Quest for the right Drug
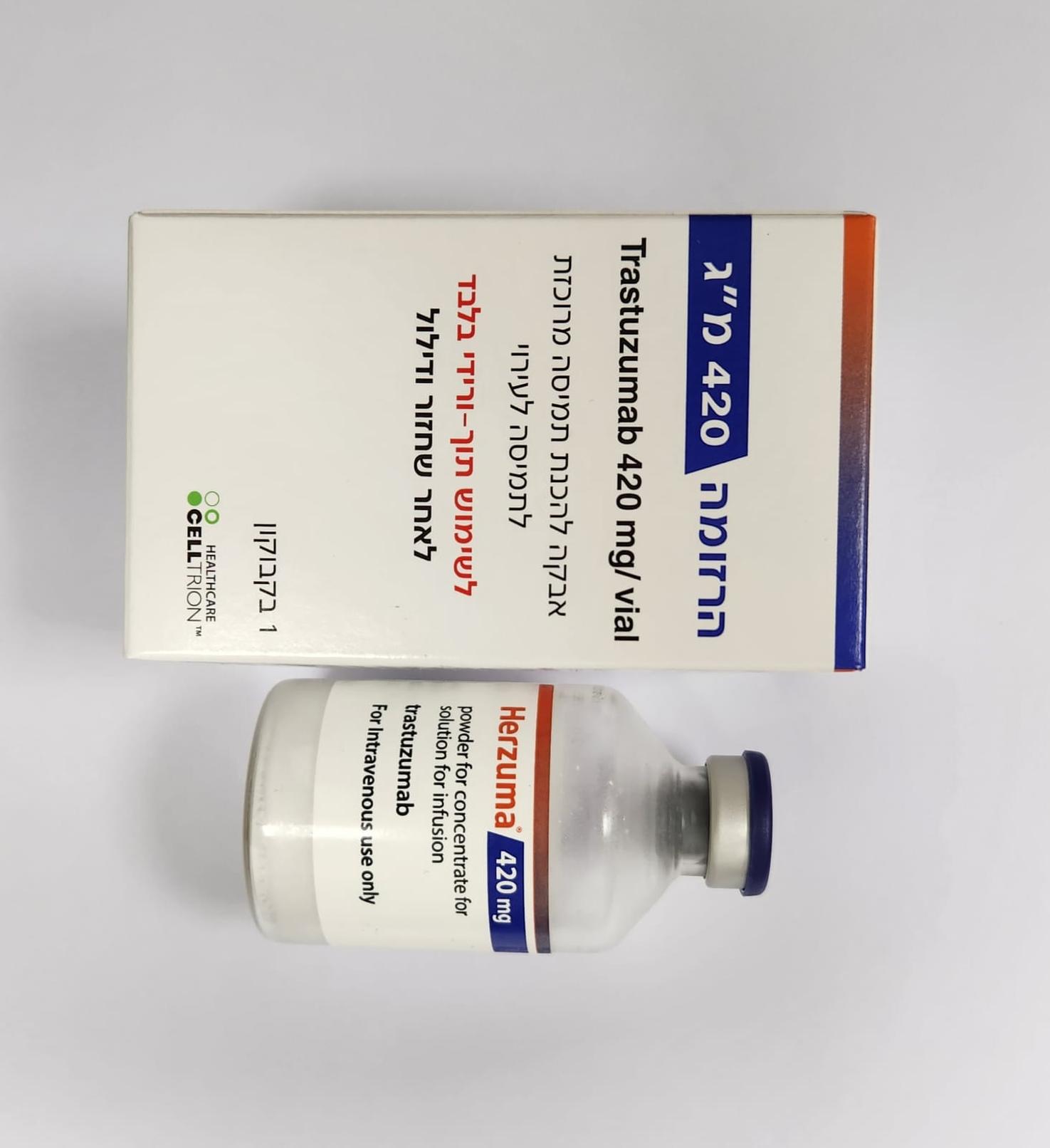
הרזומה 420 מ"ג HERZUMA 420 MG (TRASTUZUMAB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה להכנת תמיסה מרוכזת לעירוי : POWDER FOR CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4. Special warnings and precautions for use Traceability In order to improve the traceability of biological medicinal products, the trade name and the batch number of the administered product should be clearly recorded. HER2 testing must be performed in a specialised laboratory which can ensure adequate validation of the testing procedures (see section 5.1). Currently no data from clinical trials are available on re-treatment of patients with previous exposure to trastuzumab in the adjuvant setting. Cardiac dysfunction General considerations Patients treated with Herzuma are at increased risk for developing CHF (New York Heart Association [NYHA] Class II-IV) or asymptomatic cardiac dysfunction. These events have been observed in patients receiving trastuzumab therapy alone or in combination with paclitaxel or docetaxel, particularly following anthracycline (doxorubicin or epirubicin) containing chemotherapy. These may be moderate to severe and have been associated with death (see section 4.8). In addition, caution should be exercised in treating patients with increased cardiac risk, e.g. hypertension, documented coronary artery disease, CHF, LVEF of <55%, older age. All candidates for treatment with Herzuma, but especially those with prior anthracycline and cyclophosphamide (AC) exposure, should undergo baseline cardiac assessment including history and physical examination, electrocardiogram (ECG), echocardiogram, and/or multigated acquisition (MUGA) scan or magnetic resonance imaging. Monitoring may help to identify patients who develop cardiac dysfunction. Cardiac assessments, as performed at baseline, should be repeated every 3 months during treatment and every 6 months following discontinuation of treatment until 24 months from the last administration of Herzuma. A careful risk-benefit assessment should be made before deciding to treat with Herzuma. Trastuzumab may persist in the circulation for up to 7 months after stopping Herzuma treatment based on population pharmacokinetic analysis of all available data (see section 5.2). Patients who receive anthracyclines after stopping Herzuma may possibly be at increased risk of cardiac dysfunction. If possible, physicians should avoid anthracycline-based therapy for up to 7 months after stopping Herzuma. If anthracyclines are used, the patient’s cardiac function should be monitored carefully. Formal cardiological assessment should be considered in patients in whom there are cardiovascular concerns following baseline screening. In all patients cardiac function should be monitored during treatment (e.g. every 12 weeks). Monitoring may help to identify patients who develop cardiac dysfunction. Patients who develop asymptomatic cardiac dysfunction may benefit from more frequent monitoring (e.g. every 6-8 weeks). If patients have a continued decrease in left ventricular function, but remain asymptomatic, the physician should consider discontinuing therapy if no clinical benefit of Herzuma therapy has been seen. The safety of continuation or resumption of trastuzumab in patients who experience cardiac dysfunction has not been prospectively studied. If LVEF percentage drops ≥10 points from baseline AND to below 50%, treatment should be suspended and a repeat LVEF assessment performed within approximately 3 weeks. If LVEF has not improved, or declined further, or symptomatic CHF has developed, discontinuation of Herzuma should be strongly considered, unless the benefits for the individual patient are deemed to outweigh the risks. All such patients should be referred for assessment by a cardiologist and followed up. If symptomatic cardiac failure develops during Herzuma therapy, it should be treated with standard medicinal products for CHF. Most patients who developed CHF or asymptomatic cardiac dysfunction in pivotal trials improved with standard CHF