Quest for the right Drug
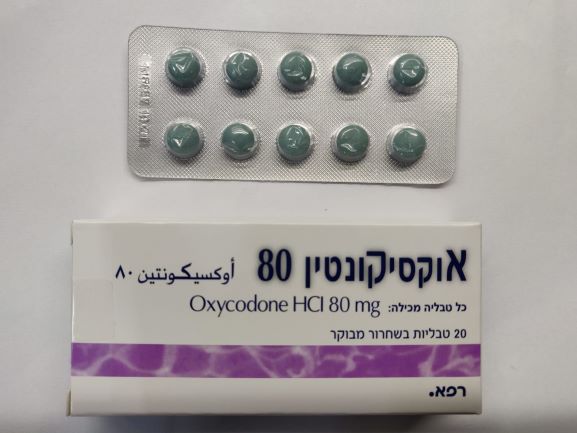
אוקסיקונטין 80 OXYCONTIN 80 (OXYCODONE HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות בשחרור מבוקר : TABLETS CONTROLLED RELEASE
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Caution must be exercised when administering oxycodone to the debilitated elderly, patients with severely impaired pulmonary function, patients with impaired hepatic or renal function, patients with myxoedema, hypothyroidism, Addison's disease, toxic psychosis, prostate hypertrophy, adrenocortical insufficiency, alcoholism, delirium tremens, diseases of the biliary tract, pancreatitis, inflammatory bowel disorders, hypotension, hypovolaemia, raised intracranial pressure, intracranial lesions, head injury (due to risk of increased intracranial pressure), reduced level of consciousness of uncertain origin, sleep apnoea or patients taking benzodiazepines, other CNS depressants (including alcohol) or MAO inhibitors (see section 4.5). The primary risk of opioid excess is respiratory depression. Sleep related breathing disorders Opioids can cause sleep-related breathing disorders including central sleep apnoea (CSA) and sleep-related hypoxemia. In patients who present with CSA, consider decreasing the total opioid dosage. Opioid use increases the risk of CSA in a dose-dependent fashion. Opioids may also cause worsening of pre-existing central sleep apnoea (see section 4.8). Concomitant use of oxycodone and sedative medicines such as benzodiazepines or related drugs may result in sedation, respiratory depression, coma and death. Because of these risks, concomitant prescribing with these sedative medicines should be reserved for patients for whom alternative treatment options are not possible. If a decision is made to prescribe oxycodone concomitantly with sedative medicines, the lowest effective dose should be used, and the duration of treatment should be as short as possible (see also general dose recommendation in section 4.2). The patient should be followed closely for signs and symptoms of respiratory depression and sedation. In this respect, it is strongly recommended to inform patients and their caregivers to be aware of these symptoms (see section 4.5). OxyContin tablets must be administered with caution in patients taking MAOIs or who have received MAOIs within the previous two weeks. OxyContin tablets should not be used where there is a possibility of paralytic ileus occurring. Should paralytic ileus be suspected or occur during use, OxyContin tablets should be discontinued immediately. OxyContin tablets are not recommended for pre-operative use or within the first 12-24 hours post- operatively. As with all opioid preparations, oxycodone products should be used with caution following abdominal surgery as opioids are known to impair intestinal motility and should not be used until the physician is assured of normal bowel function. Patients about to undergo additional pain relieving procedures (e.g. surgery, plexus blockade) should not receive OxyContin tablets for 12 hours prior to the intervention. If further treatment with OxyContin tablets is indicated, then the dosage should be adjusted to the new post-operative requirement. OxyContin 80 mg should not be used in patients not previously exposed to opioids. This tablet strength may cause fatal respiratory depression when administered to opioid naïve patients. For appropriate patients who suffer with chronic non-malignant pain, opioids should be used as part of a comprehensive treatment programme involving other medications and treatment modalities. A crucial part of the assessment of a patient with chronic non-malignant pain is the patient’s addiction and substance abuse history. If opioid treatment is considered appropriate for the patient, then the main aim of treatment is not to minimise the dose of opioid, but rather to achieve a dose which provides adequate pain relief with a minimum of side effects. Tolerance, Dependence and Opioid Use Disorder Tolerance and physical and/or psychological dependence may develop upon repeated administration of opioids such as oxycodone. Repeated use of OxyContin tablets may lead to Opioid Use Disorder (OUD). A higher dose and longer duration of opioid treatment can increase the risk of developing OUD. Abuse or intentional misuse of OxyContin tablets may result in overdose and/or death. The risk of developing OUD is increased in patients with a personal or a family history (parents or siblings) of substance use disorders (including alcohol use disorder), in current tobacco users or in patients with a personal history of other mental health disorders (e.g. major depression, anxiety and personality disorders). Before initiating treatment with OxyContin tablets and during the treatment, treatment goals and a discontinuation plan should be agreed with the patient. Before and during treatment the patient should also be informed about the risks and signs of OUD. If these signs occur, patients should be advised to contact their physician. Patients will require monitoring for signs of drug-seeking behaviour (e.g. too early requests for refills). The prescriber should conduct a review of concomitant opioids and psycho-active drugs (like benzodiazepines). For patients with signs and symptoms of OUD, consultation with an addiction specialist should be considered. A comprehensive patient history should be taken to document concomitant medications, including over-the-counter medicines and medicines obtained on-line, and past and present medical and psychiatric conditions. Patients may find that treatment is less effective with chronic use and express a need to increase