), Adverse Reactions (7.2)]. 6.5 Severe cutaneous adverse reactions Severe cutaneous adverse reactions, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), drug reaction with eosinophilia and systemic symptoms (DRESS), and acute generalized exanthematous pustulosis (AGEP) have been reported in association with the use of PPIs [see Adverse Reactions (7.2)]. Discontinue DEXILANT at the first signs or symptoms of severe cutaneous adverse reactions or other signs of hypersensitivity and consider further evaluation. 6.6 Cutaneous and Systemic Lupus Erythematosus Cutaneous lupus erythematosus (CLE) and systemic lupus erythematosus (SLE) have been reported in patients taking PPIs. These events have occurred as both new onset and an exacerbation of existing autoimmune disease. The majority of PPI-induced lupus erythematosus cases were CLE. The most common form of CLE reported in patients treated with PPIs was subacute CLE (SCLE) and occurred within weeks to years after continuous drug therapy in patients ranging from infants to the elderly. Generally, histological findings were observed without organ involvement. Systemic lupus erythematosus (SLE) is less commonly reported than CLE in patients receiving PPIs. PPI associated SLE is usually milder than non-drug induced SLE. Onset of SLE typically occurred within days to years after initiating treatment primarily in patients ranging from young adults to the elderly. The majority of patients presented with rash; however, arthralgia and cytopenia were also reported. Avoid administration of PPIs for longer than medically indicated. If signs or symptoms consistent with CLE or SLE are noted in patients receiving DEXILANT, discontinue the drug and refer the patient to the appropriate specialist for evaluation. Most patients improve with discontinuation of the PPI alone in four to 12 weeks. Serological testing (e.g., ANA) may be positive and elevated serological test results may take longer to resolve than clinical manifestations. 6.7 Cyanocobalamin (Vitamin B12) Deficiency Daily treatment with any acid-suppressing medications over a long period of time (e.g., longer than three years) may lead to malabsorption of cyanocobalamin (Vitamin B12) caused by hypo- or achlorhydria. Rare reports of cyanocobalamin deficiency occurring with acid-suppressing therapy have been reported in the literature. This diagnosis should be considered if clinical symptoms consistent with cyanocobalamin deficiency are observed in patients treated with DEXILANT. 6.8 Hypomagnesemia and Mineral Metabolism Hypomagnesemia, symptomatic and asymptomatic, has been reported rarely in patients treated with PPIs for at least three months, in most cases after a year of therapy. Serious adverse events include tetany, arrhythmias, and seizures. Hypomagnesemia may lead to hypocalcemia and/or hypokalemia and may exacerbate underlying hypocalcemia in at-risk patients In most patients, treatment of hypomagnesemia required magnesium replacement and discontinuation of the PPI. For patients expected to be on prolonged treatment or who take PPIs with medications such as digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), health care professionals may consider monitoring magnesium levels prior to initiation of PPI treatment and periodically [see Adverse Reactions (7.2)]. Consider monitoring magnesium and calcium levels prior to initiation of DEXILANT and periodically while on treatment in patients with a preexisting risk of hypocalcemia (e.g., hypoparathyroidism). Supplement with magnesium and/or calcium as necessary. If hypocalcemia is refractory to treatment, consider discontinuing the PPI. 6.9 Interactions with Investigations for Neuroendocrine Tumors Serum chromogranin A (CgA) levels increase secondary to drug-induced decreases in gastric acidity. The increased CgA level may cause false positive results in diagnostic investigations for neuroendocrine tumors. Healthcare providers should temporarily stop dexlansoprazole treatment at least 14 days before assessing CgA levels and consider repeating the test if initial CgA levels are high. If serial tests are performed (e.g. for monitoring), the same commercial laboratory should be used for testing, as reference ranges between tests may vary [see Drug Interactions (8), Clinical Pharmacology (12.2)]. 