Quest for the right Drug
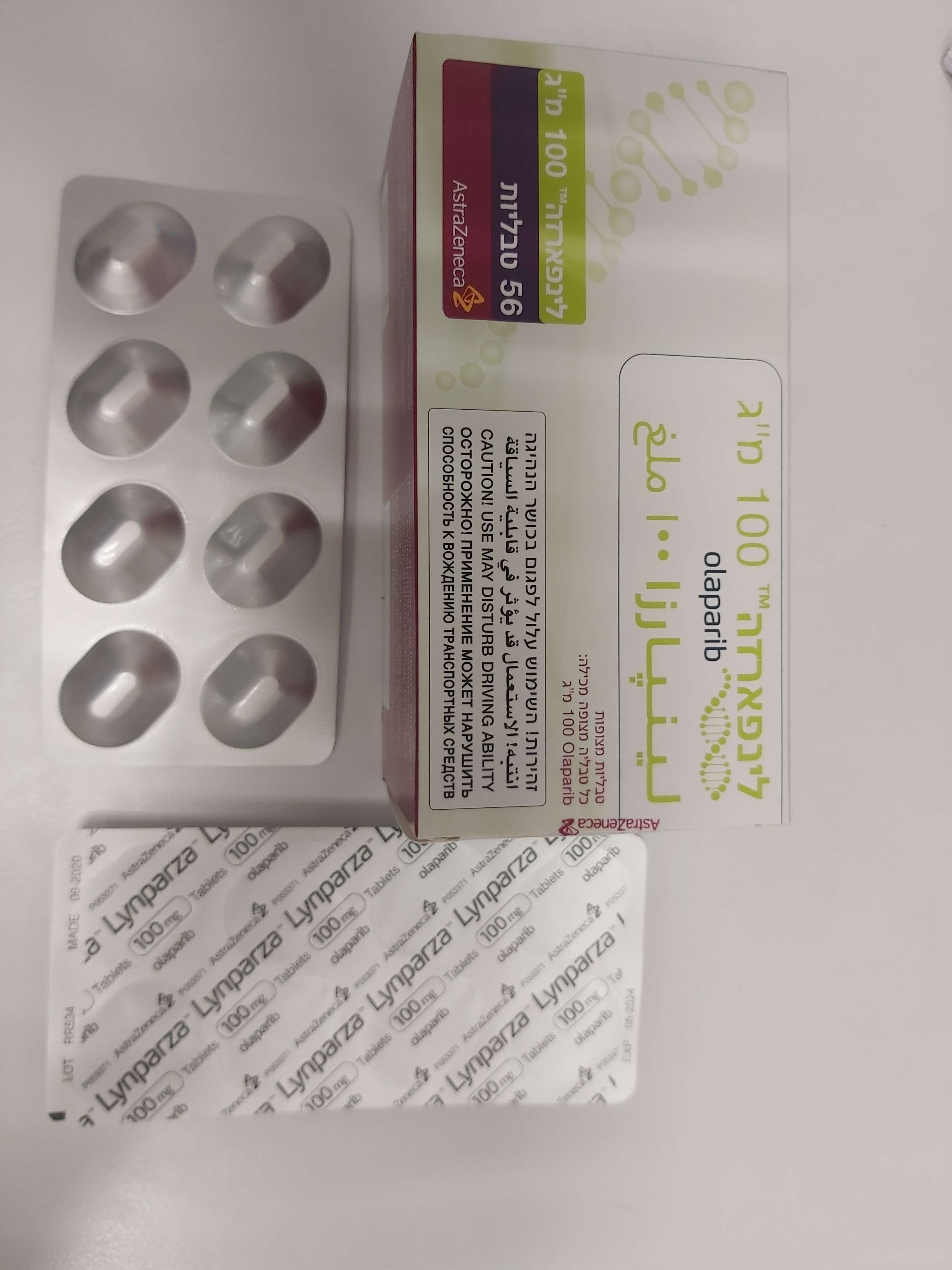
לינפארזה 100 מ"ג LYNPARZA 100 MG (OLAPARIB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Other antineoplastic agents, ATC code: L01XK01 Mechanism of action and pharmacodynamic effects Olaparib is a potent inhibitor of human poly (ADP-ribose) polymerase enzymes (PARP-1, PARP-2, and PARP-3), and has been shown to inhibit the growth of selected tumour cell lines in vitro and tumour growth in vivo either as a standalone treatment or in combination with established chemotherapies or new hormonal agents (NHA). PARPs are required for the efficient repair of DNA single strand breaks and an important aspect of PARP-induced repair requires that after chromatin modification, PARP auto-modifies itself and dissociates from the DNA to facilitate access for base excision repair (BER) enzymes. When olaparib is bound to the active site of DNA-associated PARP it prevents the dissociation of PARP and traps it on the DNA, thus blocking repair. In replicating cells this also leads to the formation of DNA double-strand breaks (DSBs) when replication forks meet the PARP-DNA adducts. In normal cells, homologous recombination repair (HRR) pathway is effective at repairing these DNA DSBs. In cancer cells lacking critical functional components for efficient HRR such as BRCA1 or 2, DNA DSBs cannot be repaired accurately or effectively, leading to substantial homologous recombination deficiency (HRD). Instead, alternative and error-prone pathways are activated, such as the classical non-homologous end joining (NHEJ) pathway, leading to a high degree of genomic instability. After a number of rounds of replication, genomic instability can reach insupportable levels and result in cancer cell death, as cancer cells already have a high DNA damage load relative to normal cells. HRR pathway may be compromised by other mechanisms, although the causative aberrancy and penetrance are not fully elucidated. Absence of fully functional HRR pathway is one of the key determinants of platinum sensitivity in ovarian and possibly other cancers. In BRCA1/2-deficient in vivo models, olaparib given after platinum treatment resulted in a delay in tumour progression and an increase in overall survival compared to platinum treatment alone that correlated with the period of olaparib maintenance treatment. Combined anti-tumour effect with NHAs Pre-clinical studies in prostate cancer models reported a combined anti-tumour effect when PARP inhibitors and next-generation hormonal agents are administered together. PARP is involved in positive co-regulation of androgen receptor (AR) signalling, which leads to enhanced AR target gene suppression when PARP/AR signalling is co-inhibited. Other pre- clinical studies reported that treatment with NHAs inhibit the transcription of some HRR genes, therefore, inducing HRR deficiency and increased sensitivity to PARP inhibitors via non-genetic mechanisms. Detection of BRCA1/2 mutations Genetic testing should be conducted by an experienced laboratory using a validated test. Local or central testing of blood and/or tumour samples for germline and/or somatic BRCA1/2 mutations have been used in different studies. DNA obtained from a tissue or blood sample has been tested in most of the studies, with testing of ctDNA being used for exploratory purposes. Depending on the test used and the international classification consensus, the BRCA1/2 mutations have been classified as deleterious/suspected deleterious or pathogenic/likely pathogenic. Homologous recombination deficiency (HRD) positive status can be defined by detection of a BRCA1/2 mutation classified as deleterious/suspected deleterious or pathogenic/likely pathogenic. Detection of these mutations could be combined with positive HRD score (below) to determine HRD positive status. Detection of genomic instability HR deficiency-associated genomic alterations that have been investigated in Paola-1 include genome- wide loss of heterozygosity, telomeric allelic imbalance and large scale transition, which are continuous measures with pre-defined criteria and score. Composite genomic instability score (GIS, also called HRD score) is determined when the combined measures and respective scores are used to assess the extent of specific genomic aberrations accumulated in tumour cells. Lower score defines lower likelihood of HR deficiency of tumour cells and higher score determines higher likelihood of HR deficiency of tumour cells at the time of the sample collection relative to exposure to DNA damaging agents. Validated cut-offs should be used to determine GIS positive status. HRD positive status can be defined by a composite GIS score for HR deficiency- associated genomic alterations tested by an experienced laboratory using a validated test. Clinical efficacy and safety First-line maintenance treatment of BRCA-mutated advanced ovarian cancer: SOLO1 Study The safety and efficacy of olaparib as maintenance therapy were studied in patients with newly diagnosed advanced (FIGO Stage III-IV) high-grade serous or endometrioid BRCA1/2 mutated (BRCA1/2m) ovarian cancer following completion of first-line platinum-based chemotherapy in a Phase III randomised, double-blind, placebo-controlled, multicentre trial. In this study 391 patients were randomised 2:1 to receive either Lynparza (300 mg [2 x 150 mg tablets] twice daily) or placebo. Patients were stratified by response to first-line platinum chemotherapy; complete response (CR) or partial response (PR). Treatment was continued until radiological progression of the underlying disease, unacceptable toxicity or for up to 2 years. For patients who remained in complete clinical response (i.e. no radiological evidence of disease), the maximum duration of treatment was 2 years; however, patients who had evidence of disease that remained stable (i.e. no evidence of disease progression) could continue to receive Lynparza beyond 2 years. Patients with germline or somatic BRCA1/2 mutations were identified prospectively either from germline testing in blood via a local test (n=208) or central test (n=181) or from testing a tumour sample using a local test (n=2). By central germline testing, deleterious or suspected deleterious mutations were identified in 95.3% (365/383) and 4.7% (18/383) of patients, respectively. Large rearrangements in the BRCA1/2 genes were detected in 5.5% (21/383) of the randomised patients. The gBRCAm status of patients enrolled via local testing was confirmed retrospectively by central testing. Retrospective testing of patients with available tumour samples was performed using central testing and generated successful results in 341 patients, of which 95% had an eligible mutation (known [n=47] or likely pathogenic [n=277]) and 2 gBRCAwt patients were confirmed to have sBRCAm only. There were 389 patients who were germline BRCA1/2m and 2 who were somatic BRCA1/2m in SOLO1. Demographic and baseline characteristics were generally well balanced between the olaparib and placebo treatment arms. Median age was 53 years in both arms. Ovarian cancer was the primary tumour in 85% of the patients. The most common histological type was serous (96%), endometrioid histology was reported in 2% of the patients. Most patients were ECOG performance status 0 (78%), there are no data in patients with performance status 2 to 4. Sixty- three percent (63%) of the patients had upfront debulking surgery and of these the majority (75%) had no macroscopic residual disease. Interval debulking surgery was performed in 35% of the patients and of these 82% had no macroscopic residual disease reported. Seven patients, all stage IV, had no cytoreductive surgery. All patients had received first-line platinum- based therapy. There was no evidence of disease at study entry (CR), defined by the investigator as no radiological evidence of disease and cancer antigen 125 (CA-125) within normal range, in 73% and 77% of patients in the olaparib and placebo arms, respectively. PR, defined as the presence of any measurable or non-measurable lesions at baseline or elevated CA-125, was reported in 27% and 23% of patients in the olaparib and placebo arms, respectively. Ninety three percent (93%) of patients were randomised within 8 weeks of their last dose of platinum-based chemotherapy. Patients who had been treated with bevacizumab were excluded from the study, therefore there are no safety and efficacy data on olaparib patients who had previously received bevacizumab. There are very limited data in patients with a somatic BRCA mutation. The primary endpoint was progression-free survival (PFS) defined as time from randomisation to progression determined by investigator assessment using modified Response Evaluation Criteria in Solid Tumors (RECIST) 1.1, or death. Secondary efficacy endpoints included time from randomisation to second progression or death (PFS2), overall survival (OS), time from randomisation to discontinuation of treatment or death (TDT), time from randomisation to first subsequent anti- cancer therapy or death (TFST) and health related quality of life (HRQoL). Patients had tumour assessments at baseline and every 12 weeks for 3 years, and then every 24 weeks relative to date of randomisation, until objective radiological disease progression. The study demonstrated a clinically relevant and statistically significant improvement in investigator assessed PFS for olaparib compared to placebo. The investigator assessment of PFS was supported with a blinded independent central radiological (BICR) review of PFS. A descriptive analysis performed at seven years after the last patient was randomized demonstrated a clinically meaningful benefit in OS that numerically favoured the olaparib arm. Efficacy results are presented in Table 2 and Figures 1 and 2. Table 2 Efficacy results for newly diagnosed patients with BRCA1/2m advanced ovarian cancer in SOLO1 Olaparib 300 mg bd Placeboc PFS (51% maturity)a Number of events: Total number of patients (%) 102:260 (39) 96:131 (73) Median time (months) NR 13.8 HR (95% CI)b 0.30 (0.23-0.41) P value (2-sided) p<0.0001 PFS2 (31% maturity) Number of events: Total number of patients (%) 69:260 (27) 52:131 (40) Median time (months) NR 41.9 HR (95% CI) c 0.50 (0.35-0.72) P value (2-sided) p=0.0002 OS (38% maturity)d Number of events: Total number of patients (%) 84:260 (32) 65:131 (50) Median time (months) NR 75.2 HR (95% CI)b 0.55 (0.40-0.76) TFST (60% maturity) Number of events: Total number of patients (%) 135:260 (52) 98:131 (75) Median time (months) 64.0 15.1 HR (95% CI) c 0.37 (0.28-0.48) a Based on Kaplan-Meier estimates, the proportion of patients that were progression free at 24 and 36 months were 74% and 60% for olaparib versus 35% and 27% for placebo; the median follow-up time was 41 months for both the olaparib and placebo arms. b A value <1 favours olaparib. The analysis was performed using a Cox proportional hazards model including response to previous platinum chemotherapy (CR or PR) as a covariate. c Of the 97 patients on the placebo arm who received subsequent therapy, 58 (60%) received a PARP inhibitor. d Based on Kaplan-Meier estimates, the proportion of patients that were alive 84 months was 67% for olaparib versus 47% for placebo. bd Twice daily; NR Not reached; CI Confidence interval; PFS Progression-free survival; PFS2 Time to second progression or death; OS Overall survival; TFST Time from randomisation to first subsequent anti-cancer therapy or death. Figure 1 SOLO1: Kaplan-Meier plot of PFS in newly diagnosed