Quest for the right Drug
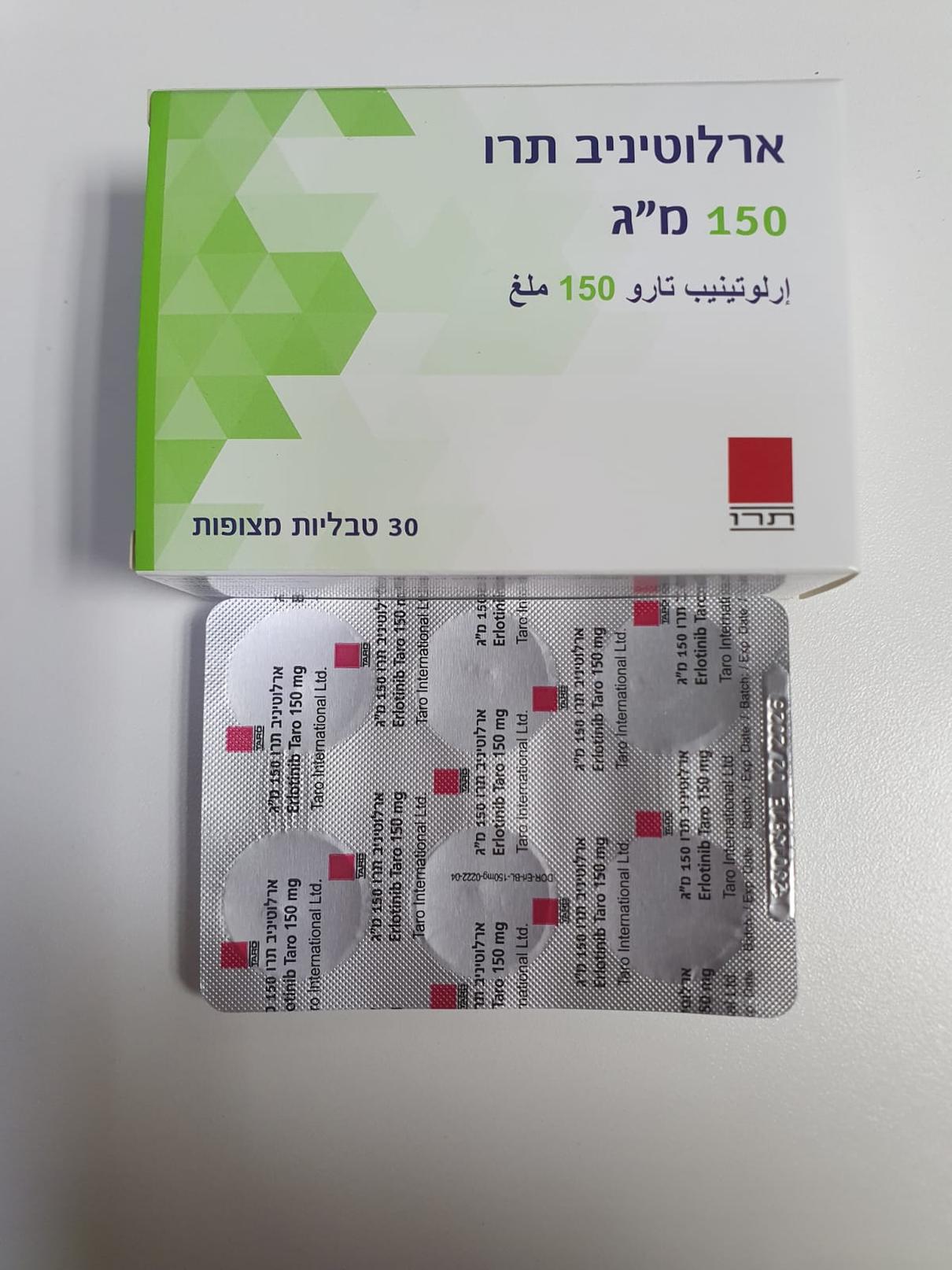
ארלוטיניב תרו 150 מ"ג ERLOTINIB TARO 150 MG (ERLOTINIB AS HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Assessment of EGFR mutation status When considering the use of ERLOTINIB TARO as a first line or maintenance treatment for locally advanced or metastatic NSCLC, it is important that the EGFR mutation status of a patient is determined. A validated, robust, reliable and sensitive test with a prespecified positivity threshold and demonstrated utility for the determination of EGFR mutation status, using either tumor DNA derived from a tissue sample or circulating free DNA (cfDNA) obtained from a blood (plasma) sample, should be performed according to local medical practice. If a plasma-based cfDNA test is used and the result is negative for activating mutations, perform a tissue test wherever possible due to the potential for false negative results from a plasma-based test. Smokers Current smokers should be advised to stop smoking, as plasma concentrations of erlotinib in smokers as compared to non-smokers are reduced. The degree of reduction is likely to be clinically significant (see sections 4.2, 4.5, 5.1, and 5.2). Interstitial Lung Disease Cases of interstitial lung disease (ILD)-like events, including fatalities, have been reported uncommonly in patients receiving erlotinib for treatment of non-small cell lung cancer (NSCLC), pancreatic cancer or other advanced solid tumours. In the pivotal study BR.21 in NSCLC, the incidence of ILD (0.8%) was the same in both the placebo and erlotinib groups. In a meta-analysis of NSCLC randomised controlled clinical trials (excluding phase I and single-arm phase II studies due to lack of control groups), the incidence of ILD-like events was 0.9% on erlotinib compared to 0.4% in patients in the control arms. In the pancreatic cancer study in combination with gemcitabine, the incidence of ILD-like events was 2.5% in the erlotinib plus gemcitabine group versus 0.4% in the placebo plus gemcitabine treated group. Reported diagnoses in patients suspected of having ILD-like events included pneumonitis, radiation pneumonitis, hypersensitivity pneumonitis, interstitial pneumonia, interstitial lung disease, obliterative bronchiolitis, pulmonary fibrosis, Acute Respiratory Distress Syndrome (ARDS), alveolitis, and lung infiltration. Symptoms started from a few days to several months after initiating erlotinib therapy. Confounding or contributing factors such as concomitant or prior chemotherapy, prior radiotherapy, pre-existing parenchymal lung disease, metastatic lung disease, or pulmonary infections were frequent. A higher incidence of ILD (approximately 5% with a mortality rate of 1.5%) is seen among patients in studies conducted in Japan. In patients who develop acute onset of new and/or progressive unexplained pulmonary symptoms such as dyspnoea, cough and fever, ERLOTINIB TARO therapy should be interrupted pending diagnostic evaluation. Patients treated concurrently with erlotinib and gemcitabine should be monitored carefully for the possibility to develop ILD-like toxicity. If ILD is diagnosed, ERLOTINIB TARO