6.10 Interaction with Methotrexate Literature suggests that concomitant use of PPIs with methotrexate (primarily at high dose) may elevate and prolong serum levels of methotrexate and/or its metabolite, possibly leading to methotrexate toxicities. In high-dose methotrexate administration, a temporary withdrawal of the PPI may be considered in some patients [see Drug Interactions (8)]. 6.11 Fundic Gland Polyps PPI use is associated with an increased risk of fundic gland polyps that increases with long-term use, especially beyond one year. Most PPI users who developed fundic gland polyps were asymptomatic and fundic gland polyps were identified incidentally on endoscopy. Use the shortest duration of PPI therapy appropriate to the condition being treated. 7 ADVERSE REACTIONS The following serious adverse reactions are described below and elsewhere in labeling: • Acute Tubulointerstitial Nephritis [see Warnings and Precautions (6.2)] • Clostridium difficile - Associated Diarrhea [see Warnings and Precautions (6.3)] • Bone Fracture [see Warnings and Precautions (6.4)] • Severe Cutaneous Adverse Reactions [see Warnings and Precautions (6.5)] •Cutaneous and Systemic Lupus Erythematosus [see Warnings and Precautions (6.6)] •Cyanocobalamin (Vitamin B-12) Deficiency [see Warnings and Precautions (6.7)] • Hypomagnesemia and Mineral Metabolism [see Warnings and Precautions (6.8)] • Fundic Gland Polyps [see Warnings and Precautions (6.11)] 7.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. Adults The safety of DEXILANT was evaluated in 4548 adult patients in controlled and single-arm clinical trials, including 863 patients treated for at least six months and 203 patients treated for one year. Patients ranged in age from 18 to 90 years (median age 48 years), with 54% female, 85% Caucasian, 8% Black, 4% Asian, and 3% Other races. Six randomized controlled clinical trials were conducted for the treatment of erosive reflux oesophagitis, maintenance of healed erosive reflux oesophagitis, and symptomatic GORD, which included 896 patients on placebo, 455 patients on DEXILANT 30 mg, 2218 patients on DEXILANT 60 mg, and 1363 patients on lansoprazole 30 mg once daily. Common Adverse Reactions The most common adverse reactions (≥2%) that occurred at a higher incidence for DEXILANT than placebo in the controlled studies are presented in Table 2. Table 2. Common Adverse Reactions in Controlled Studies in Adults Placebo DEXILAN DEXILAN DEXILAN Lansoprazol T T T e Adverse (N=896 30 mg 60 mg Total 30 mg Reaction ) (N=455) (N=2218) (N=2621) (N=1363) % % % % % Diarrhea 2.9 5.1 4.7 4.8 3.2 Abdominal 3.5 3.5 4.0 4.0 2.6 Pain Nausea 2.6 3.3 2.8 2.9 1.8 Upper 0.8 2.9 1.7 1.9 0.8 Respirator y Tract Infection Vomiting 0.8 2.2 1.4 1.6 1.1 Flatulence 0.6 2.6 1.4 1.6 1.2 Adverse Reactions Resulting in Discontinuation In controlled clinical studies, the most common adverse reaction leading to discontinuation from DEXILANT was diarrhea (0.7%). Less Common Adverse Reactions Other adverse reactions that were reported in controlled studies at an incidence of less than 2% are listed below by body system: Blood and Lymphatic System Disorders: anemia, lymphadenopathy Cardiac Disorders: angina, arrhythmia, bradycardia, chest pain, edema, myocardial infarction, palpitation, tachycardia Ear and Labyrinth Disorders: ear pain, tinnitus, vertigo Endocrine Disorders: goiter Eye Disorders: eye irritation, eye swelling Gastrointestinal Disorders: abdominal discomfort, abdominal tenderness, abnormal feces, anal discomfort, Barrett’s esophagus, bezoar, bowel sounds abnormal, breath odor, colitis microscopic, colonic polyp, constipation, dry mouth, duodenitis, dyspepsia, dysphagia, enteritis, eructation, oesophagitis, gastric polyp, gastritis, gastroenteritis, gastrointestinal disorders, gastrointestinal hypermotility