Quest for the right Drug
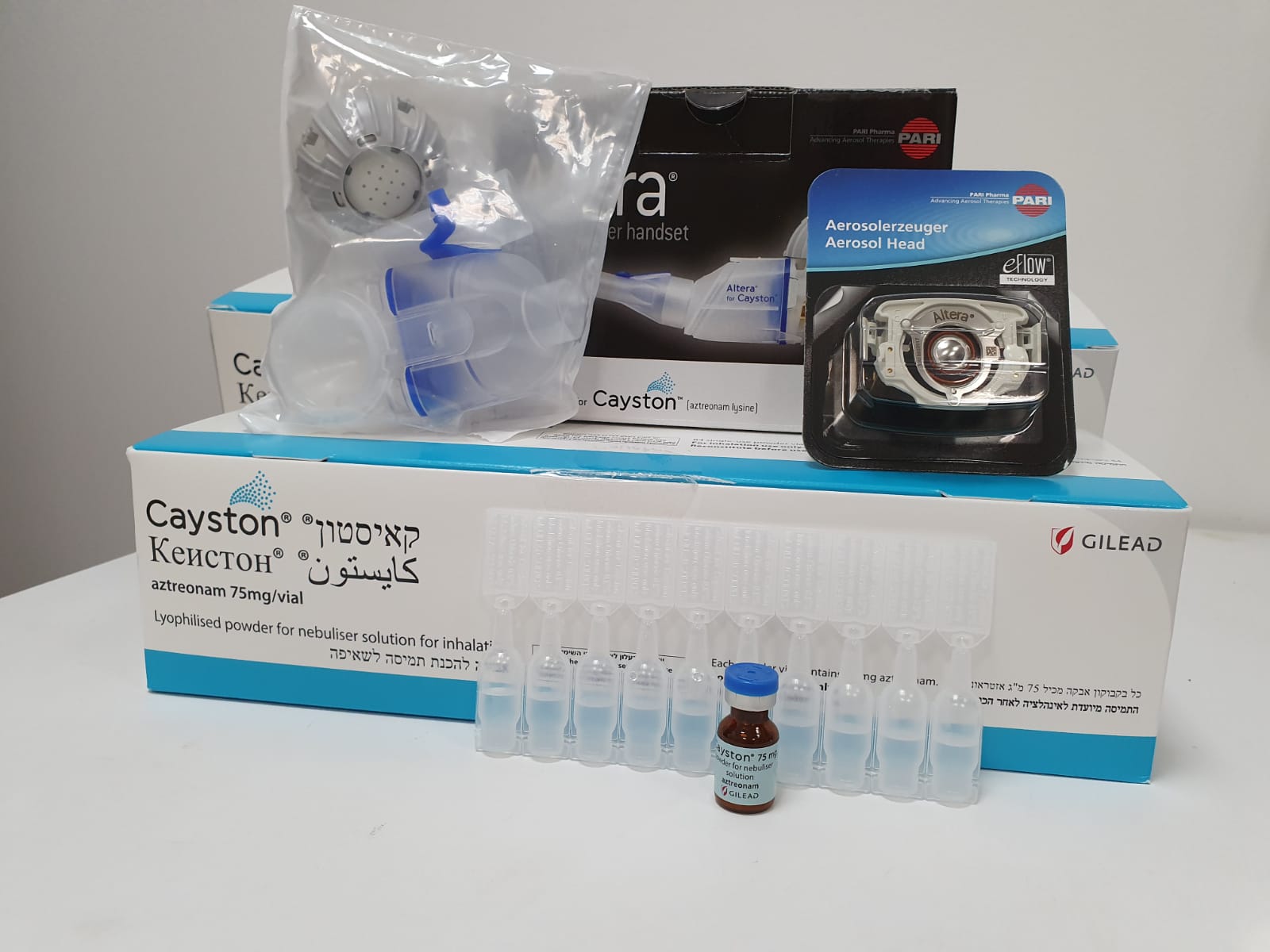
קאיסטון CAYSTON (AZTREONAM)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
שאיפה : INHALATION
צורת מינון:
אבקה מיובשת בהקפאה לתמיסת נבולייזר : LYOPHILIZED POWDER FOR NEBULISER SOLUTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antibacterials for systemic use, other beta-lactam antibacterials, ATC code: J01DF01 Mechanism of action Aztreonam exhibits activity in vitro against gram-negative aerobic pathogens, including P. aeruginosa. Aztreonam binds to penicillin-binding proteins of susceptible bacteria, which leads to inhibition of bacterial cell wall synthesis, followed by filamentation and cell lysis. Mechanisms of resistance Loss of susceptibility to aztreonam in CF patients with P. aeruginosa occurs either through selection of strains with mutations located on the chromosome or rarely through acquisition of plasmid/integron mediated genes. Known mechanisms of resistance to aztreonam mediated by mutation of chromosomal genes include: hyperexpression of the Class C beta-lactamase AmpC and up-regulation of the efflux pump MexAB-OprM. The known mechanism of resistance to aztreonam mediated by acquisition of genes involves acquisition of extended spectrum beta-lactam enzymes (ESBLs) that hydrolyse the four- member, nitrogen-containing ring of aztreonam. ESBLs from Class A, B and D beta-lactamases may have activity against aztreonam. Class A beta- lactamases reported to hydrolyse aztreonam include the VEB type (primarily Southeast Asia), PER type (Turkey), and GES and IBC types (France, Greece, and S. Africa). There are rare reports of organisms with metallo-beta-lactamases (MBLs), Class B, that are resistant to aztreonam, VIM-5 (K. pneumoniae and P. aeruginosa - Turkey), VIM-6 (P. putida - Singapore) and VIM-7 (P. aeruginosa - United States), however, it is possible that these organisms were expressing multiple resistance mechanisms and thus a MBL was not responsible for the observed resistance to aztreonam. There are rare reports of Class D beta-lactamases from clinical isolates of P. aeruginosa, OXA-11 (Turkey) and OXA-45 (United States) that hydrolyse aztreonam. Microbiology A single sputum sample from a CF patient may contain multiple isolates of P. aeruginosa and each isolate may have a different level of in vitro susceptibility to aztreonam. The in vitro antimicrobial susceptibility test methods used for parenteral aztreonam therapy can be used to monitor the susceptibility of P. aeruginosa isolated from CF patients. In the Phase 3 placebo-controlled studies of Cayston, local aztreonam concentrations generally exceeded aztreonam MIC values for P. aeruginosa, regardless of the level of P. aeruginosa susceptibility. Treatment with up to nine 28-day courses of 75 mg 3 times a day Cayston therapy resulted in clinically important improvements in respiratory symptoms, pulmonary function, and sputum P. aeruginosa CFU density; no increases in P. aeruginosa MIC50 (± 2 dilution change) were observed, whereas MIC90 increased intermittently to 4 times the initial MIC. In a 24-week active-controlled study of Cayston therapy, no increases in P. aeruginosa MIC50 (± 2 dilution change) were observed, whereas MIC90 increased to 4 times the initial MIC. At the end of the study, the percentage of patients with aztreonam MIC for P. aeruginosa above the parenteral breakpoint (> 8 µg/ml) increased from 34% at baseline to 49%, the percentage of patients with P. aeruginosa resistant to at least 1 beta- lactam antibiotic increased from 56% at baseline to 67%, and the percentage of patients with P. aeruginosa resistant to all 6 beta-lactam antibiotics tested increased from 13% at baseline to 18%. There is a risk that P. aeruginosa isolates may develop resistance to aztreonam or other beta-lactam antibiotics in patients treated with Cayston. The emergence of parenteral P. aeruginosa resistance to aztreonam and other beta-lactam antibiotics may have potential consequences for