Quest for the right Drug
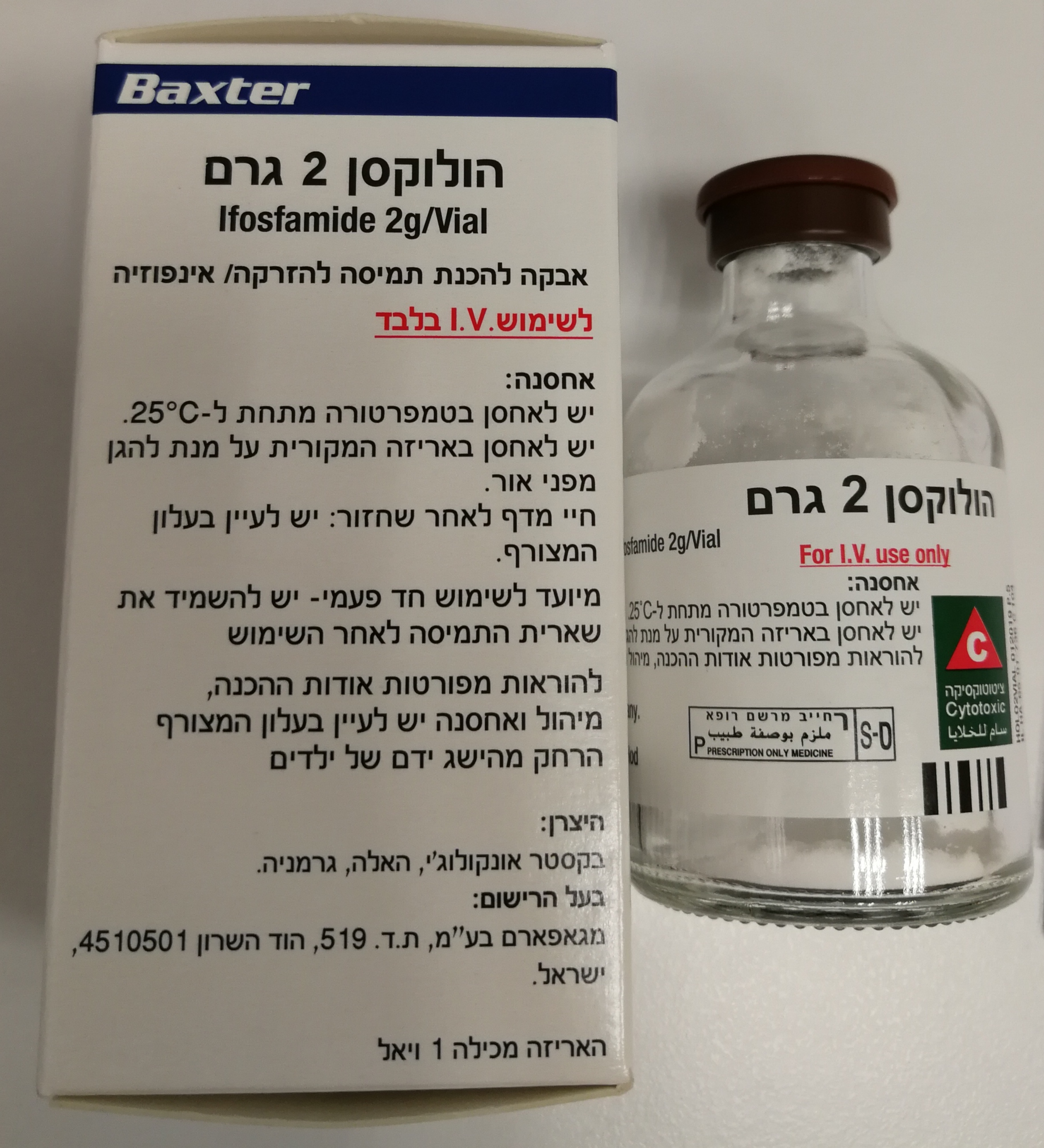
הולוקסן 2 גרם HOLOXAN 2 G (IFOSFAMIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה להמסה להזרקהאינפוזיה : POWDER FOR SOLUTION FOR INJ/INF
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Posology : מינונים
4.2 Posology and method of administration Recurrence of CNS toxicity after several uneventful treatment courses has been reported. Planned co administration or sequential administration of other substances or treatments that Ifosfamide should only be administered when there are facilities for regular monitoring of clinical, CNS toxicity appears to be dose dependent. could increase the likelihood or severity of toxic effects (by means of pharmacodynamic or biochemical and haematological parameters before, during and after administration and under pharmacokinetic interactions) requires careful individual assessment of the expected benefit the direction of a specialist oncology service by physicians experienced with this drug. Other risk factors that have been demonstrated or discussed in the literature include: and the risks. Patients receiving such combinations must be monitored closely for signs of – Renal dysfunction, elevated serum creatinine toxicity to permit timely intervention. Dosage must be individualized. Doses and duration of treatment and/or treatment intervals – Low serum albumin Patients being treated with ifosfamide and agents that reduce its activation should be monitored depend on the therapeutic indication, the scheme of a combination therapy, the patient’s general – Hepatic dysfunction for a potential reduction of therapeutic effectiveness and the need for dose adjustment. state of health and organ function, and the results of laboratory monitoring. – Low bilirubin, low haemoglobin levels, decreased white blood cell count In combination with other agents of similar toxicity, a dose reduction or extension of the therapy- – Acidosis, low serum bicarbonate Increased haematotoxicity and/or immunosuppression may result from a combined effect of free intervals may be necessary. – Electrolyte imbalances, hyponatraemia and inappropriate ADH (vasopressin) secretion, low ifosfamide and, for example: fluid intake – ACE inhibitors: ACE inhibitors can cause leukopenia. Method of administration – Presence of brain metastases, prior CNS disease, brain irradiation – Carboplatin – Cerebral sclerosis, peripheral vasculopathy – Cisplatin A guide to the dosage regimens used for most indications is given below: – Presence of tumour in lower abdomen, bulky abdominal disease – Natalizumab – Poor performance status, advanced age a) 8 - 12 g/m² equally fractionated as single daily doses over 3 – 5 days every 2-4 weeks. – Obesity, female gender Increased cardiotoxicity may result from a combined effect of ifosfamide and, for example: b) 5 - 6 g/m² (maximum 10 g) given as a 24 hour infusion every 3 – 4 weeks. – Interactions with other medicines (e.g., aprepitant, CYP 3A4 inhibitors), alcohol, drug – Anthracyclines abuse, or pretreatment with cisplatin – Irradiation of the cardiac region The frequency of dosage is determined by the degree of myelosuppression and the time taken to recover adequate bone marrow function. The usual number of courses given is 4, but up If encephalopathy develops, administration of ifosfamide should be discontinued. Increased pulmonary toxicity may result from a combined effect of ifosfamide and, for example: to 7 (6 by 24 hour infusion) courses have been given. Re-treatment has been given following – Amiodarone relapse. Publications report both successful and unsuccessful use of methylene blue for the treatment – G-CSF, GM-CSF (granulocyte colonystimulating factor, granulocyte macrophage colony- and prophylaxis of ifosfamide-associated encephalopathy. stimulating factor) During or immediately after administration, adequate amounts