disorders, GORD, GI ulcers and perforation, hematemesis, hematochezia, hemorrhoids, impaired gastric emptying, irritable bowel syndrome, mucus stools, oral mucosal blistering, painful defecation, proctitis, paresthesia oral, rectal hemorrhage, retching General Disorders and Administration Site Conditions: adverse drug reaction, asthenia, chest pain, chills, feeling abnormal, inflammation, mucosal inflammation, nodule, pain, pyrexia Hepatobiliary Disorders: biliary colic, cholelithiasis, hepatomegaly Immune System Disorders: hypersensitivity Infections and Infestations: candida infections, influenza, nasopharyngitis, oral herpes, pharyngitis, sinusitis, viral infection, vulvo-vaginal infection Injury, Poisoning and Procedural Complications: falls, fractures, joint sprains, overdose, procedural pain, sunburn Laboratory Investigations: ALP increased, ALT increased, AST increased, bilirubin decreased/increased, blood creatinine increased, blood gastrin increased, blood glucose increased, blood potassium increased, liver function test abnormal, platelet count decreased, total protein increased, weight increase Metabolism and Nutrition Disorders: appetite changes, hypercalcemia, hypokalemia Musculoskeletal and Connective Tissue Disorders: arthralgia, arthritis, muscle cramps, musculoskeletal pain, myalgia Nervous System Disorders: altered taste, convulsion, dizziness, headaches, migraine, memory impairment, paresthesia, psychomotor hyperactivity, tremor, trigeminal neuralgia Psychiatric Disorders: abnormal dreams, anxiety, depression, insomnia, libido changes Renal and Urinary Disorders: dysuria, micturition urgency Reproductive System and Breast Disorders: dysmenorrhea, dyspareunia, menorrhagia, menstrual disorder Respiratory, Thoracic and Mediastinal Disorders: aspiration, asthma, bronchitis, cough, dyspnea, hiccups, hyperventilation, respiratory tract congestion, sore throat Skin and Subcutaneous Tissue Disorders: acne, dermatitis, erythema, pruritus, rash, skin lesion, urticaria Vascular Disorders: deep vein thrombosis, hot flush, hypertension Additional adverse reactions that were reported in a long-term single-arm trial and were considered related to DEXILANT by the treating physician included: anaphylaxis, auditory hallucination, B-cell lymphoma, bursitis, central obesity, cholecystitis acute, dehydration, diabetes mellitus, dysphonia, epistaxis, folliculitis, gout, herpes zoster, hyperlipidemia, hypothyroidism, increased neutrophils, MCHC decrease, neutropenia, rectal tenesmus, restless legs syndrome, somnolence, tonsillitis. Pediatrics The safety of DEXILANT was evaluated in controlled and single-arm clinical trials including 166 pediatric patients, 12 to 17 years of age for the treatment of symptomatic non-erosive GORD, treatment of erosive reflux oesophagitis, maintenance of healed erosive reflux oesophagitis and maintenance of relief of heartburn [see Clinical Studies (14.4)]. The adverse reaction profile was similar to that of adults. The most common adverse reactions that occurred in ≥ 5% of patients were headache, abdominal pain, diarrhea, nasopharyngitis and oropharyngeal pain. Other Adverse Reactions See the full prescribing information for lansoprazole for other adverse reactions not observed with DEXILANT. 7.2 Postmarketing Experience The following adverse reactions have been identified during post-approval use of DEXILANT. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Blood and Lymphatic System Disorders: autoimmune hemolytic anemia, idiopathic thrombocytopenic purpura Ear and Labyrinth Disorders: deafness Eye Disorders: blurred vision Gastrointestinal Disorders: oral edema, pancreatitis, fundic gland polyps General Disorders and Administration Site Conditions: facial edema Hepatobiliary Disorders: drug-induced hepatitis Immune System Disorders: anaphylactic shock (requiring emergency intervention), exfoliative dermatitis, Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN) (some fatal), DRESS, AGEP. Infections and Infestations: Clostridium difficile associated diarrhea Metabolism and