the treatment of acute pulmonary exacerbations with systemic antibiotics. However, similar improvements in lung function were seen after treatment with Cayston among patients with aztreonam susceptible or resistant P. aeruginosa isolates. In studies of up to nine 28-day courses of Cayston therapy, no increases of clinical significance were observed in the treatment-emergent isolation of other gram-negative bacterial respiratory pathogens (Burkholderia species, Stenotrophomonas maltophilia and Alcaligenes species). During the 6-month randomised phase of study GS-US-205-0110, treatment-emergent isolation of MSSA and MRSA was observed more commonly among aztreonam-treated patients than Tobramycin Nebuliser Solution (TNS)-treated patients. The majority of the treatment-emergent isolations were intermittent. Treatment-emergent persistent isolation (defined as absent at screening/baseline then present at 3 or more subsequent consecutive visits) of MSSA occurred in 6% of aztreonam-treated patients compared to 3% of TNS-treated patients. Treatment-emergent intermittent isolation of MRSA occurred in 7% of aztreonam-treated patients compared to 1% of TNS-treated patients and treatment-emergent persistent isolation of MRSA occurred in 3% of aztreonam-treated patients compared to no TNS-treated patients. An association between persistent isolation of MRSA and more severe disease and increased mortality has been reported in the literature. During clinical studies of Cayston, isolation of MRSA did not result in worsening of lung function. Clinical efficacy and safety Cayston was compared to TNS over three 28-day courses of treatment in a randomised, active- controlled, multicenter study (GS-US-205-0110). Patients participating in this study in Europe who completed at least 1 course of Cayston or TNS during the randomised phase could subsequently receive up to three 28-day courses of Cayston in an open-label extension phase. Entry criteria included CF, FEV1 ≤ 75% predicted, stable pulmonary disease, a recent positive sputum culture for P. aeruginosa, and previous treatment with aerosolised antibiotics without demonstration of drug intolerance. Cayston was evaluated over a period of 28-days of treatment (one course) in two randomised, double- blind, placebo-controlled, multicentre studies (CP-AI-005 and CP-AI-007). Patients participating in these studies could subsequently receive multiple courses of Cayston in an open-label follow-on study (CP-AI-006). Entry criteria included CF, baseline FEV1 between 25% and 75% predicted, and chronic P. aeruginosa lung infection. Overall, 539 patients (78% adults) were treated in these studies. Studies were conducted using the Altera Nebuliser System to administer Cayston. GS-US-205-0110 In GS-US-205-0110, 268 patients with CF and chronic P. aeruginosa lung infection were randomised and received Cayston (n = 136) or TNS (n = 132). Fifty-nine paediatric patients aged 6 to 17 years were included in the study. Patients were randomised in a 1:1 ratio to receive either aztreonam (75 mg) administered by inhalation 3 times a day or TNS (300 mg) administered 2 times a day. Treatments were administered for three cycles of 28 days on therapy followed by 28 days off therapy. The co-primary endpoints were non-inferiority of Cayston to TNS in relative change from baseline to Day 28 in FEV1 % predicted and superiority of Cayston to TNS in actual change from baseline in FEV1 % predicted across 3 treatment courses (the average of the actual change in FEV1 % predicted observed at the end of each treatment course). The adjusted mean percent change from baseline to Day 28 in FEV1 % predicted was 8.35 and 0.55 in the Cayston and TNS groups, respectively (treatment difference: 7.80; p = 0.0001; 95% CI: 3.86, 11.73). The adjusted mean actual change from baseline in FEV1 % predicted across 3 treatment courses was 2.05 and -0.66 in the Cayston and TNS groups, respectively (treatment difference: 2.70; p = 0.0023; 95% CI: 0.98, 