patients with BRCA1/2m advanced ovarian cancer (51% maturity - investigator assessment) Figure 2 SOLO1: Kaplan-Meier plot of OS in newly diagnosed patients with BRCA1/2m advanced ovarian cancer (38% maturity) Consistent results were observed in the subgroups of patients by evidence of the disease at study entry. Patients with CR defined by the investigator had HR 0.34 (95% CI 0.24–0.47); median PFS not reached on olaparib vs 15.3 months on placebo. At 24 and 36 months, Olaparib 300mg twice daily tablet Placebo twice daily tablet Proportion of patients event free Time from randomisation (months) Number of patients at risk: Olaparib 300mg twice daily tablet Placebo twice daily tablet respectively, 68% and 45% patients remained in CR in the olaparib arm, and 34% and 22% of patients in the placebo arm. Patients with PR at study entry had PFS HR 0.31 (95% CI 0.18, 0.52; median PFS 30.9 months on olaparib vs 8.4 months on placebo). Patients with PR at study entry either achieved CR (15% in olaparib arm and 4% in the placebo arm at 24 months, remained in CR at 36 months) or had further PR/stable disease (43% in olaparib arm and 15% in the placebo arm at 24 months; 17% in olaparib arm and 15% in placebo arm at 36 months). The proportion of patients who progressed within 6 months of the last dose of platinum-based chemotherapy was 3.5% for olaparib and 8.4% for placebo. Maintenance treatment of platinum-sensitive relapsed (PSR) ovarian cancer SOLO2 Study The safety and efficacy of olaparib as maintenance therapy were studied in a Phase III randomised, double-blind, placebo-controlled trial in patients with germline BRCA1/2- mutated PSR ovarian, fallopian tube or primary peritoneal cancer. The study compared the efficacy of Lynparza maintenance treatment (300 mg [2 x 150 mg tablets] twice daily) taken until progression with placebo treatment in 295 patients with high-grade serous or endometrioid PSR ovarian cancer (2:1 randomisation: 196 olaparib and 99 placebo) who were in response (CR or PR) following completion of platinum-containing chemotherapy. Patients who have received two or more platinum-containing regimens and whose disease had recurred > 6 months after completion of penultimate platinum-based chemotherapy were enrolled. Patients could not have received prior olaparib or other PARP inhibitor treatment. Patients could have received prior bevacizumab, except in the regimen immediately prior to randomisation. All patients had evidence of gBRCA1/2m at baseline. Patients with BRCA1/2 mutations were identified either from germline testing in blood via a local test or by central testing at Myriad or from testing a tumour sample using a local test. Large rearrangements in the BRCA1/2 genes were detected in 4.7% (14/295) of the randomised patients. Demographic and baseline characteristics were generally well balanced between the olaparib and placebo arms. Median age was 56 years in both arms. Ovarian cancer was the primary tumour in > 80% of the patients. The most common histological type was serous (> 90%), endometrioid histology was reported in 6% of the patients. In the olaparib arm 55% of the patients had only 2 prior lines of treatment with 45% receiving 3 or more prior lines of treatment. In the placebo arm 61% of patients had received only 2 prior lines with 39% receiving 3 or more prior lines of treatment. Most patients were ECOG performance status 0 (81%), there are no data in patients with performance status 2 to 4. Platinum free interval was > 12 months in 60% and > 6-12 months in 40% of the patients. Response to prior platinum chemotherapy was complete in 47% and partial in 53% of the patients. In the olaparib and placebo arms, 17% and 20% of patients had prior bevacizumab, respectively. The primary endpoint was PFS determined by investigator assessment using RECIST 1.1. Secondary efficacy endpoints included PFS2; OS TDT, TFST, TSST; and HRQoL. The study met its primary objective demonstrating a statistically significant improvement in investigator assessed PFS for olaparib compared with placebo with a HR of 0.30 (95% CI 0.22-0.41; p<0.0001; median 19.1 months olaparib vs 5.5 months placebo). The investigator assessment of PFS was supported with a blinded independent central radiological review of PFS (HR 0.25; 95% CI 0.18-0.35; p<0.0001; median 30.2 months for olaparib and 5.5 months placebo). At 2 years, 43% olaparib-treated patients remained progression free compared with only 15% placebo-treated patients. A summary of the primary objective outcome for patients with gBRCA1/2m PSR ovarian cancer in SOLO2 is presented in Table 3 and Figure 3. Table 3 Summary of primary objective outcome for patients with gBRCA1/2m PSR ovarian cancer in SOLO2 a HR= Hazard Ratio. A value <1 favours olaparib. The analysis was performed using a Cox proportional hazard model including response to previous platinum chemotherapy (CR or PR), and time to disease progression (>6-12 months and >12 months) in the penultimate platinum-based chemotherapy as covariates. bd Twice daily; PFS progression-free survival; CI confidence interval; Figure 3 SOLO2: Kaplan-Meier plot of PFS in patients with gBRCA1/2m PSR ovarian cancer (63% maturity - investigator assessment) Proportion of patients event free Time from randomisation (months) - - - - - - - - - Placebo bd --------------Olaparib 300 mg bd Number of patients at risk: 196 182 156 134 118 104 89 82 32 29 3 2 0 Olaparib 300 mg bd 99 70 37 22 18 17 14 12 7 6 0 0 0 Placebo bd bd Twice daily; PFS Progression free survival At the final analysis of OS (61% maturity) the HR was 0.74 (95% CI 0.54-1.00; p=0.0537; median 51.7 months for olaparib vs 38.8 months for placebo) which did not reach statistical significance. The secondary endpoints TFST and PFS2 demonstrated a persistent and statistically significant improvement for olaparib compared with placebo. Results for OS, TFST and PFS2 are presented in Table 4 and Figure 4. Table 4 Summary of key secondary objective outcomes for patients with gBRCA1/2m PSR ovarian cancer in SOLO2 Olaparib 300 mg tablet Placebo bd OS (61% maturity) Number of events: Total number of 116:196 (59) 65:99 (66) patients (%) Median time (95% CI), months 51.7 (41.5, 59.1) 38.8 (31.4, 48.6) HR (95% CI) a 0.74 (0.54-1.00) P value (2-sided) p=0.0537 TFST (71% maturity) Number of events: Total number of 139:196 (71) 86:99 (87) patients (%) Median time (months) (95% CI) 27.4 (22.6-31.1) 7.2 (6.3-8.5) HR (95% CI) a 0.37 (0.28-0.48) P value* (2-sided) P<0.0001 PFS2 (40% maturity) Number of events: Total number of 70:196 (36) 49:99 (50) patients (%) Median time (months) (95% CI) NR (24.1-NR) 18.4 (15.4-22.8) HR (95% CI) a 0.50 (0.34-0.72) P value (2-sided) p=0.0002 Not controlled for multiplicity a HR= Hazard Ratio. A value <1 favours olaparib. The analysis was performed using a Cox proportional hazard model including response to previous platinum chemotherapy (CR or PR), and time to disease progression (>6-12 months and >12 months) in the penultimate platinum-based chemotherapy as covariates. bd Twice daily; NR not reached; CI confidence interval; PFS2 time from randomisation to second progression or death; TFST Time from randomisation to start of first subsequent therapy or death. Figure 4 SOLO2: Kaplan-Meier plot of OS in patients with gBRCA1/2m PSR ovarian cancer 61% maturity) Proportion of patients event free Time from randomisation (months) Number of patients at risk: Olaparib 300mg twice daily tablet Placebo twice daily tablet Among the patients entering the trial with measurable disease (target lesions at baseline), an objective response rate of 41% was achieved in the Lynparza arm versus 17% on placebo. Of patients treated with Lynparza, who entered the study with evidence of disease (target or non-target lesions at baseline), 15.0% experienced complete response compared with 9.1% of patients on placebo. At the time of the analysis of PFS the median duration of treatment was 19.4 months for olaparib and 5.6 months for placebo. The majority of patients remained on the 300 mg bd starting dose of olaparib. The incidence of dose interruptions, reductions, discontinuations due to an adverse event was 45.1%, 25.1% and 10.8%, respectively. Dose interruptions occurred most frequently in the first 3 months and dose reductions in the first 3-6 months of treatment. The most frequent adverse reactions leading to dose interruption or dose reduction were anaemia, nausea and vomiting Patient-reported outcome (PRO) data indicate no difference for the olaparib-treated patients as compared to placebo as assessed by the change from baseline in the TOI of the FACT- O. Study 19 (D0810C00019) The safety and efficacy of olaparib as a maintenance therapy in the treatment of PSR ovarian, including fallopian tube or primary peritoneal cancer patients, following treatment with two or more platinum containing regimens, were studied in a large Phase II randomised, double-blind, placebo-controlled trial (study 19). The study compared the efficacy of Lynparza maintenance treatment taken until progression with placebo treatment in 265 (136 olaparib and 129 placebo) PSR high grade serous ovarian cancer patients who were in response (CR or PR) following completion of platinum-containing chemotherapy. The primary endpoint was PFS based on investigator assessment using RECIST 1.0. Secondary efficacy endpoints included OS, disease control rate (DCR) defined as confirmed CR/PR + SD (stable disease), HRQoL and disease related symptoms. Exploratory analyses of TFST and TSST were also performed. Patients whose disease had recurred >6 months after completion of penultimate platinum- based chemotherapy were enrolled. Enrolment did not require evidence of BRCA1/2 mutation (BRCA mutation status for some patients was determined retrospectively). Patients could not have received prior olaparib or other PARP inhibitor treatment. Patients could have received prior bevacizumab, except in the regimen immediately prior to randomisation. Retreatment with olaparib was not permitted following progression on olaparib. Patients with BRCA1/2 mutations were identified either from germline testing in blood via a local test or by central testing at Myriad or from testing a tumour sample using a test performed by Foundation Medicine. Large rearrangements in the BRCA1/2 genes were detected in 7.4% (10/136) of the randomised patients. Demographic and baseline characteristics were generally well balanced between the olaparib and placebo arms. Median age was 59 years in both arms. Ovarian cancer was the primary tumour in 86% of the patients. In the olaparib arm 44% of the patients had only 2 prior lines of treatment with 56% receiving 3 or more prior lines of treatment. In the placebo arm 49% of patients had received only 2 prior lines with 51% receiving 3 or more prior lines of treatment. Most patients were ECOG performance status 0 (77%), there are no data in patients with performance status 2 to 4. Platinum free interval was > 12 months in 60% and 6-12 months in 40% of the patients. Response to prior platinum chemotherapy was complete in 45% and partial in 55% of the patients. In the olaparib and placebo arms, 6% and 5% of patients had prior bevacizumab, respectively. The study met its primary objective demonstrating a statistically significant improvement in PFS for olaparib compared with placebo in the overall population with a HR of 0.35 (95% CI 0.25-0.49; p<0.00001; median 8.4 months olaparib vs 4.8 months placebo). At the final OS analysis (data cut off [DCO] 9 May 2016) at 79% maturity, the