Nutrition Disorders: hypomagnesemia, hypocalcemia, hypokalemia, hyponatremia Musculoskeletal System Disorders: bone fracture Nervous System Disorders: cerebrovascular accident, transient ischemic attack Renal and Urinary Disorders: acute renal failure Respiratory, Thoracic and Mediastinal Disorders: pharyngeal edema, throat tightness Skin and Subcutaneous Tissue Disorders: generalized rash, leukocytoclastic vasculitis Reporting suspected adverse reactions after authorization of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il 8 DRUG INTERACTIONS Tables 3 and 4 include drugs with clinically important drug interactions and interaction with diagnostics when administered concomitantly with DEXILANT and instructions for preventing or managing them. Consult the labeling of concomitantly used drugs to obtain further information about interactions with PPIs. Table 3. Clinically Relevant Interactions Affecting Drugs Co-Administered with DEXILANT and Interactions with Diagnostics Antiretrovirals The effect of PPIs on antiretroviral drugs is variable. The clinical importance Clinical and the mechanisms behind these interactions are not always known. Impact: • Decreased exposure of some antiretroviral drugs (e.g., rilpivirine, atazanavir, and nelfinavir) when used concomitantly with dexlansoprazole may reduce antiviral effect and promote the development of drug resistance. • Increased exposure of other antiretroviral drugs (e.g., saquinavir) when used concomitantly with dexlansoprazole may increase toxicity of the antiretroviral drugs. • There are other antiretroviral drugs which do not result in clinically relevant interactions with dexlansoprazole. Rilpivirine-containing products: Concomitant use with DEXILANT is Intervention: contraindicated [see Contraindications (5)]. See prescribing information. Atazanavir: See prescribing information for atazanavir for dosing information. Nelfinavir: Avoid concomitant use with DEXILANT. See prescribing information for nelfinavir. Saquinavir: See the prescribing information for saquinavir and monitor for potential saquinavir toxicities. Other antiretrovirals: See prescribing information. Warfarin Increased INR and prothrombin time in patients receiving PPIs and Clinical warfarin concomitantly. Increases in INR and prothrombin time may lead Impact: to abnormal bleeding and even death. Intervention: Monitor INR and prothrombin time. Dose adjustment of warfarin may be needed to maintain target INR range. See prescribing information for warfarin. Methotrexate Concomitant use of PPIs with methotrexate (primarily at high dose) may Clinical elevate and prolong serum concentrations of methotrexate and/or its Impact: metabolite hydroxymethotrexate, possibly leading to methotrexate toxicities. No formal drug interaction studies of high-dose methotrexate with PPIs have been conducted [see Warnings and Precautions (6.10)]. A temporary withdrawal of DEXILANT may be considered in some Intervention: patients receiving high-dose methotrexate. Digoxin Clinical Potential for increased exposure of digoxin. Impact: Monitor digoxin concentrations. Dose adjustment of digoxin may be needed Intervention: to maintain therapeutic drug concentrations. See prescribing information for digoxin. Drugs Dependent on Gastric pH for Absorption (e.g., iron salts, erlotinib, dasatinib, nilotinib, mycophenoloate mofetil, ketoconazole/itraconazole) Clinical Dexlansoprazole can reduce the absorption of other drugs due to its effect on Impact: reducing intragastric acidity. Mycophenolate mofetil (MMF): Co-administration of PPIs in healthy Intervention: subjects and in transplant patients receiving MMF has been reported to reduce the exposure to the active metabolite, mycophenolic acid (MPA), possibly due to a decrease in MMF solubility at an increased gastric pH. The clinical relevance of reduced MPA exposure on organ rejection has not been established in transplant patients receiving DEXILANT and MMF. Use DEXILANT with caution in transplant patients receiving MMF. See the prescribing information for other drugs