4.43). Patients treated with aztreonam experienced a longer time to need for i.v. antipseudomonal antibiotics related to respiratory events compared to TNS-treated patients (p = 0.0025). The Kaplan-Meier estimates for this event rate at week 24 were 36% in aztreonam- treated patients and 54% in TNS-treated patients. Additionally, aztreonam-treated patients had fewer hospitalisations due to respiratory events (40 versus 58, p = 0.044) and fewer respiratory events requiring the use of i.v. or inhaled antipseudomonal antibiotics (84 versus 121, p = 0.004) than TNS- treated patients. Aztreonam-treated patients also demonstrated larger mean improvements in CFQ-R respiratory symptoms scores compared to TNS-treated patients across 3 treatment courses (6.30 versus 2.17, p = 0.019). In the limited subgroup of patients who received inhaled tobramycin for less than 84 days in the previous 12 months (n = 40), lung function improvements at Day 28 and across three 28-day treatment courses were numerically smaller among aztreonam-treated patients than TNS-treated patients. CP-AI-007 CP-AI-007 enrolled 164 adult (predominantly) and paediatric patients randomised in a 1:1 ratio comparing Cayston 75 mg (80 patients) or placebo (84 patients) administered 3 times a day for 28 days (one course). Patients were required to have been off antipseudomonal antibiotics for at least 28 days before treatment with study drug. Pulmonary function and respiratory symptoms significantly improved from baseline to Day 28 in patients treated with one course of Cayston. CP-AI-005 CP-AI-005 enrolled 246 adult (predominantly) and paediatric patients. All patients were treated with Tobramycin Nebuliser Solution (TNS) 300 mg, 2 times a day in the four weeks immediately prior to receiving Cayston or placebo either 2 or 3 times a day for 28 days. Patients continued on their baseline medications, including macrolide antibiotics. Patients were randomised in a 2:2:1:1 ratio to be treated with aztreonam 75 mg 2 or 3 times a day or volume-matched placebo 2 or 3 times a day for 28 days immediately following the 28-day lead-in course of open-label TNS. Aztreonam therapy resulted in significant improvements in pulmonary function and respiratory symptoms at Day 28 in the 66 patients treated with one course Cayston 75 mg 3 times a day. CP-AI-006 CP-AI-006 was an open-label follow-on study to CP-AI-005 and CP-AI-007 evaluating the safety of repeated exposure to aztreonam and the effect on disease-related endpoints over multiple 28-day courses. Patients received Cayston at the same frequency (2 or 3 times a day) as they took Cayston or placebo in the randomised studies. Patients continued on their baseline medications and whenever indicated additional antibiotics were used in the majority of patients to treat exacerbations. Each 28-day course of Cayston was followed by a 28-day off drug period. Over nine 28-day courses of therapy, measures of pulmonary function (FEV1), CFQ-R respiratory symptoms scores, and P. aeruginosa sputum density showed a trend to improvement while the patients were on treatment compared with off treatment. However, due to the uncontrolled nature of the study and concomitant medications no conclusion can be drawn on the sustainability of the observed short term benefit over subsequent courses of treatment. Paediatric population A total of 137 paediatric patients aged 6 to 17 years with chronic P. aeruginosa infection and FEV1 ≤ 75% predicted have received Cayston in Phase 2 and Phase 3 clinical studies. Paediatric patients had clinical improvements with aztreonam as determined by an increase in FEV1, improvement in CFQ-R respiratory symptoms scores and decline in P. aeruginosa sputum density. Cayston is indicated for use in paediatric patients aged 6 years and older with repeated cycles of 28 days on therapy followed by 28 days off Cayston therapy based on the above clinical experience.