hazard ratio comparing olaparib with placebo was 0.73 (95% CI 0.55-0.95; p=0.02138 [did not meet pre-specified significance level of < 0.0095]; median 29.8 months olaparib versus 27.8 months placebo). In the olaparib-treated group, 23.5% (n=32/136) of patients remained on treatment for ≥2 years as compared with 3.9% (n=5/128) of the patients on placebo. Although patient numbers were limited, 13.2% (n=18/136) of the patients in the olaparib-treated group remained on treatment for ≥5 years as compared with 0.8% (n=1/128) in the placebo group. Preplanned subgroup analysis identified patients with BRCA1/2-mutated ovarian cancer (n=136, 51.3%; including 20 patients identified with a somatic tumour BRCA1/2 mutation) as the subgroup that derived the greatest clinical benefit from olaparib maintenance monotherapy. A benefit was also observed in patients with BRCA1/2 wild-type/variants of uncertain significance (BRCA1/2 wt/VUS), although of a lesser magnitude. There was no strategy for multiple testing in place for the sub-group analyses. A summary of the primary objective outcome for patients with BRCA1/2-mutated and BRCA1/2 wt/VUS PSR ovarian cancer in study 19 is presented in Table 5 and for all patients in Study 19 in Table 5 and Figure 5. Table 5 Summary of primary objective outcome for all patients and patients with BRCA1/2-mutated and BRCA1/2 wt/VUS PSR ovarian cancer in Study 19 a All patients comprises of the following subgroups: BRCA1/2-mutated, BRCA1/2 wt/VUS and BRCA1/2 status unknown (11 patients with status unknown, not shown as a separate subgroup in table). b HR= Hazard Ratio. A value <1 favours olaparib. The analysis was performed using a Cox proportional hazards model with factors for treatment, ethnic descent, platinum sensitivity and response to final platinum therapy. bd Twice daily; PFS progression-free survival; DCO data cut off; CI confidence interval; NR not reached. Figure 5 Study 19: Kaplan-Meier plot of PFS in the FAS (58% maturity – investigator assessment) DCO 30 June 2010 A summary of key secondary objective outcomes for patients with BRCA1/2-mutated and BRCA1/2 wt/VUS PSR ovarian cancer in Study 19 is presented in Table 6 and for all patients in Study 19 in Table 6 and Figure 6. Table 6 Summary of key secondary objective outcomes for all patients and patients with BRCA1/2-mutated and BRCA1/2 wt/VUS PSR ovarian cancer in study 19 * There was no strategy for multiple testing in place for the sub-group analyses or for the all patients TFST. a All patients comprises of the following subgroups: BRCA1/2-mutated, BRCA1/2 wt/VUS and BRCA1/2 status unknown (11 patients with status unknown, not shown as a separate subgroup in table). b HR= Hazard Ratio. A value <1 favours olaparib. The analysis was performed using a Cox proportional hazards model with factors for treatment, ethnic descent, platinum sensitivity and response to final platinum therapy. c Approximately a quarter of placebo-treated patients in the BRCA-mutated subgroup (14/62; 22.6%) received a subsequent PARP inhibitor. OS Overall survival; DCO data cut off; CI confidence interval; TFST time from randomisation to start of first subsequent therapy or death. Figure 6 Study 19: Kaplan Meier plot of OS in the FAS (79% maturity) DCO 09 May 2016 Placebo twice daily tablet bd Twice daily; DCO Data cut off; FAS Full analysis set; OS Overall survival At the time of the analysis of PFS the median duration of treatment was 8 months for olaparib and 4 months for placebo. The majority of patients remained on the starting dose of olaparib. The incidence of dose interruptions, reductions and discontinuations due to an adverse event was 34.6%, 25.7% and 5.9%, respectively. Dose interruptions and reductions occurred most frequently in the first 3 months of treatment. The most frequent adverse reactions leading to dose interruption or dose reduction were nausea, anaemia, vomiting, neutropenia and fatigue. The incidence of anaemia adverse reactions was 22.8% (CTCAE grade ≥3 7.4%). Patient-reported outcome (PRO) data indicate no difference for the olaparib-treated patients as compared to placebo as measured by improvement and worsening rates in the TOI and FACT-O total. OPINION Study OPINION, a Phase IIIb single arm, multicentre study, investigated olaparib as a maintenance treatment in patients with PSR ovarian, fallopian tube or primary peritoneal cancer following 2 or more lines of platinum based chemotherapy and who did not have a known deleterious or suspected deleterious gBRCA mutation. Patients whose disease was in response (CR or PR) following completion of platinum-based chemotherapy were enrolled. A total of 279 patients were enrolled and received olaparib treatment in this study until disease progression or unacceptable toxicity. Based on central testing 90.7% were confirmed with a non gBRCAm status, in addition 9.7% were identified as sBRCAm. The primary endpoint was investigator-assessed PFS according to modified RECIST v1.1. Secondary endpoints included OS. Olaparib, when used as maintenance therapy, demonstrated clinical activity in patients with non- gBRCAm PSR ovarian cancer. At the final overall survival analysis (DCO 17 September 2021), the OS data were 52.3% mature. A summary of the primary PFS and OS secondary objective outcome for patients with non- gBRCAm PSR ovarian cancer in OPINION is presented in Table 7. Table 7 Summary of key objective outcome for non-gBRCAm patients with PSR ovarian cancer in OPINION Olaparib tablets 300 mg bd PFS (75% maturity) (DCO 2 October 2020) Number of events: total number of patients 210: 279 (75.3) (%) Median PFS (95% CI), monthsa 9.2 (7.6, 10.9) OS (52.3% maturity) (DCO 17 September 2021) Number of events: total number of patients 146: 279 (52.3) (%) Median OS (95% CI), monthsa 32.7 (29.5, 35.3) a Calculated using the Kaplan-Meier technique. Confidence intervals for median PFS and OS were derived based on Brookmeyer Crowley method. bd Twice daily; PFS Progression-free survival; OS Overall survival; DCO Data cut off; CI Confidence interval. Adjuvant Treatment of BRCA-mutated HER2-negative High Risk Early Breast Cancer OlympiA The safety of Lynparza as monotherapy for the adjuvant treatment of patients with BRCA-mutated HER2 negative high risk early breast cancer was investigated in OlympiA. This study was a randomized, double-blind, multi-center study in which patients received either Lynparza tablets 300 mg orally twice daily (n=911) or placebo (n=904) for a total of 1 year, or until disease recurrence, or unacceptable toxicity. The median duration of treatment was 1 year in both arms. Dose interruptions due to an adverse reaction of any grade occurred in 31% of patients receiving Lynparza; dose reductions due to an adverse reaction occurred in 23% of patients receiving Lynparza. The most frequent adverse reactions leading to dose interruption of Lynparza were anemia (11%), neutropenia (6%), nausea (5%), leukopenia (3.5%), fatigue (3%), and vomiting (2.9%) and the most frequent adverse reactions leading to dose reduction of Lynparza were anemia (8%), nausea (4.7%), neutropenia (4.2%), fatigue (3.3%), leukopenia (1.8%), and vomiting (1.5%). Discontinuation due to adverse reactions occurred in 10% of patients receiving Lynparza. The adverse reactions that most frequently led to discontinuation of Lynparza were nausea (2%), anemia (1.8%), and fatigue (1.3%). Tables 7 and 8 summarize the adverse reactions and laboratory abnormalities, respectively, in patients in OlympiA. Table 7 Adverse Reactions* in OlympiA (≥ 10% of Patients Who Received Lynparza) Adverse Reactions Lynparza Placeb tablets o n=911 n=904 Grades 1- Grades 3- Grades 1- Grades 3- 4 (%) 4 (%) 4 (%) 4 (%) Gastrointestinal Disorders Nausea 57 0.8 23 0 Vomiting 23 0.7 8 0 Diarrhea 18 0.3 14 0.3 Stomatitis† 10 0.1 4.5 0 General Disorders and Administration Site Conditions Fatigue (including 42 1.8 28 0.7 asthenia) Blood and Lymphatic Disorders Anemia‡ 24 9 3.9 0.3 Leukopenia§ 17 3 6 0.3 Neutropenia ¶ 16 5 7 0.8 Nervous System Disorders Headache 20 0.2 17 0.1 Dysgeusia# 12 0 4.8 0 Dizziness 11 0.1 7 0.1 Metabolism and Nutrition Disorders Decreased appetite 13 0.2 6 0 * Graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE), version 4.03 † Includes aphthous ulcer, mouth ulceration, stomatitis. ‡ Includes anemia, anemia macrocytic, erythropenia, hematocrit decreased, hemoglobin decreased, normochromic anemia, normochromic normocytic anemia, normocytic anemia, red blood cell count decreased. § Includes leukopenia, white blood cell count decreased. ¶ Includes agranulocytosis, febrile neutropenia, granulocyte count decreased, granulocytopenia, idiopathic neutropenia, neutropenia, neutropenic infection, neutropenic sepsis, neutrophil count decreased. # Includes dysgeusia, taste disorder. In addition, adverse reactions in OlympiA that occurred in <10% of patients receiving Lynparza were cough (9.2%), lymphopenia (7%), dyspepsia (6%), upper abdominal pain (4.9%), rash (4.9%), dyspnea (4.2%), thrombocytopenia (4.2%), increase in creatinine (2%), hypersensitivity (0.9%), dermatitis (0.5%), increase in mean corpuscular volume (0.2%), and MDS/AML (0.1%). Table 8 Laboratory Abnormalities Reported in ≥25% of Patients in OlympiA Lynparza Placeb Laboratory tablets n†= o 911 n†=904 Parameter* Grades 1- Grades 3- Grades 1- Grades 3- 4 (%) 4 (%) 4 (%) 4 (%) Decrease in 77 13 59 3.7 lymphocytes Decrease in 65 8 31 0.9 hemoglobin Decrease in leukocytes 64 5 42 0.7 Increase in mean 67 0 4.8 0 corpuscular volume‡ Decrease in absolute 39 7 27 1.1 neutrophil count * Patients were allowed to enter clinical studies with laboratory values of CTCAE Grade 1. † This number represents the safety population. The derived values in the table are based on the total number of evaluable patients for each laboratory parameter. ‡ Represents the proportion of subjects whose mean corpuscular volume was > ULN. The efficacy of Lynparza was evaluated in OlympiA (NCT02032823), a randomized (1:1), double- blind, placebo-controlled, international study in patients with gBRCAm HER2-negative high risk early breast cancer who had completed definitive local treatment and neoadjuvant or adjuvant chemotherapy. Patients were randomized to receive Lynparza tablets 300 mg orally twice daily or placebo. Treatment was continued for up to 1 year, or until disease recurrence, or unacceptable toxicity. Patients were required to have completed at least 6 cycles of neoadjuvant or adjuvant chemotherapy containing anthracyclines, taxanes or both. Prior platinum for previous cancer (e.g. ovarian) or as adjuvant or neoadjuvant treatment for breast cancer was allowed. Patients with high risk early breast cancer were defined as follows: • patients who received prior neoadjuvant chemotherapy: patients with either triple negative breast cancer (TNBC) or hormone receptor positive breast cancer must have had residual invasive cancer in the breast and/or the resected lymph nodes (non-pathologic complete response) at the time of surgery. Additionally, patients with hormone receptor positive breast cancer must have had a score of ≥3 based on pre-treatment clinical and post- treatment pathologic stage (CPS), estrogen receptor (ER) status, and histologic grade as shown in Table 9. Table 9 Early Breast Cancer Stage, Receptor Status, and Grade Scoring Requirements for Study Enrollment* Stage/feature Points Clinical Stage I/IIA 0 (pre-treatment) IIB/IIIA 1 IIIB/IIIC 2 Pathologic Stage 0/I 0 (post-treatment) IIA/IIB/IIIA/IIIB 1 IIIC 2 Receptor status ER positive 0 ER negative 1 Nuclear grade Nuclear grade 1-2 0 Nuclear grade 3 1 * Total score of ≥3 required for patients with hormone receptor positive breast cancer. • patients who received prior adjuvant chemotherapy: patients with TNBC must have had node positive disease or node negative disease with a ≥2cm primary tumor; patients with hormone receptor positive, HER2-negative breast cancer must have had ≥4 pathologically confirmed positive lymph nodes. 