should be discontinued and appropriate treatment initiated as necessary (see section 4.8). Diarrhoea, dehydration, electrolyte imbalance and renal failure Diarrhoea (including very rare cases with a fatal outcome) has occurred in approximately 50% of patients on erlotinib and moderate or severe diarrhoea should be treated with e.g. loperamide. In some cases dose reduction may be necessary. In the clinical studies doses were reduced by 50 mg steps. Dose reductions by 25 mg steps have not been investigated. In the event of severe or persistent diarrhoea, nausea, anorexia, or vomiting associated with dehydration, ERLOTINIB TARO therapy should be interrupted and appropriate measures should be taken to treat the dehydration (see section 4.8). There have been rare reports of hypokalaemia and renal failure (including fatalities). Some cases were secondary to severe dehydration due to diarrhoea, vomiting and/or anorexia, while others were confounded by concomitant chemotherapy. In more severe or persistent cases of diarrhoea, or cases leading to dehydration, particularly in groups of patients with aggravating risk factors (especially concomitant chemotherapy and other medications, symptoms or diseases or other predisposing conditions including advanced age), ERLOTINIB TARO therapy should be interrupted and appropriate measures should be taken to intensively rehydrate the patients intravenously. In addition, renal function and serum electrolytes including potassium should be monitored in patients at risk of dehydration. Hepatitis, hepatic failure Rare cases of hepatic failure (including fatalities) have been reported during use of erlotinib. Confounding factors have included pre-existing liver disease or concomitant hepatotoxic medications. Therefore, in such patients, periodic liver function testing should be considered. ERLOTINIB TARO dosing should be interrupted if changes in liver function are severe (see section 4.8). ERLOTINIB TARO is not recommended for use in patients with severe hepatic dysfunction. Gastrointestinal perforation Patients receiving erlotinib are at increased risk of developing gastrointestinal perforation, which was observed uncommonly (including some cases with a fatal outcome). Patients receiving concomitant anti- angiogenic agents, corticosteroids, NSAIDs, and/or taxane based chemotherapy, or who have prior history of peptic ulceration or diverticular disease are at increased risk. ERLOTINIB TARO should be permanently discontinued in patients who develop gastrointestinal perforation (see section 4.8). Bullous and exfoliative skin disorders Bullous, blistering and exfoliative skin conditions have been reported, including very rare cases suggestive of Stevens-Johnson syndrome/Toxic epidermal necrolysis, which in some cases were fatal (see section 4.8). ERLOTINIB TARO treatment should be interrupted or discontinued if the patient develops severe bullous, blistering or exfoliating conditions. Patients with bullous and exfoliative skin disorders should be tested for skin infection and treated according to local management guidelines. Ocular disorders Patients presenting with signs and symptoms suggestive of