dependent on gastric pH for absorption. Tacrolimus Clinical Potentially increased exposure of tacrolimus, especially in transplant patients Impact: who are intermediate or poor metabolizers of CYP2C19. Monitor tacrolimus whole blood trough concentrations. Dose adjustment Intervention: of tacrolimus may be needed to maintain therapeutic drug concentrations. See prescribing information for tacrolimus. Interactions with Investigations of Neuroendocrine Tumors CgA levels increase secondary to PPI-induced decreases in gastric acidity. The Clinical increased CgA level may cause false positive results in diagnostic Impact: investigations for neuroendocrine tumors [see Warnings and Precautions (6.9), Clinical Pharmacology (12.2)]. Temporarily stop DEXILANT treatment at least 14 days before assessing CgA Intervention: levels and consider repeating the test if initial CgA levels are high. If serial tests are performed (e.g. for monitoring), the same commercial laboratory should be used for testing, as reference ranges between tests may vary. Interaction with Secretin Stimulation Test Clinical Hyper-response in gastrin secretion in response to secretin stimulation test, Impact: falsely suggesting gastrinoma. Temporarily stop DEXILANT treatment at least 30 days before assessing to Intervention: allow gastrin levels to return to baseline [see Clinical Pharmacology (12.2)]. False Positive Urine Tests for THC Clinical There have been reports of false positive urine screening tests for Impact: tetrahydrocannabinol (THC) in patients receiving PPIs. Intervention: An alternative confirmatory method should be considered to verify positive results. Table 4. Clinically Relevant Interactions Affecting DEXILANT When Co-administered with Other Drugs and substances CYP2C19 or CYP3A4 Inducers Clinical Decreased exposure of dexlansoprazole when used concomitantly with Impact: strong inducers [see Clinical Pharmacology (12.3)]. St. John’s Wort, rifampin: Avoid concomitant use with Intervention: DEXILANT. Ritonavir-containing products: See prescribing information. CYP2C19 or CYP3A4 Inhibitors Increased exposure of dexlansoprazole is expected when used concomitantly Clinical with strong inhibitors [see Clinical Pharmacology (12.3)]. Impact: Intervention: Voriconazole: See prescribing information. 9 USE IN SPECIFIC POPULATIONS 9.1 Pregnancy Risk Summary There are no studies with dexlansoprazole use in pregnant women to inform a drug- associated risk. Dexlansoprazole is the R-enantiomer of lansoprazole, and published observational studies of lansoprazole use during pregnancy did not demonstrate an association of adverse pregnancy-related outcomes with lansoprazole (see Data). In animal reproduction studies, oral administration of lansoprazole to rats during organogenesis through lactation at 1.8 times the maximum recommended human dexlansoprazole dose produced reductions in the offspring in femur weight, femur length, crown-rump length and growth plate thickness (males only) on postnatal Day 21 (see Data). These effects were associated with reduction in body weight gain. Advise pregnant women of the potential risk to the fetus. The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively. Data Human Data Dexlansoprazole is the R-enantiomer of lansoprazole. Available data from published observational studies failed to demonstrate an association of adverse pregnancy- related outcomes and lansoprazole use. Methodological limitations of these observational studies cannot definitely establish or exclude any drug-associated risk during pregnancy. In a prospective study by the European Network of Teratology Information Services, outcomes from a group of 62 pregnant women administered median daily doses of 30 mg of lansoprazole were compared to a control group of 868 pregnant women who did not take any PPIs. There was no difference in the rate of major malformations between women exposed to PPIs and the control group, corresponding to a Relative Risk (RR)=1.04, [95% Confidence Interval (CI) 0.25-

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