40 Randomization was stratified by hormone receptor status (hormone receptor positive versus triple negative), by prior neoadjuvant versus adjuvant chemotherapy, and by prior platinum use for breast cancer (yes versus no). The major efficacy outcome measure was invasive disease free survival (IDFS), defined as the time from randomization to date of first recurrence, where recurrence is defined as invasive loco- regional, distant recurrence, contralateral invasive breast cancer, new cancer or death from any cause. An additional efficacy outcome measure was OS. A total of 1836 patients were randomized, 921 to Lynparza and 915 to placebo. Demographic and baseline characteristics were well balanced between arms. The median age was 42 years. Sixty- seven percent (67%) of patients were White, 29% were Asian, and 3% were Black. Three percent (3%) of patients were Hispanic or Latino. Two patients (0.2%) in the Lynparza arm and four patients (0.4%) in the placebo arm were male. Sixty-one percent (61%) of patients were pre- menopausal. Eighty-nine percent (89%) of patients were ECOG performance status 0 and 11% ECOG PS 1. Eighty-two percent (82%) of patients had TNBC and 18% had hormone receptor- positive disease. Fifty percent (50%) of patients had received prior neoadjuvant and 50% received prior adjuvant chemotherapy. Ninety-four percent (94%) of patients received anthracycline and taxane chemotherapy. Twenty-six (26%) of patients overall had received prior platinum for breast cancer. Ninety percent (90%) of patients with hormone receptor positive breast cancer received concurrent endocrine therapy. Patients enrolled based on local gBRCA test results provided a sample for retrospective confirmatory central testing with BRACAnalysis®. Out of 1836 patients enrolled into OlympiA, 1623 were confirmed as gBRCAm by Myriad BRACAnalysis®, either prospectively or retrospectively. A statistically significant improvement in IDFS and OS was demonstrated in patients in the Lynparza arm compared with the placebo arm. Efficacy data for OlympiA (FAS) are presented in Table 10 and Figures 7 and 8. Table 10 Efficacy Results – OlympiA Lynparza tablets Placebo (N=915) (N=921) Invasive Disease Free Survival (IDFS)* Number of events (%) 106 (12) 178 (20) Hazard Ratio (95% CI)† 0.58 (0.46, 0.74) p-value (2-sided)‡ < 0.0001 3-year event-free rate, % (95% CI)§ 86 (82.8, 88.4) 77 (73.7, 80.1) Overall Survival¶ Number of events (%) 75 (8) 109 (12) HR (95% CI)† 0.68 (0.50, 0.91) p-value (2-sided)‡ 0.0091 3-year event-free rate, % (95% CI)§ 93 (90.8, 94.4) 89 (86.7, 91) *Data from the pre-specified interim analysis (86% of the number of events for the planned final analysis). † Based on the stratified Cox's Proportional Hazards Model. ‡ p-value from a stratified log-rank test. Compared with the allocated alpha of 0.005 for IDFS and 0.015 for OS. § Percentage are calculated using Kaplan-Meier estimates. ¶ Data from the pre-specified second interim analysis of OS (at ~330 IDFS events). CI = confidence interval. Figure 7 Kaplan-Meier Curves of IDFS – OlympiA Figure 8 Kaplan-Meier Curves of OS – OlympiA gBRCA1/2-mutated HER2-negative Metastatic Breast Cancer OlympiAD (Study D0819C00003) The safety and efficacy of olaparib in patients with gBRCA1/2-mutations who had HER2-negative metastatic breast cancer were studied in a Phase III randomised, open-label, controlled trial (OlympiAD). In this study 302 patients with a documented deleterious or suspected deleterious gBRCA mutation were randomised 2:1 to receive either Lynparza (300 mg [2 x 150 mg tablets] twice daily) or physician’s choice of chemotherapy (capecitabine 42%, eribulin 35%, or vinorelbine 17%) until progression or unacceptable toxicity. Patients with BRCA1/2 mutations were identified from germline testing in blood via a local test or by central testing at Myriad. Patients were stratified based on: receipt of prior chemotherapy regimens for metastatic breast cancer (yes/no), hormone receptor (HR) positive vs triple negative (TNBC), prior platinum treatment for breast cancer (yes/no). The primary endpoint was PFS assessed by blinded independent central review (BICR) using RECIST 1.1. Secondary endpoints included PFS2, OS, objective response rate (ORR) and HRQoL. Patients must have received treatment with an anthracycline unless contraindicated and a taxane in either a (neo)adjuvant or metastatic setting. Patients with HR+ (ER and/or PgR positive) tumours must have received and progressed on at least one endocrine therapy (adjuvant or metastatic) or had disease that the treating physician believed to be inappropriate for endocrine therapy. Prior therapy with platinum was allowed in the metastatic setting provided there had been no evidence of disease progression during platinum treatment and in the (neo)adjuvant setting provided the last dose was received at least 12 months prior to randomisation. No previous treatment with a PARP inhibitor, including olaparib, was permitted. Demographic and baseline characteristics were generally well balanced between the olaparib and comparator arms (see Table 11). Table 11 Patient demographic and baseline characteristics in OlympiAD Olaparib 300 mg bd Chemotherapy n=205 n=97 Age - year (median) 44 45 Gender (%) Female 200 (98) 95 (98) Male 5 (2) 2 (2) Race (%) White 134 (65) 63 (65) Asian 66 (33) 28 (29) Other 5 (2) 6 (6) ECOG performance status (%) 0 148 (72) 62 (64) 1 57 (28) 35 (36) Overall disease classification Metastatic 205 (100) 97 (100) Locally advanced 0 0 New metastatic breast cancer (%) 26 (13) 12 (12) Hormone receptor status (%) HR+ 103 (50) 49 (51) TNBC 102 (50) 48 (49) gBRCA mutation type (%) gBRCA1 117 (57) 51 (53) gBRCA2 84 (41) 46 (47) gBRCA1 and gBRCA2 4 (2) 0 ≥2 Metastatic sites (%) 159 (78) 72 (74) Location of the metastasis (%) Bone only 16 (8) 6 (6) Other 189 (92) 91 (94) Measurable disease (%) 167 (82) 66 (68) Progressive disease at time of 159 (78) 73 (75) randomization (%) Tumour grade at diagnosis Well differentiated (G1) 5 (2) 2 (2) Moderately differentiated (G2) 52 (25) 23 (24) Poorly differentiated (G3) 108 (53) 55 (57) Undifferentiated (G4) 4 (2) 0 Unassessable (GX) 27 (13) 15 (16) Missing 9 (4) 2 (2) Number of prior lines of chemotherapy for metastatic breast cancer (%) 0 68 (33) 31 (32) 1 80 (39) 42 (43) 2 57 (28) 24 (25) Previous platinum-based therapy(%) 60 (29) 26 (27) in (neo)adjuvant setting 15 (7) 7 (7) metastatic setting 43 (21) 14 (14) in (neo)adjuvant and metastatic setting 3 (1) 1 (1) Previous anthracycline treatment in (neo) adjuvant setting 169 (82) 76 (78) metastatic setting 41 (20) 16 (17) Previous taxane treatment in (neo)adjuvant setting 146 (71) 66 (68) metastatic setting 107 (52) 41 (42) Previous anthracycline and taxane treatment 204 (99.5) 96 (99) As subsequent therapy, 0.5% and 8% of patients received a PARP inhibitor in the treatment and comparator arms, respectively; 29% and 42% of patients, respectively, received subsequent platinum therapy. A statistically significant improvement in PFS, the primary efficacy outcome, was demonstrated for olaparib-treated patients compared with those in the comparator arm (see Table 12 and Figure 9). Table 12 Summary of key efficacy findings for patients with gBRCA1/2-mutated HER2- negative metastatic breast cancer in OlympiAD Olaparib 300 mg bd Chemotherapy PFS (77% maturity) – DCO 09 December 2016 Number of events: Total number of 163:205 (80) 71:97 (73) patients (%) Median time (months) (95% CI) 7.0 (5.7-8.3) 4.2 (2.8- 4.3) HR (95% CI) 0.58 (0.43-0.80) P value (2-sided)a p=0.0009 PFS2 (65% maturity) - DCO 25 September 2017b Number of events: Total number of patients (%) 130:205 (63) 65:97 (67) Median time (months) (95% CI) 12.8 (10.9-14.3) 9.4 (7.4- 10.3) HR (95% CI) 0.55 (0.39-0.77) P value (2-sided)a p=0.0005 OS (64% maturity) – DCO 25 September 2017 Number of events: Total number of patients (%) 130:205 (63) 62:97 (64) Median time (months) (95% CI) 19.3 (17.2-21.6)c 17.1 (13.9- 21.9) HR (95% CI) 0.90 (0.66-1.23) P value (2-sided)a p=0.5131 Confirmed ORR – DCO 09 December 2016 Number of objective responders: Total number of patients with measurable disease (%) 87: 167 (52)d 15:66 (23) 95% CI 44.2-59.9 13.3-34.7 DOR – DCO 09 December 2016 Median, months (95% CI) 6.9 (4.2, 10.2) 7.9 (4.5, 12.2) a Based on stratified log-rank test. b Post-hoc analysis. c The median follow-up time in censored patients was 25.3 months for olaparib versus 26.3 months for comparator. d Confirmed responses (by BICR) were defined as a recorded response of either CR/PR, confirmed by repeat imaging not less than 4 weeks after the visit when the response was first observed. In the olaparib arm 8% with measurable disease had a complete response versus 1.5% of patients in the comparator arm; 74/167 (44%) of patients in the olaparib arm had a partial response versus 14/66 (21%) of patients in the chemotherapy arm. In the TNBC patient subgroup the confirmed ORR was 48% (41/86) in the olaparib arm and 12% (4/33) in the comparator arm. In the HR+ patient subgroup the confirmed ORR was 57% (46/81) in the olaparib arm and 33% (11/33) in the comparator arm. bd Twice daily; CI Confidence interval; DOR Duration of response; DCO Data cut off; HR Hazard ratio; HR+ Hormone receptor positive, ORR Objective response rate; OS overall survival; PFS progression-free survival; PFS2 Time to second progression or death, TNBC triple negative breast cancer. Figure 9 OlympiAD: Kaplan-Meier plot of BICR PFS in patients with gBRCA1/2-mutated HER2-negative metastatic breast cancer (77% maturity) DCO 09 December 2016 Consistent results were observed in all predefined patient subgroups (see Figure 8). Subgroup analysis indicated PFS benefit of olaparib versus comparator in TNBC (HR 0.43; 95% CI: 0.29- 0.63, n=152) and HR+ (HR 0.82; 95% CI: 0.55-1.26, n=150) patient subgroups. Figure 10 PFS (BICR), Forest plot, by prespecified subgroup In a post-hoc analysis of the subgroup of patients that had not progressed on chemotherapy other than platinum, the median PFS in the olaparib arm (n=22) was 8.3 months (95% CI 3.1- 16.7) and 2.8 months (95% CI 1.4-4.2) in the chemotherapy arm (n=16) with a HR of 0.54 (95% CI 0.24-1.23). However, the number of patients is too limited to make meaningful conclusions on the efficacy in this subgroup. Seven male patients were randomised (5 olaparib and 2 comparator). At the time of the PFS analysis, 1 patient had a confirmed partial response with a duration of response of 9.7 months in the olaparib arm. There were no confirmed responses in the comparator arm. Figure 11 OlympiAD: Kaplan-Meier plot of OS in patients with gBRCA1/2-mutated HER2- negative metastatic breast cancer (64% maturity) DCO 25 September 2017 OS analysis in patients with no prior chemotherapy for metastatic breast cancer indicated benefit in these patients with a HR of 0.45 (95% CI 0.27-0.77), while for further lines of therapy HR exceeded 1. Paediatric population The European Medicines Agency has waived the obligation to submit the results of studies with Lynparza in all subsets of the paediatric population, in ovarian carcinoma (excluding rhabdomyosarcoma and germ cell