keratitis such as acute or worsening: eye inflammation, lacrimation, light sensitivity, blurred vision, eye pain and/or red eye should be referred promptly to an ophthalmology specialist. If a diagnosis of ulcerative keratitis is confirmed, treatment with ERLOTINIB TARO should be interrupted or discontinued. If keratitis is diagnosed, the benefits and risks of continuing treatment should be carefully considered. ERLOTINIB TARO should be used with caution in patients with a history of keratitis, ulcerative keratitis or severe dry eye. Contact lens use is also a risk factor for keratitis and ulceration. Very rare cases of corneal perforation or ulceration have been reported during use of erlotinib (see section 4.8). Interactions with other medicinal products Potent inducers of CYP3A4 may reduce the efficacy of erlotinib whereas potent inhibitors of CYP3A4 may lead to increased toxicity. Concomitant treatment with these types of agents should be avoided (see section 4.5). Other forms of interactions Erlotinib is characterised by a decrease in solubility at pH above 5. Medicinal products that alter the pH of the upper Gastro-Intestinal (GI) tract, like proton pump inhibitors, H2 antagonists and antacids, may alter the solubility of erlotinib and hence its bioavailability. Increasing the dose of ERLOTINIB TARO when co- administered with such agents is not likely to compensate for the loss of exposure. Combination of erlotinib with proton pump inhibitors should be avoided. The effects of concomitant administration of erlotinib with H2 antagonists and antacids are unknown; however, reduced bioavailability is likely. Therefore, concomitant administration of these combinations should be avoided (see section 4.5). If the use of antacids is considered necessary during treatment with ERLOTINIB TARO, they should be taken at least 4 hours before or 2 hours after the daily dose of ERLOTINIB TARO. Excipients with known effect: The tablets contain lactose. Patients with rare hereditary problems of galactose intolerance, total lactase deficiency or glucose-galactose malabsorption should not take this medicine This medicine contains less than 1 mmol sodium (less than 23 mg) per tablet, that is to say ERLOTINIB TARO isessentially ‘sodium -free’.
Effects on Driving
4.7 Effects on ability to drive and use machines No studies on the effects on the ability to drive and use machines have been performed; however erlotinib is not associated with impairment of mental ability.

פרטי מסגרת הכללה בסל
1. התרופה תינתן לטיפול בסרטן ריאה מתקדם מקומי או גרורתי מסוג non small cell: א. כקו טיפול ראשון לחולים המבטאים מוטציה ב-EGFR; ב. לאחר כשל בטיפול קודם בתרופה אחרת המיועדת להתוויה זו, לקו טיפול שני או שלישי. 2. קיבל החולה טיפול באחת מהתרופות Erlotinib או Gefitinib או Afatinib, לא יקבל טיפול בתרופה האחרת, להתוויה זו. 3. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| סרטן ריאה מסוג EGFR positive NSCLC - קו ראשון | 10/01/2012 | אונקולוגיה | EGFR+ NSCLC | |
| טיפול בסרטן ריאה מסוג NSCLC - קו טיפול שני ושלישי | 01/01/2009 | אונקולוגיה | NSCLC |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/2009
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