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption Sputum concentrations Individual patients’ sputum aztreonam concentrations exhibited considerable variability. For the combined Phase 3 placebo-controlled studies, ten minutes following a single dose of 75 mg inhaled aztreonam on Days 0, 14, and 28, the mean sputum concentrations in 195 patients with CF were 726 µg/g, 711 µg/g, and 715 µg/g, respectively, indicating no increased accumulation of aztreonam following repeated dosing. Plasma concentrations Individual patients’ plasma aztreonam concentrations exhibited considerable variability. One hour following a single dose of 75 mg inhaled aztreonam (at approximately peak plasma concentration), the mean plasma level in patients with CF was 0.59 µg/ml. Mean peak plasma levels at Days 0, 14, and 28 of a course with 75 mg inhaled aztreonam 3 times a day were 0.55 µg/ml, 0.67 µg/ml, and 0.65 µg/ml, respectively, indicating no systemic accumulation of aztreonam following 3 times a day dosing. In contrast, the serum concentration of aztreonam following administration of aztreonam for injection (500 mg) is approximately 54 µg/ml. The protein binding of aztreonam in plasma is approximately 77% at clinically relevant plasma concentrations. Metabolism Aztreonam is not extensively metabolised. The principal metabolite (SQ26,992) is inactive and is formed by opening of the beta-lactam ring due to hydrolysis. Recovery data indicate that about 10% of the dose is excreted as this metabolite. Elimination The elimination half-life of aztreonam from serum is approximately 2.1 hours for inhalation administration, similar to what has been reported for aztreonam for injection. Approximately 10% of the total inhaled aztreonam dose is excreted in the urine as unchanged drug, as compared to 60-65% following intravenous administration of aztreonam for injection. Systemically absorbed aztreonam is eliminated about equally by active tubular secretion and glomerular filtration. Pharmacokinetics in special populations Age and gender There was no clinically relevant effect of age or sex on the pharmacokinetics of aztreonam. Renal and hepatic impairment Pharmacokinetic studies have not been performed in patients with renal or hepatic impairment. Pharmacokinetic properties for aztreonam for injection Peak levels of aztreonam are achieved at about one hour after i.m. administration. After identical single i.m. or i.v. doses, the serum concentrations are comparable at 1 hour (1.5 hours from the start of i.v. infusion), with similar slopes of serum concentrations thereafter. The serum half-life of aztreonam averaged 1.7 hours in subjects with normal renal function, independent of the dose and route. In healthy subjects 60-70% of a single i.m. or i.v. dose was recovered in the urine by 8 hours, and urinary excretion was essentially complete by 12 hours. Paediatric population The Phase 2 and 3 placebo-controlled, registrational studies permitted comparison of plasma concentrations 1 hour post dose of Cayston by age (6 to 12 years, 13 to 17 years, and ≥ 18 years). Data from these studies revealed minimal differences in mean plasma aztreonam concentrations between age groups in patients receiving Cayston 3 times a day. Pooled sputum concentration data from the Phase 2 and 3 registrational studies revealed some evidence of lower mean sputum concentrations in patients aged 13 to 17 years following one dose of Cayston 3 times a day. However, all mean sputum concentration values were associated with relatively large standard deviations.

פרטי מסגרת הכללה בסל
1. התרופה האמורה תינתן לטיפול נגד פסאודומונס ארוגינוזה בחולי לייפת כיסתית, שמיצו את הטיפול ב-Tobramycin.2. התרופה האמורה לא תינתן במקביל לטיפול ב-Tobramycin באינהלציה, למעט בחולים עם תפקודי ריאה מתחת ל-40%.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| התרופה האמורה תינתן לטיפול נגד פסאודומונס ארוגינוזה בחולי לייפת כיסתית, שמיצו את הטיפול ב-Tobramycin. | 12/01/2014 |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
12/01/2014
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
