Quest for the right Drug
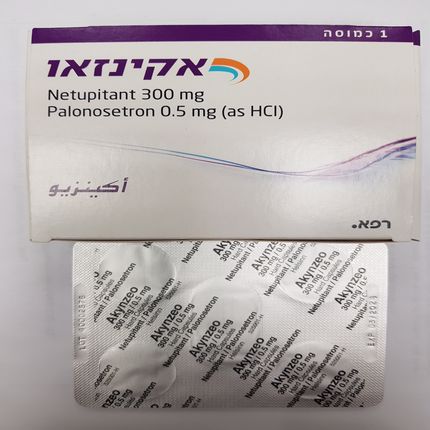
אקינזאו 300 מ"ג/0.50 מ"ג AKYNZEO 300mg/0.50mg (NETUPITANT, PALONOSETRON AS HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
קפסולות : CAPSULES
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antiemetics and antinauseants, serotonin (5-HT3) antagonists; ATC code: A04AA55 Mechanism of action Netupitant is a selective antagonist of human substance P/neurokinin 1 (NK1) receptors. Palonosetron is a 5-HT3 receptor antagonist with a strong binding affinity for this receptor and little or no affinity for other receptors. Chemotherapeutic substances produce nausea and vomiting by stimulating the release of serotonin from the enterochromaffin cells of the small intestine. Serotonin then activates 5-HT3 receptors located on vagal afferents to initiate the vomiting reflex. Delayed emesis has been associated with the activation of tachykinin family neurokinin 1 (NK1) receptors (broadly distributed in the central and peripheral nervous systems) by substance P. As shown in in vitro and in vivo studies, netupitant inhibits substance P mediated responses. Netupitant was shown to cross the blood brain barrier with a NK1 receptor occupancy of 92.5%, 86.5%, 85.0%, 78.0%, and 76.0% in striatum at 6, 24, 48, 72, and 96 hours, respectively, after administration of 300 mg netupitant. Clinical efficacy and safety Oral administration of Akynzeo in combination with dexamethasone has been shown to prevent acute and delayed nausea and vomiting associated with highly and moderately emetogenic cancer chemotherapy in two separate pivotal studies. Highly Emetogenic Chemotherapy (HEC) study In a multicenter, randomized, parallel, double-blind, controlled clinical study of 694 patients, the efficacy and safety of single doses of oral netupitant in combination with oral palonosetron was compared with a single oral dose of palonosetron in cancer patients receiving a chemotherapy regimen that included cisplatin (median dose = 75 mg/m2). The efficacy of Akynzeo was assessed in 135 patients who received a single oral dose (netupitant 300 mg and palonosetron 0.5 mg) and 136 patients who received oral palonosetron 0.5 mg alone. Treatment regimens for the Akynzeo and the palonosetron 0.5 mg arms are displayed in Table below. Table 2: Oral Antiemetic treatment regimen –– HEC study Treatment regimen Day 1 Days 2 to 4 Akynzeo Akynzeo (Netupitant 300 mg + Dexamethasone 8 mg once a Palonosetron 0.5 mg) day Dexamethasone 12 mg Palonosetron Palonosetron 0.5 mg Dexamethasone 8 mg twice Dexamethasone 20 mg a day The primary efficacy endpoint was complete response (CR) rate (defined as no emetic episodes, no rescue medication) within 120 hours (overall phase) after the start of the highly emetogenic chemotherapy administration. A summary of the key results from this study is shown in Table 3 below. Table 3: Proportion of patients receiving cisplatin chemotherapy responding by treatment group and phase Palonosetron Akynzeo 0.5 mg N=135 N=136 % % p-value Primary endpoint Complete response Overall phase§ 89.6 76.5 0.004 Major secondary endpoints Complete response Acute phase‡ 98.5 89.7 0.007 Delayed phase † 90.4 80.1 0.018 No emesis Acute phase 98.5 89.7 0.007 Delayed phase 91.9 80.1 0.006 Overall phase 91.1 76.5 0.001 No significant nausea Acute phase 98.5 93.4 0.050 Delayed phase 90.4 80.9 0.004 Overall phase 89.6 79.4 0.021 ‡ Acute phase: 0 to 24 hours post-cisplatin treatment. † Delayed phase: 25 to 120 hours post-cisplatin treatment. § Overall: 0 to 120 hours post-cisplatin treatment. Moderately Emetogenic Chemotherapy (MEC) study In a multicenter, randomized, parallel, double-blind, active-controlled, superiority study, the efficacy and safety of a single oral dose of Akynzeo was compared with a single oral dose of palonosetron 0.5 mg in cancer patients scheduled to receive the first cycle of an anthracycline and cyclophosphamide regimen for the treatment of a solid malignant tumor. At the time of the study, anthracycline-cyclophosphamide containing chemotherapy regimens