of fluid should be ingested or infused to force diuresis in order to reduce the risk of urothelial toxicity (see section 4.4). Due to the potential for additive effects, drugs acting on the CNS (such as antiemetics, Increased nephrotoxicity may result from a combined effect of ifosfamide and, for example: sedatives, narcotics, or antihistamines) must be used with particular caution or, if necessary, be – Cyclovir For prophylaxis of hemorrhagic cystitis, ifosfamide should be used in combination with mesna. discontinued in case of ifosfamide induced encephalopathy. – Aminoglycosides – Amphotericin B Use in Patients with Renal Impairment Renal and Urothelial Toxicity – Carboplatin In patients with renal impairment, particularly in those with severe renal impairment, decreased – Cisplatin renal excretion may result in increased plasma levels of ifosfamide and its metabolites. This may Ifosfamide is both nephrotoxic and urotoxic. result in increased toxicity (e.g., neurotoxicity, nephrotoxicity, haematotoxicity) and should be An increased risk of developing hemorrhagic cystitis may result from a combined effect of considered when determining the dosage in such patients (see section 4.3). ifosfamide and, for example: Glomerular and tubular kidney function must be evaluated and checked before commencement – Busulfan of therapy, as well as during and after treatment. – Irradiation of the bladder Ifosfamide and its metabolites are dialyzable. Close clinical monitoring of serum and urine chemistries, including phosphorus, potassium, and Use in Patients with Hepatic Impairment other laboratory parameters appropriate for identifying nephrotoxicity and urothelial toxicity is Additive CNS effects may result from a combined effect of ifosfamide and, for example: Hepatic impairment, particularly if severe, may be associated with decreased activation of recommended (see section 4.3). – Antiemetics ifosfamide. This may alter the effectiveness of ifosfamide treatment. Low serum albumin and – Antihistamines hepatic impairment are also considered risk factors for the development of CNS toxicity. Hepatic Nephrotoxic Effects – Narcotics impairment may increase the formation of a metabolite that is believed to cause or contribute to – Sedatives CNS toxicity and also contribute to nephrotoxicity. This should be considered when selecting the Fatal outcome from nephrotoxicity has been documented. dose and interpreting response to the dose selected (see section 4.3). Inducers of human hepatic and extrahepatic microsomal enzymes (e.g.,cytochrome P450 enzymes): Disorders of renal function (glomerular and tubular) following ifosfamide administration are very The potential for increased formation of metabolites responsible for cytotoxicity and other Use in Paediatric Patients common (see section 4.8). In children, the dosage and administration should be determined by the tumour type, tumour toxicities (depending on the enzymes induced) must be considered in case of prior or stage, the general condition of the patient, any previous cytotoxic therapy, and whether Development of a syndrome resembling SIADH (syndrome of inappropriate antidiuretic hormone concomitant treatment with, for example: chemotherapy or radiotherapy is to be administered concurrently. Clinical trials have involved secretion) has been reported with ifosfamide. – Carbamazepine doses of: – Corticosteroids a) 5 g/m² over 24 hours Tubular damage may become apparent during therapy, months or even years after cessation of – Rifampin b) 9 g/m² equally fractionated as single daily doses over 5 days treatment. – Phenobarbital c) 9 g/m² as a continuous infusion over 72 hours- repeated at three weekly intervals. – Phenytoin Glomerular or tubular dysfunction may resolve with time, remain stable, or progress over a – St. John’s Wort Elderly period of months or years, even after completion of ifosfamide treatment. See also aprepitant below. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other The risk of developing clinical manifestations of nephrotoxicity is increased with, for example: Inhibitors of CYP 3A4: Reduced activation and metabolism of ifosfamide may alter the drug therapy (see Section 5.2). – large cumulative doses of ifosfamide effectiveness of ifosfamide treatment. Inhibition of CYP 3A4 can also lead to increased formation – pre-existing renal impairment of an ifosfamide metabolite associated with CNS and nephrotoxicity. CYP 3A4 inhibitors include: Administration – prior or concurrent treatment with potentially nephrotoxic agents – Ketoconazole Ifosfamide is inert until activated by enzymes in the liver. However, safe handling is required – younger age in children – Fluconazole and advice is included under Pharmaceutical Precautions. The dry contents of a vial should be – reduced nephron reserve as in patients with renal tumours and those having undergone – Itraconazole dissolved in Water for Injections as follows: renal radiation or unilateral nephrectomy. – Sorafenib Holoxan 1 gram vial: add 25 ml of Water for Injections See also aprepitant below. Holoxan 2 gram vial: add 50 ml of Water for Injections Urothelial Effects Ifosfamide administration is associated with urotoxic effects, which can be reduced by Aprepitant: Reports suggest increased ifosfamide neurotoxicity in patients receiving antiemetic The resultant solution contains 4% of ifosfamide. prophylaxis with aprepitant, which is both an inducer and a moderate inhibitor of CYP 3A4. prophylactic use of mesna. The solution may then be: Docetaxel: Increased gastrointestinal toxicity has been reported when ifosfamide was Hemorrhagic cystitis requiring blood transfusion has been reported with ifosfamide. administered before docetaxel infusion. - For intravenous infusion (30-120min) – diluted in 250ml of Ringer’s solution or 5% strength The risk of hemorrhagic cystitis is dose-dependent and increased with administration of single glucose solution or 0.9% strength physiological solution high doses compared to fractionated administration. Coumarin derivatives: Increased INR (increased international normalized ratio) has been - For prolonged administration (60-120min) - diluted in 500ml of Ringer’s solution or 5% strength reported in patients receiving ifosfamide and warfarin. glucose solution or 0.9% strength physiological solution Hemorrhagic cystitis after a single dose of ifosfamide has been reported. - For continuous 24-hour infusion - diluted in 3000ml of 5% strength glucose solution or 0.9% Vaccines: The immunosuppressive effects of ifosfamide can be expected to reduce the response Before starting treatment, it is necessary to exclude or correct any urinary tract obstructions. to vaccination. Use of live vaccines may lead to vaccine induced infection. strength physiological solution During or immediately after administration, adequate amounts of fluid should be ingested or infused to force diuresis in order to reduce the risk of urinary tract toxicity. Tamoxifen: Concomitant use of tamoxifen and chemotherapy may increase the risk of Care should be taken that extravasation does not take place, however, should it occur local thromboembolic complications. tissue damage is unlikely and no specific measures need be taken. Repeated intravenous injections of large doses of Ifosfamide have resulted in local irritation. Ifosfamide should be used with caution, if at all, in patients with active urinary tract infections. Cisplatin: Cisplatin-induced hearing loss can be exacerbated by concurrent ifosfamide therapy Past or concomitant radiation of the bladder or busulfan treatment may increase the risk for (see also interactions above). Mesna should be used to prevent urothelial toxicity. hemorrhagic cystitis. Irinotecan: Formation of the active metabolite of