treatment consisting of an angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor blocker (ARB) and a beta-blocker. The majority of patients with cardiac symptoms and evidence of a clinical benefit of trastuzumab treatment continued on therapy without additional clinical cardiac events. Metastatic breast cancer Herzuma and anthracyclines should not be given concurrently in combination in the MBC setting. Patients with MBC who have previously received anthracyclines are also at risk of cardiac dysfunction with Herzuma treatment, although the risk is lower than with concurrent use of Herzuma and anthracyclines. Early breast cancer For patients with EBC, cardiac assessments, as performed at baseline, should be repeated every 3 months during treatment and every 6 months following discontinuation of treatment until 24 months from the last administration of Herzuma. In patients who receive anthracycline containing chemotherapy further monitoring is recommended, and should occur yearly up to 5 years from the last administration of Herzuma, or longer if a continuous decrease of LVEF is observed. Patients with history of myocardial infarction (MI), angina pectoris requiring medical treatment, history of or existing CHF (NYHA Class II –IV), LVEF of < 55%, other cardiomyopathy, cardiac arrhythmia requiring medical treatment, clinically significant cardiac valvular disease, poorly controlled hypertension (hypertension controlled by standard medical treatment eligible), and hemodynamic effective pericardial effusion were excluded from adjuvant and neoadjuvant EBC pivotal trials with trastuzumab and therefore treatment cannot be recommended in such patients. Adjuvant treatment Herzuma and anthracyclines should not be given concurrently in combination in the adjuvant treatment setting. In patients with EBC an increase in the incidence of symptomatic and asymptomatic cardiac events was observed when trastuzumab was administered after anthracycline-containing chemotherapy compared to administration with a non-anthracycline regimen of docetaxel and carboplatin and was more marked when trastuzumab was administered concurrently with taxanes than when administered sequentially to taxanes. Regardless of the regimen used, most symptomatic cardiac events occurred within the first 18 months. In one of the 3 pivotal studies conducted in which a median follow-up of 5.5 years was available (BCIRG006) a continuous increase in the cumulative rate of symptomatic cardiac or LVEF events was observed in patients who were administered trastuzumab concurrently with a taxane following anthracycline therapy up to 2.37% compared to approximately 1% in the two comparator arms (anthracycline plus cyclophosphamide followed by taxane and taxane, carboplatin and trastuzumab). Risk factors for a cardiac event identified in four large adjuvant studies included advanced age (> 50 years), low LVEF (<55%) at baseline, prior to or following the initiation of paclitaxel treatment, decline in LVEF by 10-15 points, and prior or concurrent use of anti-hypertensive medicinal products. In patients receiving trastuzumab after completion of adjuvant chemotherapy, the risk of cardiac dysfunction was associated with a higher cumulative dose of anthracycline given prior to initiation of trastuzumab and a body mass index (BMI) >25 kg/m2. Benzyl alcohol as a preservative in Bacteriostatic Water for Injection has been associated with toxicity in neonates and children up to 3 years old. When administering Herzuma to a patient with a known sensitivity to benzyl alcohol, Herzuma should be reconstituted with Water for Injection, and only one dose per Herzuma vial should be used. Any unused portion must be discarded. Neoadjuvant-adjuvant treatment In patients with EBC eligible for neoadjuvant-adjuvant treatment, Herzuma should be used concurrently with anthracyclines only in chemotherapy-naive patients and only with low-dose anthracycline regimens i.e. maximum cumulative doses: of doxorubicin 180 mg/m2 or epirubicin 360 mg/m2. If patients have been treated concurrently with a full course of low-dose anthracyclines