tumours) (see section 4.2 for information on paediatric use). First-line Maintenance Treatment of Germline BRCA-mutated Metastatic Pancreatic Adenocarcinoma POLO The safety of Lynparza as maintenance treatment of germline BRCA-mutated metastatic pancreatic adenocarcinoma following first-line treatment with platinum-based chemotherapy was evaluated in POLO . Patients received Lynparza tablets 300 mg orally twice daily (n=90) or placebo (n=61) until disease progression or unacceptable toxicity. Among patients receiving Lynparza, 34% were exposed for 6 months or longer and 25% were exposed for greater than one year. Among patients who received Lynparza, dosage interruptions due to an adverse reaction of any grade occurred in 35% and dosage reductions due to an adverse reaction occurred in 17%. The most frequent adverse reactions leading to dosage interruption or reduction in patients who received Lynparza were anemia (11%), vomiting (5%), abdominal pain (4%), asthenia (3%), and fatigue (2%). Discontinuation due to adverse reactions occurred in 6% of patients receiving Lynparza. The most frequent adverse reaction that led to discontinuation of Lynparza was fatigue (2.2%). Tables 13 and 14 summarize the adverse reactions and laboratory abnormalities in patients in POLO. Table 13 Adverse Reactions* in POLO (Occurring in ≥10% of Patients who Received Lynparza) Adverse Reaction Lynparza tablets Placebo (n=91)† (n=60)† All Grades Grades All Grades ( %) 3 – 4 (%) Grades (%) 3 – 4 (%) General Disorders and Administration Site Conditions Fatigue‡ 60 5 35 2 Gastrointestinal Disorders Nausea 45 0 23 2 Abdominal pain^ 34 2 37 5 Diarrhea 29 0 15 0 Constipation 23 0 10 0 Vomiting 20 1 15 2 Stomatitis§ 10 0 5 0 Blood and Lymphatic System Disorders Anemia 27 11 17 3 Thrombocytopenia¶ 14 3 7 0 Neutropeniaǁ 12 4 8 3 Metabolism and Nutrition Disorders Decreased appetite 25 3 7 0 Musculoskeletal and Connective Tissue Disorders Back pain 19 0 17 2 Adverse Reaction Lynparza tablets Placebo (n=91)† (n=60)† All Grades Grades All Grades ( %) 3 – 4 (%) Grades (%) 3 – 4 (%) Arthralgia 15 1 10 0 Skin and Subcutaneous Tissue Disorder Rash# 15 0 5 0 Respiratory, Thoracic and Mediastinal Disorders Dyspnea** 13 0 5 2 Infections and Infestations Nasopharyngitis 12 0 3 0 Nervous System Disorders Dysgeusia 11 0 5 0 * Graded according to NCI CTCAE, version 4.0 † This number represents the safety population. The derived values in the table are based on the total number of evaluable patients for each laboratory parameter. ‡ Includes asthenia and fatigue ^ Includes abdominal pain, abdominal pain upper, abdominal pain lower § Includes stomatitis and mouth ulceration ǁ Includes neutropenia, febrile neutropenia and neutrophil count decreased ¶ Includes platelets count decreased and thrombocytopenia # Includes rash erythematous, rash macular and rash maculo-papular **Includes dyspnea and dyspnea exertional In addition, the adverse reactions observed in POLO that occurred in <10% of patients receiving Lynparza were cough (9%), abdominal pain upper (7%), blood creatinine increased (7%), dizziness (7%), headache (7%), dyspepsia (5%), leukopenia (5%), hypersensitivity (2%) and lymphopenia (2%). Table 14 Laboratory Abnormalities Reported in ≥25% of Patients in POLO Laboratory Lynparza tablets Placebo Parameter* n†=91 n†=60 Grades 1-4 Grades 3-4 Grades Grades 3-4 (%) (%) 1-4 (%) (%) Increase in serum 99 2 85 0 creatinine Decrease in 86 11 65 0 hemoglobin Increase in mean 71 - 30 - corpuscular volume‡ Decrease in 61 9 27 0 lymphocytes Decrease in platelets 56 2 39 0 Decrease in leukocytes 50 3 23 0 Decrease in absolute 25 3 10 0 neutrophil count * Patients were allowed to enter POLO with hemoglobin ≥9 g/dL (CTCAE Grade 2) and other laboratory values of CTCAE Grade 1. † This number represents the safety population. The derived values in the table are based on the total number of evaluable patients for each laboratory parameter. ‡ Represents the proportion of subjects whose mean corpuscular volume was > ULN. First-Line Maintenance Treatment of Germline BRCA-mutated Metastatic Pancreatic Adenocarcinoma The efficacy of Lynparza was evaluated in POLO (NCT02184195), a randomized (3:2), double-blind placebo-controlled, multi-center trial. Patients were required to have metastatic pancreatic adenocarcinoma with a deleterious or suspected deleterious germline BRCA mutation (gBRCAm) and absence of disease progression after receipt of first-line platinum-based chemotherapy for at least 16 weeks. Patients were randomized to receive Lynparza tablets 300 mg orally twice daily or placebo until disease progression or unacceptable toxicity. The major efficacy outcome measure was PFS by BICR using RECIST, version 1.1 modified to assess patients with clinical complete response at entry who were assessed as having no evidence of disease unless they had progressed based on the appearance of new lesions. Additional efficacy outcome measures were OS and ORR. A total of 154 patients were randomized, 92 to Lynparza and 62 to placebo. The median age was 57 years (range 36 to 84); 54% were male; 92% were White, 4% were Asian and 3% were Black; baseline ECOG PS was 0 (67%) or 1 (31%). The median time from initiation of first-line platinum-based chemotherapy to randomization was 5.8 months (range 3.4 to 33.4 months). Seventy-five percent (75%) of patients received FOLFIRINOX with a median of 9 cycles (range 4-61), 8% received FOLFOX or XELOX, 4% received GEMOX, and 3% received gemcitabine plus cisplatin; 49% achieved a complete or partial response to platinum-based chemotherapy. All patients had a deleterious or suspected deleterious germline BRCA-mutation as detected by the Myriad BRACAnalysis® or BRACAnalysis CDx® at a central laboratory only (n=106), local BRCA test only (n=4), or both local and central testing (n=44). Among the 150 patients with central test results, 30% had a mutation in BRCA1; 69% had a mutation in BRCA2; and 1 patient (1%) had mutations in both BRCA1 and BRCA2. POLO demonstrated a statistically significant improvement in BICR-assessed PFS in patients randomized to Lynparza as compared with placebo. The final analysis of OS did not reach statistical significance Efficacy results of POLO are provided in Table 15 and Figure 12. Table 15 Efficacy Results - POLO (BICR-assessed) Lynparza tablets Placebo (n=92) (n=62) Progression-Free Survival Number of events (%)* 60 (65%) 44 (71%) Median, months (95% CI) 7.4 (4.1, 11.0) 3.8 (3.5, 4.9) Hazard ratio** (95% CI) 0.53 (0.35, 0.81) p-value 0.0035 Overall Survival Number of events (%) 61 (66) 47 (76) Median, months (95% CI) 19.0 (15.3, 26.3) 19.2 (14.3, 26.1) Hazard ratio† (95% CI) 0.83 (0.56, 1.22) p-value 0.3487 Patients with Measurable Disease n=78 n=52 Objective Response Rate (95% CI) 23% (14, 34) 12% (4, 23) Complete response (%) 2 (2.6) 0 Partial response (%) 16 (21) 6 (12) Duration of Response (DOR) Median time in months (95% CI) 25 (15, NC) 4 (2, NC) * Number of events: Progression – Lynparza 55, placebo 44; death before BICR-documented progression – Lynparza 5, placebo 0 ** Hazard ratio, 95% CI, and p-value calculated from a log-rank test. A hazard ratio <1 favors Lynparza. NC Not calculable Figure12 Kaplan-Meier Curves of BICR-Assessed Progression-Free Survival - POLO First-line Maintenance Treatment of Advanced Ovarian Cancer in Combination with Bevacizumab PAOLA-1 The safety of Lynparza in combination with bevacizumab for the maintenance treatment of patients with advanced ovarian cancer following first-line treatment containing platinum-based chemotherapy and bevacizumab was investigated in PAOLA-1. This study was a placebo-controlled, double-blind study in which 802 patients received either Lynparza 300 mg BID in combination with bevacizumab (n=535) or placebo in combination with bevacizumab (n=267) until disease progression or unacceptable toxicity. The median duration of treatment with Lynparza was 17.3 months and 11 months for bevacizumab post-randomization on the Lynparza/bevacizumab arm. Fatal adverse reactions occurred in 1 patient due to concurrent pneumonia and aplastic anemia. Serious adverse reactions occurred in 31% of patients who received Lynparza/bevacizumab. Serious adverse reactions in >5% of patients included hypertension (19%) and anemia (17%). Dose interruptions due to an adverse reaction of any grade occurred in 54% of patients receiving Lynparza/bevacizumab and dose reductions due to an adverse reaction occurred in 41% of patients who received Lynparza/bevacizumab. The most frequent adverse reactions leading to dose interruption in the Lynparza/bevacizumab arm were anemia (21%), nausea (7%), vomiting (3%), and fatigue (3%), and the most frequent adverse reactions leading to reduction in the Lynparza/bevacizumab arm were anemia (19%), nausea (7%), and fatigue (4%). Discontinuation due to adverse reactions occurred in 20% of patients receiving Lynparza/bevacizumab. Specific adverse reactions that most frequently led to discontinuation in patients treated with Lynparza/bevacizumab were anemia (4%) and nausea (3%). The most common adverse reactions (≥ 10%) for patients receiving Lynparza/bevacizumab irrespective of the frequency compared with the placebo/bevacizumab arm were nausea (53%), fatigue (including asthenia) (53%), anemia (41%), lymphopenia (24%), vomiting (22%), diarrhea (18%), neutropenia (18%), leukopenia (18%), urinary tract infection (15%), and headache (14%). Tables 16 and 17 summarize adverse reactions and laboratory abnormalities in PAOLA-1, respectively. Table 16 Adverse Reactions* Occurring in ≥10% of Patients Treated with Lynparza/bevacizumab in PAOLA-1 and at ≥5% Frequency Compared to the Placebo/bevacizumab Arm Lynparz a n=267 n=535 Grades 1- Grades 3- Grades 1- Grades 3-4 4 4 (%) 4 (%) (%) (%) General Disorders and Administration Site Conditions † 53 5 32 1.5 53 2.4 22 0.7 22 1.7 11 1.9 Blood and Lymphatic Disorders Anemia‡ 41 17 10 0.4 § 24 7 9 1.1 ǁ 18 1.9 10 1.5 Leukopenia * Graded according to the National Cancer Institute Common T erminology Criteria for Adverse Events (NCI CTCAE), version 4.0. † Includes asthenia, and fatigue. ‡ Includes anemia, anemia macrocytic, erythropenia, haematocrit decreased, haemoglobin decreased, normochromic anemia, normochromic normocytic anemia, normocytic anemia, and red blood cell count decreased. § Includes B-lymphocyte count decreased, lymphocyte count decreased, lymphopenia, and T-lymphocyte count decreased. ǁ Includes leukopenia, and white blood cell count decreased. Clinically relevant adverse reactions that occurred in <10% of patients receiving Lynparza/bevacizumab were dysgeusia (8%), dyspnea (8%), stomatitis (5%), dyspepsia (4.3%), erythema (3%), dizziness (2.6%), hypersensitivity (1.7%) and MDS/AML (0.7%). Venous thromboembolism occurred more commonly in patients receiving Lynparza/bevacizumab (5%) than in those receiving placebo/bevacizumab (1.9%). Table 17 Laboratory Abnormalities Reported in ≥25% of Patients in PAOLA-1* Lynparza/bevacizumab Placebo/bevacizumab Laboratory Parameter† n†=535 n‡=267 Grades 1-4 Grades 3-4 Grades 1-4 Grades 3-4 (%) (%) (%) (%) 79 13 55 0.4 63 10 42 3.0 61 0.4 36 0.4 59 3.4 45 2.2 35 7 30 3.7 Decrease in platelets 35 2.4 28 0.4 * Reported within 30 days of the last dose. † Patients were allowed to enter clinical studies with laboratory values of CTCAE Grade 1. ‡ This number represents the safety population. The derived values in the table are based on the total number of evaluable patients for each laboratory parameter. PAOLA-1 (NCT03737643) was a