irinotecan may be reduced when irinotecan is Where Ifosfamide is used as an i.v. bolus, increased dosages of mesna are recommended in administered with ifosfamide. children, patients whose urothelium may be damaged from previous therapies and those who Cardiotoxicity, Use in Patients with Cardiac Disease are not adequately protected by the standard dose of mesna. Fatal outcome of ifosfamide-associated cardiotoxicity has been reported. Alcohol: In some patients, alcohol may increase ifosfamide-induced nausea and vomiting. The patient should be well hydrated and maintained in fluid balance, replacement fluids being The risk of developing cardiotoxic effects is dose-dependent. It is increased in patients with prior Concurrent administration of antidiabetic agents, such as sulfonylureas and ifosfamide may given as necessary to achieve this. The fluid intake of patients on the intermittent regimen or concomitant treatment with other cardiotoxic agents or radiation of the cardiac region and, enhance the hypoglycaemic effects of the former drugs. should be at least 2 litres in 24 hours. As Ifosfamide may exert an antidiuretic effect, a diuretic possibly, renal impairment. may be necessary to ensure an adequate urinary output. Theoretical interactions of ifosfamide and allopurinol resulting in an increased severity of bone Particular caution should be exercised when ifosfamide is used in patients with risk factors for marrow depression. Urine should be sent for laboratory analysis before, and at the end of, each course of treatment, cardiotoxicity and in patients with pre-existing cardiac disease. and the patient should be monitored for output and evidence of proteinuria and haematuria at 4.6 Fertility, pregnancy and lactation regular intervals (4-hourly if possible) throughout the treatment period. The patient should be Manifestations of cardiotoxicity reported with ifosfamide treatment (see section 4.8) and include: instructed to report any signs or symptoms of cystitis. Ifosfamide should be avoided in patients – Supraventricular or ventricular arrhythmias, including atrial/supraventricular tachycardia, Pregnancy with cystitis from any cause until it has been treated. atrial fibrillation, pulseless ventricular tachycardia The administration of ifosfamide during organogenesis has been shown to have a fetotoxic – Decreased QRS voltage and ST segment or T-wave changes effect in mice, rats, and rabbits and therefore may cause fetal damage when administered to Antiemetics given before, during and after therapy may reduce nausea and vomiting. Oral – Toxic cardiomyopathy leading to heart failure with congestion and hypotension pregnant women. hygiene is important. – Pericardial effusion, fibrinous pericarditis, and epicardial fibrosis There are only very limited data available on the use of ifosfamide during pregnancy in humans. If leucocyte count is below 4,000/mm³ or the platelet count is below 100,000/mm³, treatment Pulmonary Toxicity Fetal growth retardation and neonatal anaemia have been reported following exposure to with Ifosfamide should be withheld until the blood count returns to normal. ifosfamide-containing chemotherapy regimens during pregnancy. Multiple congenital deviations There should be no signs or symptoms of urothelial toxicity or renal or hepatic impairment prior Pulmonary toxicity leading to respiratory failure as well as fatal outcome has been reported. have been reported after use during the first trimester of pregnancy. Animal data generated with to the start of each course of Ifosfamide. Interstitial pneumonitis and pulmonary fibrosis have been reported with ifosfamide treatment. cyclophosphamide, another oxazaphosphorine cytotoxic agent suggest that an increased risk of failed pregnancy and malformations may persist after discontinuation of the agent as long as

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
