Quest for the right Drug
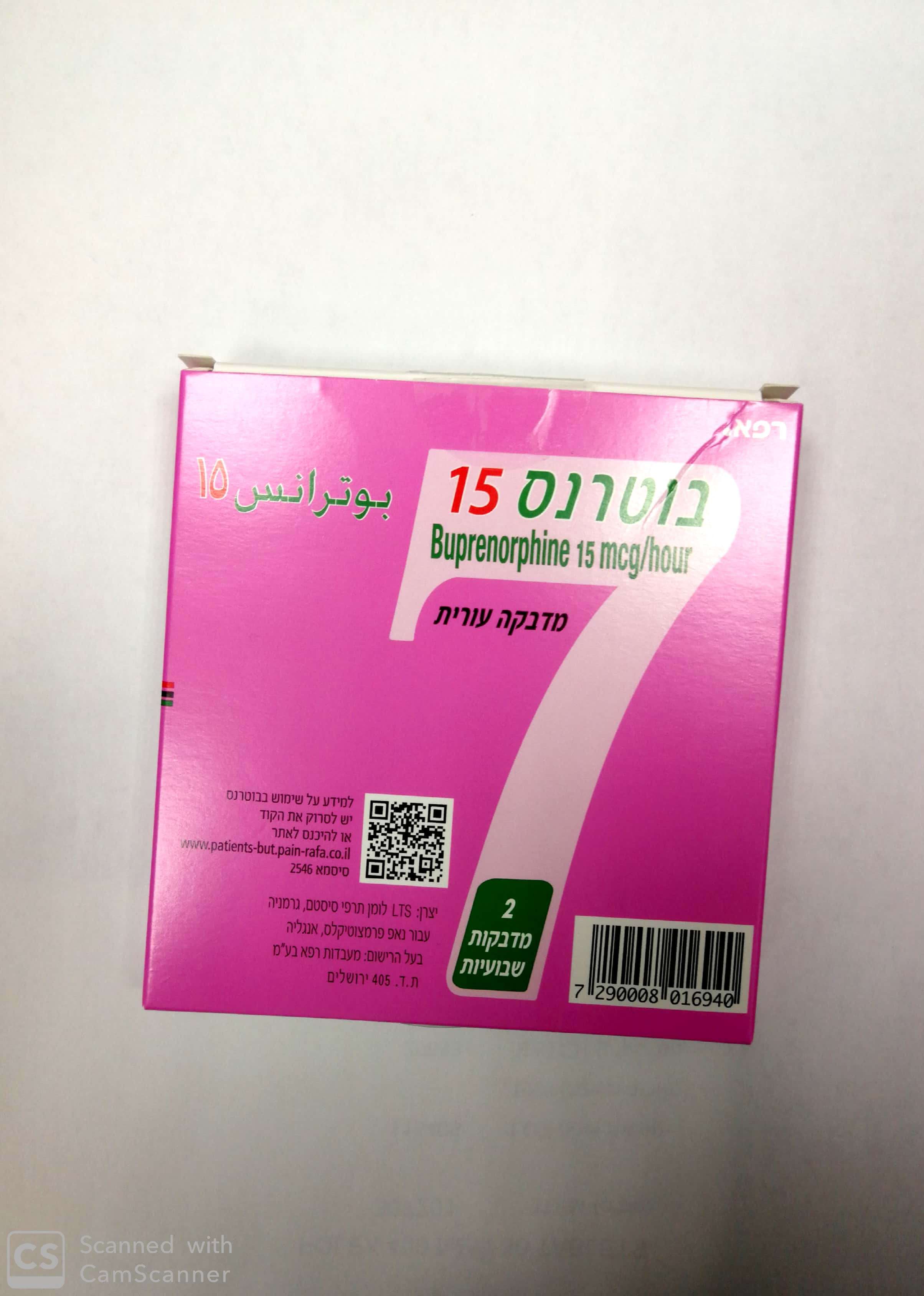
בוטרנס 15 BUTRANS 15 (BUPRENORPHINE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
בין-עורי : TRANSDERMAL
צורת מינון:
מדבקות במבנה מטריצה : PATCHES MATRIX
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4. Special warnings and precautions for use BuTrans should be used with particular caution in patients with severely impaired respiratory function, sleep apnoea, acute alcohol intoxication, head injury, shock, a reduced level of consciousness of uncertain origin, intracranial lesions or increased intracranial pressure, severe hepatic impairment (see section 4.2) or constipation. The primary risk of opioid excess is respiratory depression. Sleep-related breathing disorders Opioids can cause sleep-related breathing disorders including central sleep apnoea (CSA) and sleep-related hypoxemia. Opioid use increases the risk of CSA in a dose-dependent fashion. In patients who present with CSA, consider decreasing the total opioid dosage. Concomitant use of BuTrans and sedative medicines such as benzodiazepines or related drugs may result in sedation, respiratory depression, coma and death. Because of these risks, concomitant prescribing with these sedative medicines should be reserved for patients for whom alternative treatment options are not possible. If a decision is made to prescribe BuTrans concomitantly with sedative medicines, the lowest effective dose should be used, and the duration of treatment should be as short as possible. The patients should be followed closely for signs and symptoms of respiratory depression and sedation. In this respect, it is strongly recommended to inform patients and their caregivers to be aware of these symptoms (see section 4.5). Significant respiratory depression has been associated with buprenorphine, particularly by the intravenous route. A number of overdose deaths have occurred when addicts have intravenously abused buprenorphine, usually with benzodiazepines concomitantly. Additional overdose deaths due to ethanol and benzodiazepines in combination with buprenorphine have been reported. Serotonin syndrome Concomitant administration of BuTrans and other serotonergic agents, such as selective serotonin re-uptake inhibitors (SSRIs), serotonin norepinephrine re-uptake inhibitors (SNRIs) or tricyclic antidepressants may result in serotonin syndrome, a potentially life-threatening condition (see section 4.5). If concomitant treatment with other serotonergic agents is clinically warranted, careful observation of the patient is advised, particularly during treatment initiation and dose increases. Symptoms of serotonin syndrome may include mental-status changes, autonomic instability, neuromuscular abnormalities, and/or gastrointestinal symptoms. If serotonin syndrome is suspected, a dose reduction or discontinuation of therapy should be considered depending on the severity of the symptoms. Skin reactions at application site Application site reactions usually present as a mild to moderate skin inflammation (contact dermatitis) with erythema, oedema, pruritis, rash, vesicles and pain or a burning sensation at the application site. The reaction typically resolves spontaneously following removal of the BuTrans patch. Adherence to the method of administration given in section 4.2 reduces the risk of skin reactions at the application site. BuTrans patches may also cause skin sensitisation and subsequent immune-mediated, type IV hypersensitivity reaction allergic contact dermatitis. Allergic contact dermatitis may develop with a significant delay of up to several months following initiation of treatment with BuTrans patches. This may manifest either with symptoms similar to irritant contact dermatitis or with more severe symptoms, including burn-like lesions with bullae and discharge which spread beyond the application site and may not resolve rapidly following removal of the patch. Patients and caregivers should be instructed to monitor the application site for such reactions. If allergic contact dermatitis is suspected, relevant diagnostic procedures should be performed to determine whether sensitisation has occurred and is caused by the patches. If allergic contact dermatitis is confirmed treatment should