and Herzuma in the neoadjuvant setting, no additional cytotoxic chemotherapy should be given after surgery. In other situations, the decision on the need for additional cytotoxic chemotherapy is determined based on individual factors. Experience of concurrent administration of trastuzumab with low dose anthracycline regimens is currently limited to two trials (MO16432 and BO22227). In the pivotal trial MO16432, trastuzumab was administered concurrently with neoadjuvant chemotherapy containing three cycles of doxorubicin (cumulative dose 180 mg/m2). The incidence of symptomatic cardiac dysfunction was 1.7% in the trastuzumab arm. In the pivotal trial BO22227, trastuzumab was administered concurrently with neoadjuvant chemotherapy that contained four cycles of epirubicin (cumulative dose 300 mg/m2); at a median follow-up exceeding 70 months, the incidence of cardiac failure/congestive cardiac failure was 0.3% in the trastuzumab intravenous arm. Clinical experience is limited in patients above 65 years of age. Infusion-related reactions (IRRs) and hypersensitivity Serious IRRs to trastuzumab infusion including dyspnoea, hypotension, wheezing, hypertension, bronchospasm, supraventricular tachyarrhythmia, reduced oxygen saturation, anaphylaxis, respiratory distress, urticaria and angioedema have been reported (see section 4.8). Pre-medication may be used to reduce risk of occurrence of these events. The majority of these events occur during or within 2.5 hours of the start of the first infusion. Should an infusion reaction occur the infusion should be discontinued or the rate of infusion slowed and the patient should be monitored until resolution of all observed symptoms (see section 4.2). These symptoms can be treated with an analgesic/antipyretic such as meperidine or paracetamol, or an antihistamine such as diphenhydramine. The majority of patients experienced resolution of symptoms and subsequently received further infusions of trastuzumab. Serious reactions have been treated successfully with supportive therapy such as oxygen, beta- agonists, and corticosteroids. In rare cases, these reactions are associated with a clinical course culminating in a fatal outcome. Patients experiencing dyspnoea at rest due to complications of advanced malignancy and comorbidities may be at increased risk of a fatal infusion reaction. Therefore, these patients should not be treated with Herzuma (see section 4.3). Initial improvement followed by clinical deterioration and delayed reactions with rapid clinical deterioration have also been reported. Fatalities have occurred within hours and up to one week following infusion. On very rare occasions, patients have experienced the onset of infusion symptoms and pulmonary symptoms more than six hours after the start of the trastuzumab infusion. Patients should be warned of the possibility of such a late onset and should be instructed to contact their physician if these symptoms occur. Pulmonary events Severe pulmonary events have been reported with the use of trastuzumab in the post-marketing setting (see section 4.8). These events have occasionally been fatal. In addition, cases of interstitial lung disease including lung infiltrates, acute respiratory distress syndrome, pneumonia, pneumonitis, pleural effusion, respiratory distress, acute pulmonary oedema and respiratory insufficiency have been reported. Risk factors associated with interstitial lung disease include prior or concomitant therapy with other anti-neoplastic therapies known to be associated with it such as taxanes, gemcitabine, vinorelbine and radiation therapy. These events may occur as part of an infusion-related reaction or with a delayed onset. Patients experiencing dyspnoea at rest due to complications of advanced malignancy and comorbidities may be at increased risk of pulmonary events. Therefore, these patients should not be treated with Herzuma (see section 4.3). Caution should be exercised for pneumonitis, especially in patients being treated concomitantly with taxanes.
Effects on Driving

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