were considered to be moderately emetogenic. Recent guidance has updated these regimens to highly emetogenic. All patients received a single oral dose of dexamethasone. Table 4: Oral Antiemetic treatment regimen – MEC study Treatment Day 1 Days 2 to 3 regimen Akynzeo Akynzeo Netupitant 300 mg No antiemetic treatment Palonosetron 0.5 mg Dexamethasone 12 mg Palonosetron Palonosetron 0.5 mg No antiemetic treatment Dexamethasone 20 mg After completion of cycle 1, patients had the option to participate in a multiple-cycle extension, receiving the same treatment as assigned in cycle 1. There was no pre-specified limit of the number of repeat consecutive cycles for any patient. A total of 1450 patients (Akynzeo n=725; Palonosetron n=725) received study medication. Of these, 1438 patients (98.8%) completed cycle 1 and 1286 patients (88.4%) continued treatment in the multiple-cycle extension. A total of 907 patients (62.3%) completed the multiple-cycle extension up to a maximum of eight treatment cycles. A total of 724 patients (99.9%) were treated with cyclophosphamide. All patients were additionally treated with either doxorubicin (68.0%) or epirubicin (32.0%). The primary efficacy endpoint was the CR rate in the delayed phase, 25-120 hours after the start of the chemotherapy administration. A summary of the key results from this study is shown in Table below. Table 5: Proportion of patients receiving anthracycline and cyclophosphamide chemotherapy responding by treatment group and phase – cycle 1 Akynzeo Palonosetron 0.5 mg N=724 N=725 % % p-value* Primary endpoint Complete response Delayed phase† 76.9 69.5 0.001 Major secondary endpoints Complete response Acute phase‡ 88.4 85.0 0.047 § Overall phase 74.3 66.6 0.001 No emesis Acute phase 90.9 87.3 0.025 Delayed phase 81.8 75.6 0.004 Overall phase 79.8 72.1 <0.001 No significant nausea Acute phase 87.3 87.9 N.S. Delayed phase 76.9 71.3 0.014 Overall phase 74.6 69.1 0.020 * p-value from Cochran-Mantel-Haenszel test, stratified by age class and region. ‡ Acute phase: 0 to 24 hours after anthracycline and cyclophosphamide regimen † Delayed phase: 25 to 120 hours after anthracycline and cyclophosphamide regimen § Overall: 0 to 120 hours after anthracycline and cyclophosphamide regimen Patients continued into the Multiple-Cycle extension for up to 7 additional cycles of chemotherapy. Antiemetic activity of Akynzeo was maintained throughout repeat cycles for those patients continuing in each of the multiple cycles. The impact of nausea and vomiting on patients’ daily lives was assessed using the Functional Living Index–Emesis (FLIE). The proportion of patients with Overall no impact on daily life was 6.3% higher (p value =0.005) in the Akynzeo group (78.5%) than in the palonosetron group (72.1%). Multiple-cycle safety study in patients receiving either Highly Emetogenic Chemotherapy or Moderately Emetogenic Chemotherapy In a separate study, a total of 413 patients undergoing initial and repeat cycles of chemotherapy (including carboplatin, cisplatin, oxaliplatin, and doxorubicin regimens), were randomized to receive either Akynzeo (n=309) or aprepitant and palonosetron (n=104). Safety and efficacy were maintained throughout all cycles. Paediatric population No data available.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption Netupitant Absolute netupitant bioavailability data are not available in humans; based on data from two studies with intravenous netupitant, the bioavailability in humans is estimated to be greater than 60%. In single dose oral studies, netupitant was measurable in plasma between 15 minutes and 3 hours after dosing. Plasma concentrations followed a first order absorption process and reached Cmax in approximately 5 hours. There was a supra-proportional increase in Cmax and AUC parameters for doses from 10 mg to 300 mg. In 82 healthy subjects given a single oral dose of netupitant 300 mg, maximum plasma netupitant concentration (Cmax) was 486 ±268 ng/mL (mean ± SD) and median time to maximum concentration (Tmax) was 5.25 hours, the