the dose to obtain the same level of pain control as initially experienced. Patients may also supplement their treatment with additional pain relievers. These could be signs that the patient is developing tolerance. The risks of developing tolerance should be explained to the patient. Overuse or misuse may result in overdose and/or death. It is important that patients only use medicines that are prescribed for them at the dose they have been prescribed and do not give this medicine to anyone else. Patients should be closely monitored for signs of misuse, abuse or addiction. The clinical need for analgesic treatment should be reviewed regularly. Drug withdrawal syndrome Prior to starting treatment with any opioids, a discussion should be held with patients to put in place a withdrawal strategy for ending treatment with oxycodone. Drug withdrawal syndrome may occur upon abrupt cessation of therapy or dose reduction. When a patient no longer requires therapy, it is advisable to taper the dose gradually to minimise symptoms of withdrawal. Tapering from a high dose may take weeks to months. The opioid drug withdrawal syndrome is characterised by some or all of the following: restlessness, lacrimation, rhinorrhoea, yawning, perspiration, chills, myalgia, mydriasis and palpitations. Other symptoms may also develop including irritability, agitation, anxiety, hyperkinesia, tremor, weakness, insomnia, anorexia, abdominal cramps, nausea, vomiting, diarrhoea, increased blood pressure, increased respiratory rate or heart rate. If women take this drug during pregnancy there is a risk that their newborn infants will experience neonatal withdrawal syndrome. Hyperalgesia Hyperalgesia may be diagnosed if the patient on long-term opioid therapy presents with increased pain. This might be qualitatively and anatomically distinct from pain related to disease progression or to breakthrough pain resulting from development of opioid tolerance. Pain associated with hyperalgesia tends to be more diffuse than the pre-existing pain and less defined in quality. Symptoms of hyperalgesia may resolve with a reduction of opioid dose. Hepatobiliary disorders Oxycodone may cause dysfunction and spasm of the Sphincter of Oddi, thus raising intrabiliary pressure and increasing the risk of biliary tract symptoms and pancreatitis. Therefore, oxycodone has to be administered with caution in patients with pancreatitis and diseases of the biliary tract. OxyContin tablets must be swallowed whole, and not broken, chewed or crushed. The administration of broken, chewed or crushed OxyContin tablets leads to a rapid release and absorption of a potentially fatal dose of oxycodone (see Section 4.9). OxyContin 10, 20, 40, 80: There have been post-marketing reports of difficulty in swallowing OxyContin tablets. These reports included choking, gagging, regurgitation and tablets stuck in the throat. Instruct patients not to pre-soak, lick or otherwise wet OxyContin tablets prior to placing in the mouth, and to take one tablet at a time with enough water to ensure complete swallowing immediately after placing in the mouth. There have been rare post-marketing reports of cases of intestinal obstruction, and exacerbation of diverticulitis, some of which have required medical intervention to remove the tablet. Patients with underlying GI disorders such as esophageal cancer or colon cancer with a small gastrointestinal lumen are at greater risk of developing these complications. Consider use of an alternative analgesic in patients who have difficulty swallowing and patients at risk for underlying GI disorders resulting in a small gastrointestinal lumen. Concomitant use of alcohol and OxyContin may increase the undesirable effects of OxyContin; concomitant use should be avoided. Abuse of oral dosage forms by parenteral administration can be expected to result in serious adverse events, such as local tissue necrosis, infection, pulmonary granulomas, increased risk of endocarditis, and valvular heart injury, which may be fatal. Empty matrix (tablets) may be seen in the stools. Opioids such as oxycodone hydrochloride may influence the hypothalamic-pituitary-adrenal or - gonadal axes. Some changes that can be seen include an increase in serum prolactin, and decreases in plasma cortisol and testosterone. Clinical symptoms may manifest from these hormonal changes.
Effects on Driving
4.7 Effects on ability to drive and use machines Oxycodone may impair the ability to drive and use machines. Oxycodone may modify patients' reactions to a varying extent depending on the dosage and individual susceptibility. Therefore, patients should not drive or operate machinery if affected. This medicine can impair cognitive function and can affect a patient's ability to drive safely. When prescribing this medicine, patients should be told: • The medicine is likely to affect your ability to drive. • Do not drive until you know how the medicine affects you.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/2000
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
14.02.13 - עלון לצרכן 06.08.15 - עלון לצרכן אנגלית 01.08.21 - עלון לצרכן אנגלית 01.08.21 - עלון לצרכן עברית 01.08.21 - עלון לצרכן ערבית 02.11.22 - עלון לצרכן עברית 11.05.23 - עלון לצרכן אנגלית 11.05.23 - עלון לצרכן עברית 11.05.23 - עלון לצרכן ערבית 01.08.23 - עלון לצרכן אנגלית 01.08.23 - עלון לצרכן עברית 01.08.23 - עלון לצרכן ערבית 03.06.24 - עלון לצרכן עברית 05.09.24 - עלון לצרכן עברית 05.03.19 - החמרה לעלון 12.04.21 - החמרה לעלון 27.05.13 - החמרה לעלון 02.11.22 - החמרה לעלון 05.12.22 - החמרה לעלון 07.09.23 - החמרה לעלון 06.06.24 - החמרה לעלון 05.09.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
אוקסיקונטין 80