randomized, double-blind, placebo-controlled, multi-center trial that compared the efficacy of Lynparza in combination with bevacizumab versus placebo/bevacizumab for the maintenance treatment of advanced high-grade epithelial ovarian cancer, fallopian tube or primary peritoneal cancer following first-line platinum-based chemotherapy and bevacizumab. Randomization was stratified by first-line treatment outcome (timing and outcome of cytoreductive surgery and response to platinum-based chemotherapy) and tBRCAm status, determined by prospective local testing. All available clinical samples were retrospectively tested with Myriad myChoice® CDx. Patients were required to have no evidence of disease (NED) due to complete surgical resection, or who were in complete response (CR), or partial response (PR) following completion of first-line platinum-containing chemotherapy and bevacizumab. Patients were randomized (2:1) to receive Lynparza tablets 300 mg orally twice daily in combination with bevacizumab (n=537) 15 mg/kg every three weeks or placebo/bevacizumab (n=269) Patients continued bevacizumab in the maintenance setting and started treatment with Lynparza after a minimum of 3 weeks and up to a maximum of 9 weeks following completion of their last dose of chemotherapy. Lynparza treatment was continued for up to 2 years or until progression of the underlying disease or unacceptable toxicity. Patients who in the opinion of the treating physician could derive further benefit from continuous treatment could be treated beyond 2 years. Treatment with bevacizumab was for a total of up to 15 months, including the period given with chemotherapy and given as maintenance. The major efficacy outcome measure was investigator-assessed PFS evaluated according to RECIST, version 1.1. An additional efficacy endpoint was overall survival (OS). A statistically significant difference in PFS was observed in the intent-to-treat (ITT) population. Planned exploratory analyses of PFS and OS were conducted in patients with known HRD status. The PFS hazard ratio (HR) for patients with HRD-negative tumors (277/806; 34%) was 1.00 (95% CI: 0.75, 1.34) and the OS HR was 1.18 (95% CI: 0.87, 1.60) indicating that the clinical benefit was primarily attributed to the results seen in the HRD-positive population. Efficacy results in patients with HRD-positive tumors are summarized in Table 19, Figure 13, and Figure 14. Among the 387 patients (48%) with HRD-positive tumors identified post-randomization using the Myriad myChoice® HRD Plus tumor test the median age was 58 years in both arms (range 32-82). Ovarian cancer was the primary tumor type in 87% of patients in both arms. Ninety five percent (95%) were serous histological type. The ECOG performance score was 0 in 75% of patients and 1 in 24% of patients. All patients had received first-line platinum-based therapy and bevacizumab. First-line treatment outcomes at screening indicated that patients had no evidence of disease with complete macroscopic resection at initial debulking surgery (36%), no evidence of disease/ CR with complete macroscopic resection at interval debulking surgery (29%, both arms), no evidence of disease/ CR in patients who had either incomplete resection (at initial or interval debulking surgery) or no debulking surgery (16%, both arms) and patients with a partial response (19%, both arms). Sixty-two (62%) of patients in Lynparza/bevacizumab arm and 58% of patients in placebo/bevacizumab armhad tumors with a deleterious BRCA mutation. Patients were not restricted by the surgical outcome with 67% having complete cytoreduction at initial or interval debulking surgery and 33% having residual macroscopic disease. Table 18 EfficacyResults - PAOLA-1 (HRD positive status*, Investigator Assessment) Lynparza/bevacizumab Placebo/bevacizumab (n=255) (n=132) Progression-Free Survival Number of events (%) 87 92 (34%) (70%) Median, months 37.2 17.7 Hazard ratioa (95% CI) 0.33 (0.25, 0.45) Overall Survival‡ Number of events (%) 93 (36%) 69 (52%) Median, months 75.2 57.3 Hazard ratio† (95% CI) 0.62 (0.45, 0.85) * Results from a blinded independent review of PFS were consistent with those from investigator-assessed PFS.a The analysis was performed using an unstratified Cox proportional hazards model. ‡ Based on final OS subgroup analysis. CI Confidence interval Figure 13 Kaplan-Meier Curves of Investigator-Assessed Progression-Free Survival – PAOLA-1 (HRD positive status) Figure 14 Kaplan-Meier Curves of Overall Survival – PAOLA-1 (HRD-positive status)* * Based on final OS subgroup analysis. BRCA1/2 or ATM Gene-mutated Metastatic Castration-Resistant Prostate Cancer PROfound The safety of Lynparza as monotherapy was evaluated in patients with mCRPC and BRCA1/2 or ATM gene mutations who have progressed following prior treatment with enzalutamide or abiraterone in PROfound . This study was a randomized, open-label, multi-center study in which 386 patients received either Lynparza tablets 300 mg orally twice daily (n=256) or investigator’s choice of enzalutamide or abiraterone acetate (n=130) until disease progression or unacceptable toxicity. Among patients receiving Lynparza, 62% were exposed for 6 months or longer and 20% were exposed for greater than one year. Fatal adverse reactions occurred in 4% of patients treated with Lynparza. These included pneumonia (1.2%), cardiopulmonary failure (0.4%), aspiration pneumonia (0.4%), intestinal diverticulum (0.4%), septic shock (0.4%), Budd-Chiari Syndrome (0.4%), sudden death (0.4%), and acute cardiac failure (0.4%). Serious adverse reactions occurred in 36% of patients receiving Lynparza. The most frequent serious adverse reactions (≥2%) were anemia (9%), pneumonia (4%), pulmonary embolism (2%), fatigue/asthenia (2%), and urinary tract infection (2%). Dose interruptions due to an adverse reaction of any grade occurred in 45% of patients receiving Lynparza; dose reductions due to an adverse reaction occurred in 22% of Lynparza patients. The most frequent adverse reactions leading to dose interruption of Lynparza were anemia (25%) and thrombocytopenia (6%) and the most frequent adverse reaction leading to reduction of Lynparza was anemia (16%). Discontinuation due to adverse reactions occurred in 18% of Lynparza. The adverse reaction that most frequently led to discontinuation of Lynparza was anemia (7%). Tables 19 and 20 summarize the adverse reactions and laboratory abnormalities, respectively, in patients in PROfound. * Table 19 Adverse Reactions Reported in ≥10% of Patients in PROfound Adverse Reactions Lynparza tablets n=256 Enzalutamide or abiraterone n=130 Grades 1-4 Grades 3-4 Grades 1-4 Grades 3-4 (%) (%) (%) (%) Blood and lymphatic disorders Anemia† 46 21 15 5 Thrombocytopenia‡ 12 4 3 0 Gastrointestinal disorders Nausea 41 1 19 0 Diarrhea 21 1 7 0 Vomiting 18 2 12 1 General disorders and administration site conditions Fatigue (including asthenia) 41 3 32 5 Metabolism and nutrition disorders Decreased appetite 30 1 18 1 Respiratory, thoracic, and mediastinal disorders Cough 11 0 2 0 Dyspnea 10 2 3 0 * Graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE), version 4.03 † Includes anemia and hemoglobin decreased ‡ Includes platelet count decreased and thrombocytopenia In addition, adverse reactions of clinical relevance in PROfound that occurred in <10% of patients receiving Lynparza were neutropenia (9%), venous thromboembolic events (7%), dizziness (7%), dysgeusia (7%), dyspepsia (7%), headache (6%), pneumonia (5%), stomatitis (5%), rash (4%), blood creatinine increase (4%), pneumonitis (2%), upper abdominal pain (2%), and hypersensitivity (1%). Table 20 Laboratory Abnormalities Reported in ≥25% of Patients in PROfound Lynparza tablets Enzalutamide or abiraterone Laboratory n†= 256 n†=130 Parameter* Grades 1-4 Grades 3-4 Grades 1-4 Grades 3-4 n= 247 (%) n=247 (%) n=124 (%) n=124 (%) Decrease in 242 (98) 33 (13) 91 (73) 5 (4) hemoglobin Decrease in 154 (62) 57 (23) 42 (34) 16 (13) lymphocytes Decrease in 130 (53) 9 (4) 26 (21) 0 leukocytes Decrease in absolute 83 (34) 8 (3) 11 (9) 0 neutrophil count * Patientswere allowed to enter clinical studies with laboratory values of CTCAE Grade 1. † Thisnumber represents the safety population. The derived values in the table are based on the total number of evaluable patients for each laboratory parameter. BRCA1/2 or ATM Gene-mutated Metastatic Castration-Resistant Prostate Cancer The efficacy of Lynparza was evaluated in PROfound (NCT02987543), randomized, open-label, multi- center trial that evaluated the efficacy of Lynparza 300 mg twice daily versus a comparator arm of investigator’s choice of enzalutamide or abiraterone acetate in men with metastatic castration- resistant prostate cancer (mCRPC). All patients received a GnRH analog or had prior bilateral orchiectomy. Patients needed to have progressed on prior enzalutamide or abiraterone for the treatment of metastatic prostate cancer and/or CRPC and have a tumor mutation in one of 15 genes involved in the homologous recombination repair (HRR) pathway. Patients were divided into two cohorts based on HRR gene mutation status. Patients with mutations in either BRCA1, BRCA2, or ATM were randomized in Cohort A; patients with mutations among 12 other genes involved in the HRR pathway (BARD1, BRIP1, CDK12, CHEK1, CHEK2, FANCL, PALB2, PPP2R2A, RAD51B, RAD51C, RAD51D, or RAD54L) were randomized in Cohort B; patients with co-mutations (BRCA1, BRCA2, or ATM plus a Cohort B gene) were assigned to Cohort A. Although patients with PPP2R2A gene mutations were enrolled in the trial, Lynparza is not indicated for the treatment of patients with this gene mutation due to unfavorable risk-benefit. Patients were randomized (2:1), 256 to Lynparza arm and 131 to enzalutamide or abiraterone acetate arm; in Cohort A there were 245 (162 Lynparza arm and 83 in enzalutamide or abiraterone acetate arm) and in Cohort B there were 142 patients (94 in Lynparza arm and 48 in enzalutamide or abiraterone acetate arm). Randomization was stratified by prior receipt of taxane chemotherapy and presence of measurable disease by RECIST 1.1. Treatment was continued until objective radiological disease progression determined by BICR. Upon radiological progression confirmed by BICR, patients randomized to enzalutamide or abiraterone acetate were given the option to switch to olaparib. Patients with HRR gene mutations were identified by tissue-based testing using the Foundation Medicine FoundationOne® clinical trial HRR assay performed at a central laboratory. Determination of deleterious or suspected deleterious somatic or germline HRR mutation status in line with the FDA approved mutation classification and testing criteria for the Foundation Medicine F1CDx tissue-based assay and assessment of the germline-BRCA status using the Myriad BRAC Analysis CDx blood-based assay was performed retrospectively. Representation of individual gene mutations by cohort is provided in Table 17. No patients were enrolled who had mutations in two of the 15 pre-specified HRR genes: FANCL and RAD51C. Table 21 Frequency of Patients with HRR Mutations Enrolled in PROfound HRR Mutation Cohort A Cohort B* N=245 N=142 n (%) n (%) Single mutation 224 (91) 135 (95) BRCA2 127 (52) 1 (<1) ATM 84 (34) 2 (1) BRCA1 13 (5) 0 CDK12 0 89 (63) CHEK2 0 12 (8) PPP2R2A# 0 10 (7) RAD51B 0 5 (4) RAD54L 0 5 (4) PALB2 0 4 (3) BRIP1 0 3 (2) CHEK1 0 2 (1) BARD1 0 1 (<1) RAD51D 0 1 (<1) Co-occurring mutation** 21 (9) 7 (5) * Three patients with single BRCA2 or ATM gene mutations and 1 patient with co-occurring BRCA2+CDK12 