AUC was 15032 ± 6858 h.ng/mL. In a pooled analysis, females had a higher netupitant exposure compared to males; there was a 1.31-fold increase in Cmax, a 1.02 fold increase for AUC and a 1.36 fold increase in half-life. Netupitant AUC0-∞ and Cmax increased by 1.1 fold and 1.2 fold, respectively, after a high fat meal. Palonosetron Following oral administration, palonosetron is well absorbed with its absolute bioavailability reaching 97%. After single oral doses using buffered solution mean maximum palonosetron concentrations (Cmax) and area under the concentration-time curve (AUC0-∞) were dose proportional over the dose range of 3.0 to 80 mcg/kg in healthy subjects. In 36 healthy male and female subjects given a single oral dose of 0.5 mg palonosetron, maximum plasma concentration (Cmax) was 0.81 ± 1.66 ng/mL (mean ± SD) and time to maximum concentration (Tmax) was 5.1 ± 1.7 hours. In female subjects (n=18), the mean AUC was 35% higher and the mean Cmax was 26% higher than in male subjects (n=18). In 12 cancer patients given a single oral dose of palonosetron 0.5 mg one hour prior to chemotherapy, Cmax was 0.93 ± 0.34 ng/mL and Tmax was 5.1 ± 5.9 hours. The AUC was 30% higher in cancer patients than in healthy subjects. A high fat meal did not affect the Cmax and AUC of oral palonosetron. Distribution Netupitant After a single oral 300 mg dose administration in cancer patients, netupitant disposition was characterised by a two compartment model with an estimated median systemic clearance of 20.5 L/h and a large distribution volume in the central compartment (486 L). Human plasma protein binding of netupitant and its two major metabolites M1 and M3 is > 99% at concentrations ranging from 10 to 1500 ng/mL. The third major metabolite, M2, is > 97% bound to plasma proteins. Palonosetron Palonosetron has a volume of distribution of approximately 8.3 ± 2.5 L/kg. Approximately 62% of palonosetron is bound to plasma proteins. Biotransformation Netupitant Three metabolites have been detected in human plasma at netupitant oral doses of 30 mg and higher (the desmethyl derivative, M1; the N-oxide derivative, M2; the OH-methyl derivative, M3). In vitro metabolism studies have suggested that CYP3A4 and, to a lesser extent, CYP2D6 and CYP2C9 are involved in the metabolism of netupitant. After administration of a single oral dose of 300 mg netupitant, mean plasma netupitant/plasma radioactivity ratios ranged from 0.13 to 0.49 over 96 h post-dose. The ratios were time dependent with values decreasing gradually beyond 24 h post-dose, indicating that netupitant is being rapidly metabolized. Mean Cmax was approximately 11%, 47% and 16% of the parent for M1, M2 and M3 respectively; M2 had the lowest AUC relative to the parent (14%) whereas M1 and M3 AUC were approximately 29% and 33% of the parent, respectively. M1, M2 and M3 metabolites were all shown to be pharmacologically active in an animal pharmacodynamic model, where M3 was most potent and M2 least active. Palonosetron Palonosetron is eliminated by multiple routes with approximately 50% metabolized to form two primary metabolites: N-oxide-palonosetron and 6-S-hydroxy-palonosetron. These metabolites each have less than 1% of the 5-HT3 receptor antagonist activity of palonosetron. In vitro metabolism studies have suggested that CYP2D6 and to a lesser extent, CYP3A4 and CYP1A2 are involved in the metabolism of palonosetron. However, clinical pharmacokinetic parameters are not significantly different between poor and extensive metabolizers of CYP2D6 substrates. Elimination Netupitant Following administration of a single dose of Akynzeo, netupitant is eliminated from the body in a multi-exponential fashion, with an apparent mean elimination half-life of 88 hours in cancer patients. Renal clearance is not a significant elimination route for netupitant-related entities. The mean fraction of an oral dose of netupitant excreted unchanged in urine is less than 1%; a total of 3.95% and 70.7% of the radioactive dose was recovered in the urine and faeces, respectively. Approximately