be discontinued (see section 4.3). Continued treatment with BuTrans patches in patients experiencing allergic contact dermatitis may lead to complications, including blistering of the skin, open wound, bleeding, ulceration and subsequent infections. Mechanical injuries during patch removal, such as laceration, are also possible in patients with fragile skin. Chronic inflammation may lead to long-lasting sequelae such as post-inflammatory hyper- and hypopigmentation, as well as dry and thick scaly lesions which may closely resemble scars. Buprenorphine may lower the seizure threshold in patients with a history of seizure disorder. Since CYP3A4 inhibitors may increase concentrations of buprenorphine (see section 4.5), patients already treated with CYP3A4 inhibitors should have their dose of BuTrans carefully titrated since a reduced dosage might be sufficient in these patients. BuTrans is not recommended for analgesia in the immediate post-operative period or in other situations characterised by a narrow therapeutic index or a rapidly varying analgesic requirement. Drug dependence, tolerance and potential for abuse For all patients, prolonged use of this product may lead to drug dependence (addiction), even at therapeutic doses. The risks are increased in individuals with current or past history of substance misuse disorder (including alcohol misuse) or mental health disorder (e.g., major depression). Additional support and monitoring may be necessary when prescribing for patients at risk of opioid misuse. A comprehensive patient history should be taken to document concomitant medications, including over-the- counter medicines and medicines obtained on-line, and past and present medical and psychiatric conditions. Patients may find that treatment is less effective with chronic use and express a need to increase the dose to obtain the same level of pain control as initially experienced. Patients may also supplement their treatment with additional pain relievers. These could be signs that the patient is developing tolerance. The risks of developing tolerance should be explained to the patient. Overuse or misuse may result in overdose and/or death. It is important that patients only use medicines that are prescribed for them at the dose they have been prescribed and do not give this medicine to anyone else. Patients should be closely monitored for signs of misuse, abuse, or addiction. The clinical need for analgesic treatment should be reviewed regularly. Drug withdrawal syndrome Prior to starting treatment with any opioids, a discussion should be held with patients to put in place a withdrawal strategy for ending treatment with buprenorphine. Drug withdrawal syndrome may occur upon abrupt cessation of therapy or dose reduction. When a patient no longer requires therapy, it is advisable to taper the dose gradually to minimise symptoms of withdrawal. Tapering from a high dose may take weeks to months. Withdrawal syndrome, when it occurs, is generally mild, begins after 2 days and may last up to 2 weeks. The opioid drug withdrawal syndrome is characterised by some or all of the following: restlessness, lacrimation, rhinorrhoea, yawning, perspiration, chills, myalgia, mydriasis and palpitations. Other symptoms may also develop including irritability, agitation, anxiety, hyperkinesia, tremor, weakness, insomnia, anorexia, abdominal cramps, nausea, vomiting, diarrhoea, increased blood pressure, increased respiratory rate or heart rate. If women take this drug during pregnancy, there is a risk that their newborn infants will experience neonatal withdrawal syndrome. Hyperalgesia Hyperalgesia may be diagnosed if the patient on long-term opioid therapy presents with increased pain. This might be qualitatively and anatomically distinct from pain related to disease progression or to breakthrough pain resulting from development of opioid tolerance. Pain associated with hyperalgesia tends to be more diffuse than the pre-existing pain and less defined in quality. Symptoms of hyperalgesia may resolve with a reduction of opioid dose. BuTrans should not be used at higher doses than recommended.
Effects on Driving

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/2000
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