gene mutations were incorrectly assigned to Cohort B. # Lynparza is not indicated for patients with PPP2R2A mutations. ** Patients with co-occurring mutations (BRCA1, BRCA2, or ATM plus a Cohort B gene) were assigned to Cohort A. In Cohort A+B, the median age was 69 years (range: 47 to 91 years) in both arms; 69% were White, 29% were Asian, and 1% were Black. The ECOG performance score was 0 or 1 in most patients (95%) in both arms. In patients treated with Lynparza, the proportion of patients with RECIST 1.1 measurable disease at baseline was 58%, including 17% with lung and 10% with liver metastases, respectively. At randomization, 66% of patients had received prior taxane chemotherapy, 40% had received enzalutamide, 38% had received abiraterone acetate, and 20% had received both enzalutamide and abiraterone acetate. Patient characteristics were well-balanced between arms. The major efficacy outcome of the study was radiological progression free survival (rPFS) (Cohort A) as determined by BICR using RECIST version 1.1 and Prostate Cancer Clinical Trials Working Group 3 (PCWG3) (bone) criteria. Additional efficacy outcomes included confirmed objective response rate (ORR) (Cohort A), rPFS (combined Cohorts A+B) as assessed by BICR, and overall survival (OS) (Cohort A). PROfound demonstrated a statistically significant improvement in BICR-assessed rPFS for Lynparza compared to investigator’s choice of enzalutamide or abiraterone acetate in Cohort A and Cohort A+B. In an exploratory analysis for patients in Cohort B, the median rPFS was 4.8 months for Lynparza vs 3.3 months for comparator with a HR of 0.88 (95% CI 0.58, 1.36). The major efficacy outcome was supported by a statistically significant improvement in ORR by BICR for patients with measurable disease at baseline in Cohort A. In Cohort B, ORR by BICR was 3.7% (95% CI 0.5, 12.7) in Lynparza treated patients and 8.3% (95% CI 1.0, 27.0) in patients treated with enzalutamide or abiraterone acetate. The final analysis of overall survival (OS) demonstrated a statistically significant improvement in OS in patients randomized to Lynparza compared to patients in the enzalutamide or abiraterone acetate arm in Cohort A. Efficacy results of PROfound are provided in Tables 22 and 23 and Figures 14 and 15. Table 22 Efficacy Results -PROfound (BICR-assessed) * Although 10 patients with PPP2R2A mutation were included in all analyses of Cohort A+B, Lynparza is not indicated for this population due to unfavorable risk-benefit. ǁ The HR and CI were calculated using a Cox proportional hazards model adjusted for prior taxane use and measurable disease. An HR <1 favors Lynparza 300 mg bd. ¶ The analysis was performed using the log-rank test stratified by prior taxane use and measurable disease. CI Confidence interval Figure 15 Kaplan-Meier Curves of BICR-Assessed Radiological Progression-Free Survival – PROfound – Cohort A Consistent results were observed in exploratory analyses of rPFS for patients who received or did not receive prior taxane therapy and for those with germline-BRCA mutations identified using the Myriad BRACAnalysis CDx assay compared with those with BRCA mutations identified using the Foundation Medicine F1CDx assay. Figure 16 Kaplan-Meier Curves of Overall Survival – PROfound – Cohort A Response data by HRR mutations for patients in the Lynparza arm are presented in Table 27. In the comparator arm of Cohorts A and B, a total of three patients achieved a partial response, including one patient with an ATM mutation alone and 2 patients with co-occurring mutations (one with PALB2+PPP2R2A and one with CDK12+PALB2). Table 23 Response Rate and Duration of Response by HRR Mutation in Patients withMeasurable Disease at Baseline on the Lynparza Arm – PROfound (BICR-assessed) * No patients with FANCL or RAD51C enrolled. Three patients with PPP2R2A mutations had measurable disease, however, Lynparza is not indicated for patients with PPP2R2A mutation. † In patients with a single BRCA2 mutation the median duration of response in the Lynparza arm (n=24) was 5.6 months (95% C.I: 5.5, 9.2). In the 3 responders with a single ATM mutation in the Lynparza arm, the duration of response ranged from 5.8+ to 9.0 months. In the 2 responders with a single CDK12 mutation in the Lynparza arm, the duration of response was 3.7 and 7.2 months. + denotes ongoing response. PR Partial response; SD Stable disease; PD Progressive disease; NE Not evaluable; NA Not applicable due to small numbers or lack of response. Treatment of patients in the first-line mCRPC setting PROpel The safety and efficacy of olaparib were studied in men with metastatic castration-resistant prostate cancer (mCRPC) in a Phase III randomised, double-blind, placebo-controlled, multicentre study that evaluated the efficacy of Lynparza (300 mg [2 x 150 mg tablets] twice daily) in combination with abiraterone (1000 mg [2 x 500 mg tablets] once daily) versus a comparator arm of placebo plus abiraterone. Patients in both arms also received either prednisone or prednisolone 5 mg twice daily. The study randomised 796 patients (1:1 randomisation; 399 olaparib/abiraterone:397 placebo/ abiraterone) who had evidence of histologically confirmed prostate adenocarcinoma and metastatic status defined as at least one documented metastatic lesion on either a bone or CT/MRI scan and who were treatment naïve with no prior chemotherapy or NHA in the mCRPC setting. Prior to the mCRPC stage, treatment with NHAs (except abiraterone) without PSA progression (clinical or radiological) during treatment was allowed, provided the treatment was stopped at least 12 months before randomisation. Treatment with first- generation antiandrogen agents (e.g., bicalutamide, nilutamide, flutamide) was also allowed, provided there was a washout period of 4 weeks. Docetaxel treatment was allowed during neoadjuvant/adjuvant treatment for localised prostate cancer and at metastatic hormone-sensitive prostate cancer (mHSPC) stage, as long as no signs of disease progression occurred during or immediately after such treatment. All patients received a GnRH analogue or had prior bilateral orchiectomy. Patients were stratified by metastases (bone only, visceral or other) and docetaxel treatment at mHSPC stage (yes or no). Treatment was continued until radiological progression of the underlying disease or unacceptable toxicity. Demographic and baseline characteristics were balanced between the two treatment arms. The median age of patients was 69 years overall, and the majority (71%) of patients were in the ≥65 years age group. One hundred and eighty-nine patients (24%) had prior docetaxel treatment at mHSPC stage. In total, 434 (55%) patients had bone metastases (metastases in the bone and no other distant site), 105 (13%) patients had visceral metastases (distant soft tissue metastases in an organ e.g., liver, lung) and 257 (32%) patients had other metastases (this could include, for example, patients with bone metastases and distant lymph nodes or patients with disease present only in distant lymph nodes). Most patients in both arms (70%) had an ECOG performance status of 0. There were 103 (25.8%) symptomatic patients in the olaparib group and 80 (20.2%) patients in the placebo group. Symptomatic patients were characterized by Brief Pain Inventory-Short Form (BPI-SF) item #3 score ≥ 4 and/or opiate use at baseline. Patient enrolment was not based on biomarker status. HRR gene mutation status was assessed retrospectively by ctDNA and tumour tissue tests to assess the consistency of treatment effect from the FAS population. Of the patients tested, 198 and 118 were HRRm as determined by ctDNA and tumour tissue, respectively. The distribution of HRRm patients was well balanced between the two arms. The primary endpoint was rPFS, defined as time from randomisation to radiological progression determined by investigator assessment based on RECIST 1.1 and PCWG-3 criteria (bone). The key secondary efficacy endpoint was overall survival (OS). Additional secondary endpoints included PFS2, TFST and HRQoL. The study met its primary endpoint demonstrating a statistically significant improvement in the risk of radiological disease progression or death for olaparib/abiraterone compared to placebo/abiraterone as assessed by the investigator, with HR 0.66; 95% CI 0.54, 0.81; p<0.0001; median rPFS 24.8 months in the olaparib/abiraterone arm vs 16.6 months in the placebo/abiraterone arm. The investigator assessment of rPFS was supported with a blinded independent central radiological (BICR) review. The sensitivity analysis of rPFS by BICR was consistent with the investigator-based analysis with HR 0.61; 95% CI 0.49, 0.74; p<0.0001; median rPFS 27.6 months in the olaparib/abiraterone arm vs 16.4 months in the placebo/abiraterone arm, respectively. Subgroup results were consistent with the overall results for olaparib/abiraterone compared to placebo/abiraterone in all pre-defined sub-groups, including patients with or without prior taxane at mHSPC stage, patients with different metastatic disease at baseline (bone only vs visceral vs other) and patients with or without HRRm (Figure 19). Efficacy results are presented in Table 15, Table 16, Figure 17 and Figure 18. Table 15 Summary of key efficacy findings for treatment of patients with mCRPC in PROpel arib/abiraterone N = 399cebo/abiraterone N = 397 rPFS (by investigator assessment) (50% maturity) (DCO 30 July 2021) Number of events: Total number of patients (%) 168:399 (42.1) 226:397 (56.9) Median time (95% CI) (months) 24.8 (20.5, 27.6) 16.6 (13.9, 19.2) HR (95% CI)a 0.66 (0.54, 0.81) p-valueb <0.0001 Final OS (48% maturity) (DCO 12 October 2022) Number of events: Total number of patients (%) 176:399 (44.1) 205:397 (51.6) Median time (95% CI) (months) 42.1 (38.4, 34.7 (31.0, NC) 39.3) Olaparib/abiraterone Placebo/abirateron N = 399 e N = 397 HR (95% CI)a 0.81 (0.67, 1.00) p-valueb p=0.054 4 % Alive at 36 months (95% CI) c 56.9 (51.7, 61.7) 49.5 (44.3, 54.5) aThe HR and CI were calculated using a Cox proportional hazards model adjusted for the variables selected in the primary pooling strategy: metastases, docetaxel treatment at mHSPC stage. The Efron approach was used for handling ties. A HR <1 favours olaparib 300 mg bd + abiraterone 1000 mg qd. b The 2-sided p-value was calculated using the log-rank test stratified by the same variables selected in the primary pooling strategy. c Calculated using the Kaplan-Meier technique. 