half the radioactivity administered orally as [14C]netupitant was recovered from urine and faeces within 120 h of dosing. Elimination via both routes was estimated to be complete by Day 29-30 post-dose. Palonosetron Following administration of a single oral 0.75 mg dose of [14C]palonosetron to six healthy subjects, 85% to 93% of the total radioactivity was excreted in urine, and 5% to 8% was eliminated in faeces. The amount of unchanged palonosetron excreted in the urine represented approximately 40% of the administered dose. In healthy subjects given palonosetron capsules 0.5 mg, the terminal elimination half-life (t½) of palonosetron was 37 ± 12 hours (mean ± SD), and in cancer patients, t½ was 48 ± 19 hours. After a single dose of approximately 0.75 mg intravenous palonosetron, the total body clearance of palonosetron in healthy subjects was 160 ± 35 mL/h/kg (mean ± SD) and renal clearance was 66.5± 18.2 mL/h/kg. Special populations Hepatic Impairment Netupitant Maximum concentrations and total exposure of netupitant were increased in subjects with mild (n=8), moderate (n=8), and severe (n=2) hepatic impairment compared to matching healthy subjects, although there was pronounced individual variability in both hepatically-impaired and healthy subjects. Exposure to netupitant (Cmax, AUC0-t and AUC0-∞) compared to matching healthy subjects was 11%, 28% and 19% higher in mild and 70%, 88% and 143% higher in moderate hepatically- impaired subjects, respectively. As such, no dosage adjustment is necessary for patients with mild to moderate hepatic impairment. Limited data exist in patients with severe hepatic impairment (Child Pugh score ≥9). Palonosetron Hepatic impairment does not significantly affect total body clearance of palonosetron compared to the healthy subjects. While the terminal elimination half-life and mean systemic exposure of palonosetron is increased in the subjects with severe hepatic impairment, this does not warrant dose reduction. Renal impairment Netupitant No specific studies were performed to evaluate netupitant in patients with renal impairment. In the ADME trial, less than 5% of all netupitant-related material was excreted in urine and less than 1% of the netupitant dose was eliminated unchanged in the urine and therefore any accumulation of netupitant or metabolites after a single dose would be negligible. Furthermore, the population PK study showed no correlation between PK parameters of netupitant and markers of renal dysfunction. Palonosetron Mild to moderate renal impairment does not significantly affect palonosetron PK parameters. Total systemic exposure to intravenous palonosetron increased by approximately 28% in patients with severe impairment relative to healthy subjects. In a population PK study, patients with a reduced creatinine clearance (CLCR) also had a reduced palonosetron clearance, but this reduction would not result in a significant change in palonosetron exposure. Therefore, Akynzeo can be administered without dosage adjustment in patients with renal impairment. Neither netupitant nor palonosetron have been evaluated in patients with end-stage renal disease.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול למניעת הקאות או בחילות הנובעות מכימותרפיה במקרים האלה:1. טיפול בכימותרפיה בעלת פוטנציאל אמטוגני גבוה.2. טיפול בכימותרפיה בעלת פוטנציאל אמטוגני בינוני, בחולה בו טיפול בתרופה ממשפחת ה- serotonin 5-HT3 receptor antagonists במחזור הטיפול הקודם לא הביא לשליטה מיטבית בבחילות ובהקאות. ב. התרופה לא תינתן בשילוב עם Aprepitant.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| "א. התרופה תינתן לטיפול למניעת הקאות או בחילות הנובעות מכימותרפיה במקרים האלה: 1. טיפול בכימותרפיה בעלת פוטנציאל אמטוגני גבוה. 2. טיפול בכימותרפיה בעלת פוטנציאל אמטוגני בינוני, בחולה בו טיפול בתרופה ממשפחת ה- serotonin 5-HT3 receptor antagonists במחזור הטיפול הקודם לא הביא לשליטה מיטבית בבחילות ובהקאות. ב. התרופה לא תינתן בשילוב עם Aprepitant. " |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
21/01/2016
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