1.2 Table 16 rPFS subgroup analyses by investigator assessment – PROpel (DCO 30 July 2021) Olaparib/abirateron Placebo/abirateron e e Radiological Progression-Free Survival (rPFS) by investigator assessment Aggregate HRRm Subgroup Analyses a HRRm N=111 N=115 Number of events: Total number of patients 43:111 (38.7) 73:115 (63.5) (%) Median (months) NC 13.86 b Hazard ratio (95% CI) 0.50 (0.34, 0.73) Non-HRRm N=279 N=273 Number of events: Total number of patients 119:279 (42.7) 149:273 (54.6) (%) Median (months) 24.11 18.96 Hazard ratio (95% CI) b 0.76 (0.60, 0.97) a Aggregate BRCAm Subgroup Analyses BRCAm N=47 N=38 Number of events: Total number of patients 14:47 (29.8) 28:38 (73.7) (%) Median (months) NC 8.38 Hazard ratio (95% CI) b 0.23 (0.12, 0.43) Non-BRCAm N=343 N=350 Number of events: Total number of patients 148:343 (43.1) 194:350 (55.4) (%) Median (months) 24.11 18.96 Hazard ratio (95% CI) b 0.76 (0.61, 0.94) a Aggregate subgroups were derived from ctDNA and tissue-based groupings. b The analysis was performed using a Cox proportional hazards model including terms for treatment group, the subgroup factor, and a treatment by subgroup interaction. Confidence interval calculated using the profile likelihood method. An HR < 1 favors olaparib 300 mg bd. Figure 17 PROpel: Kaplan-Meier plot of rPFS (investigator assessed) (50% Olaparib 300 mg bd + Abiraterone 1000 mg qd (N=399) Placebo bd + Abiraterone 1000 mg qd (N=397) Probability of Radiographic Progression-free Survival Time from randomisation (Months) Number of patients at risk: Olaparib 300 mg bd + Abiraterone 1000 mg qd maturity) DCO 30 July 2021 Figure 18 PROpel: Kaplan-Meier plot of OS (48% maturity) DCO 12 October 2022 Olaparib 300 mg bd + Abiraterone 1000 mg qd (N=399) Probability of Overall Survival Placebo bd + Abiraterone 1000 mg qd (N=397) Time from randomisation (Months) Number of patients at risk: Olaparib 300 mg bd + Abiraterone 1000 mg qd Placebo bd + Abiraterone 1000 mg qd Figure 19 PROpel: Forest plot of subgroup analysis of rPFS (investigator assessed) (50% maturity) DCO 30 July 2021 Hazard Ratio for Abiraterone Abiraterone Progression or Death + Olaparib + Placebo (95% CI) Number of events / Number of patients (%) All patients Age at random assignment: <65yr Age at random assignment: ≥65yr ECOG performance status at baseline = 0* ECOG performance status at baseline = 1* Metastasis: Bone only Metastasis: Visceral Metastasis: Other Docetaxel treatment at mHSPC stage No docetaxel treatment at mHSPC stage Baseline PSA: Below median baseline PSA* Baseline PSA: Above or equal to median baseline PSA* HRRm status (aggregate): HRRm HRRm status (aggregate): non-HRRm Asia region Europe region North and South America region White race Black/African American race Asian race Other race Abiraterone + Olaparib Better Abiraterone + Placebo Better Each subgroup analysis was performed using a Cox proportional hazards model that contained a term for treatment, factor, and treatment by factor interaction. A hazard ratio < 1 implies a lower risk of progression on olaparib. The size of a circle is proportional to the number of events. All subgroups in this figure are based upon data from the eCRF. *Excludes patients with no baseline assessment. CI: confidence interval, ECOG: Eastern Cooperative Oncology Group; HRRm: homologous recombination repair gene mutation; mHSPC: metastatic hormone-sensitive prostate cancer; NC: noncalculable; PSA: prostate-specific antigen.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties The pharmacokinetics of olaparib at the 300 mg tablet dose are characterised by an apparent plasma clearance of ~7 L/h, an apparent volume of distribution of ~158 L and a terminal half-life of 15 hours. On multiple dosing, an AUC accumulation ratio of 1.8 was observed and PK appeared to be time-dependent to a small extent. Absorption Following oral administration of olaparib via the tablet formulation (2 x 150 mg), absorption is rapid with median peak plasma concentrations typically achieved 1.5 hours after dosing. Co-administration with food slowed the rate (tmax delayed by 2.5 hours and Cmax reduced by approximately 21%) but did not significantly affect the extent of absorption of olaparib (AUC increased 8%). Consequently, Lynparza may be taken without regard to food (see section 4.2). Distribution The in vitro plasma protein binding is approximately 82% at 10 μg/mL which is approximately Cmax. In vitro, human plasma protein binding of olaparib was dose- dependent; the fraction bound was approximately 91% at 1 μg/mL, reducing to 82% at 10 μg/mL and to 70% at 40 μg/mL. In solutions of purified proteins, the olaparib fraction bound to albumin was approximately 56%, which was independent of olaparib concentrations. Using the same assay, the fraction bound to alpha-1 acid glycoprotein was 29% at 10 μg/mL with a trend of decreased binding at higher concentrations. Biotransformation In vitro, CYP3A4/5 were shown to be the enzymes primarily responsible for the metabolism of olaparib (see section 4.5). Following oral dosing of 14C-olaparib to female patients, unchanged olaparib accounted for the majority of the circulating radioactivity in plasma (70%) and was the major component found in both urine and faeces (15% and 6% of the dose respectively). The metabolism of olaparib is extensive. The majority of the metabolism was attributable to oxidation reactions with a number of the components produced undergoing subsequent glucuronide or sulfate conjugation. Up to 20, 37 and 20 metabolites were detected in plasma, urine and faeces respectively, the majority of them representing < 1% of the dosed material. A ring-opened piperazin-3- ol moiety, and two mono-oxygenated metabolites (each ~10%) were the major circulating components, with one of the mono-oxygenated metabolites also being the major metabolite in the excreta (6% and 5% of the urinary and faecal radioactivity respectively). In vitro, olaparib produced little/no inhibition of UGT1A4, UGT1A9, UGT2B7, or CYPs 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6 or 2E1 and is not expected to be a clinically significant time dependent inhibitor of any of these CYP enzymes. Olaparib inhibited UGT1A1 in vitro, however, PBPK simulations suggest this is not of clinical importance. In vitro, olaparib is a substrate of the efflux transporter P-gp, however, this is unlikely to be of clinical significance (see section 4.5). In vitro, data also show that olaparib is not a substrate for OATP1B1, OATP1B3, OCT1, BCRP or MRP2 and is not an inhibitor of OATP1B3, OAT1 or MRP2. Elimination Following a single dose of 14C-olaparib, ~86% of the dosed radioactivity was recovered within a 7-day collection period, ~44% via the urine and ~42% via the faeces. Majority of the material was excreted as metabolites. Special populations In population based PK analyses, patient age, gender, bodyweight, tumour location or race (including White and Japanese patients) were not significant covariates. Renal impairment In patients with mild renal impairment (creatinine clearance 51 to 80 ml/min), AUC increased by 24% and Cmax by 15% compared with patients with normal renal function. No Lynparza dose adjustment is required for patients with mild renal impairment. In patients with moderate renal impairment (creatinine clearance 31 to 50 ml/min), AUC increased by 44% and Cmax by 26% compared with patients with normal renal function. Lynparza dose adjustment is recommended for patients with moderate renal impairment (see section 4.2). There are no data in patients with severe renal impairment or end-stage renal disease (creatinine clearance < 30 ml/min). Hepatic impairment In patients with mild hepatic impairment (Child-Pugh classification A), AUC increased by 15% and Cmax by 13% and in patients with moderate hepatic impairment (Child- Pugh classification B), AUC increased by 8% and Cmax decreased by 13% compared with patients with normal hepatic function. No Lynparza dose adjustment is required for patients with mild or moderate hepatic impairment (see section 4.2). There are no data in patients with severe hepatic impairment (Child-Pugh classification C). Paediatric population No studies have been conducted to investigate the pharmacokinetics of olaparib in paediatric patients.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. טיפול אחזקה בחולה בגירה הסובלת מסרטן מתקדם מסוג שחלה אפיתליאלי או סרטן חצוצרות או סרטן פריטוניאלי ראשוני מסוג BRCA mutated, לאחר השגת תגובה מלאה או חלקית לכימותרפיה מבוססת פלטינום בקו הטיפול הראשון.2. בשילוב עם Bevacizumab, כטיפול אחזקה בחולה בגירה הסובלת מסרטן מתקדם מסוג שחלה אפיתליאלי או סרטן חצוצרות או סרטן פריטוניאלי ראשוני מסוג HRD+ (homologous recombination deficiency (HRD) positive status) ללא מוטציה ב-BRCA, לאחר השגת תגובה מלאה או חלקית לכימותרפיה מבוססת פלטינום בקו הטיפול הראשון. משך הטיפול בתכשיר להתוויה זו לא יעלה על שנתיים.3. מונותרפיה כטיפול אחזקה בחולה בגירה הסובלת מסרטן שחלה (כולל חצוצרות או פריטוניאלי ראשוני) חוזר רגיש לפלטינום מסוג BRCA (breast cancer susceptibility gene) mutated בחולות עם מוטציה מסוג germline או מוטציה סומטית של הגידול.4. טיפול בסרטן שד מוקדם בחולה עם מוטציה מולדת מסוג BRCA, שהינו HER2 שלילי, המצוי בסיכון גבוה.לעניין זה יוגדר סיכון גבוה כאחד מאלה:א. חולה שקיבלו טיפול ניאו אדג'ובנטי:1. Triple negative - כל חולה עם שארית מחלה (non pCR)2. HR positive - חולה עם שארית מחלה ומדד CPS + EG בערך 3 ומעלה ב. חולה שקיבל טיפול משלים:1. Triple negative - גידול ≥ 2 ס"מ (pT2<) או בלוטות לימפה מעורבות (pN1<)2. HR positive – לפחות ארבע בלוטות לימפה מעורבותהטיפול יינתן כטיפול משלים, לאחר טיפול כימותרפי שניתן כטיפול ניאו אדג'ובנטי או כטיפול משלים לאחר ניתוח.משך הטיפול בתכשיר להתוויה זו לא יעלה על שנה.במסגרת הטיפול המשלים יהיה החולה זכאי לטיפול באחד מאלה – Olaparib או Pembrolizumab. 5. טיפול בסרטן שד גרורתי בחולה עם מוטציה מסוג germline BRCA שלא מבטא HER2, ושטרם קיבל טיפול כימותרפי למחלתו הגרורתית. ב. מתן התרופה ייעשה לפי מרשם של רופא מומחה באונקולוגיה או רופא מומחה בגינקולוגיה המטפל באונקולוגיה גינקולוגית.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| מונותרפיה כטיפול אחזקה בחולה בגירה הסובלת מסרטן שחלה (כולל חצוצרות או פריטוניאלי ראשוני) חוזר רגיש לפלטינום מסוג BRCA (breast cancer susceptibility gene) mutated בחולות עם מוטציה מסוג germline או מוטציה סומטית של הגידול | 12/01/2017 | אונקולוגיה | ovarian cancer, סרטן שחלה | |
| מונותרפיה כטיפול אחזקה בחולה בגירה הסובלת מסרטן שחלה (כולל חצוצרות או פריטוניאלי ראשוני) חוזר רגיש לפלטינום מסוג BRCA (breast cancer susceptibility gene) mutated בחולות עם מוטציה מסוג germline | 21/01/2016 | אונקולוגיה | ovarian cancer, סרטן שחלה | |
| טיפול בסרטן שד גרורתי בחולה עם מוטציה מסוג germline BRCA שלא מבטא HER2, ושטרם קיבל טיפול כימותרפי למחלתו הגרורתית | 30/01/2020 | אונקולוגיה | Breast cancer, סרטן שד | |
| טיפול בסרטן שד מוקדם בחולה עם מוטציה מולדת מסוג BRCA, שהינו HER2 שלילי, המצוי בסיכון גבוה. לעניין זה יוגדר סיכון גבוה כאחד מאלה: א. חולה שקיבלו טיפול ניאו אדג'ובנטי: 1. Triple negative - כל חולה עם שארית מחלה (non pCR) 2. HR positive - חולה עם שארית מחלה ומדד CPS + EG בערך 3 ומעלה ב. חולה שקיבל טיפול משלים: 1. Triple negative - גידול ≥ 2 ס"מ (pT2 | 01/02/2023 | אונקולוגיה | סרטן שד, Breast cancer | |
| טיפול אחזקה בחולה בגירה הסובלת מסרטן מתקדם מסוג שחלה אפיתליאלי או סרטן חצוצרות או סרטן פריטוניאלי ראשוני מסוג BRCA mutated, לאחר השגת תגובה מלאה או חלקית לכימותרפיה מבוססת פלטינום בקו הטיפול הראשון | 30/01/2020 | אונקולוגיה | ovarian cancer, סרטן שחלה | |
| בשילוב עם Bevacizumab, כטיפול אחזקה בחולה בגירה הסובלת מסרטן מתקדם מסוג שחלה אפיתליאלי או סרטן חצוצרות או סרטן פריטוניאלי ראשוני מסוג HRD+ (homologous recombination deficiency (HRD) positive status) ללא מוטציה ב-BRCA, לאחר השגת תגובה מלאה או חלקית לכימותרפיה מבוססת פלטינום בקו הטיפול הראשון. משך הטיפול בתכשיר להתוויה זו לא יעלה על שנתיים. | 01/03/2021 | אונקולוגיה | Ovarian cancer, סרטן שחלה |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
21/01/2016
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
ATC
מידע נוסף
עלון מידע לצרכן
11.04.21 - עלון לצרכן אנגלית 31.08.21 - עלון לצרכן אנגלית 10.08.22 - עלון לצרכן אנגלית 01.03.22 - עלון לצרכן עברית 30.08.22 - עלון לצרכן עברית 11.04.21 - עלון לצרכן ערבית 31.08.21 - עלון לצרכן ערבית 10.08.22 - עלון לצרכן ערבית 03.10.22 - עלון לצרכן עברית 06.12.22 - עלון לצרכן אנגלית 06.12.22 - עלון לצרכן עברית 06.12.22 - עלון לצרכן ערבית 15.08.23 - עלון לצרכן עברית 28.08.23 - עלון לצרכן עברית 25.10.23 - עלון לצרכן עברית 24.11.23 - עלון לצרכן עברית 07.02.24 - עלון לצרכן אנגלית 07.02.24 - עלון לצרכן ערבית 18.12.19 - החמרה לעלון 21.09.20 - החמרה לעלון 03.12.20 - החמרה לעלון 16.06.21 - החמרה לעלון 08.06.22 - החמרה לעלון 30.08.22 - החמרה לעלון 15.08.23 - החמרה לעלוןלתרופה במאגר משרד הבריאות
לינפארזה 100 מ"ג