Quest for the right Drug
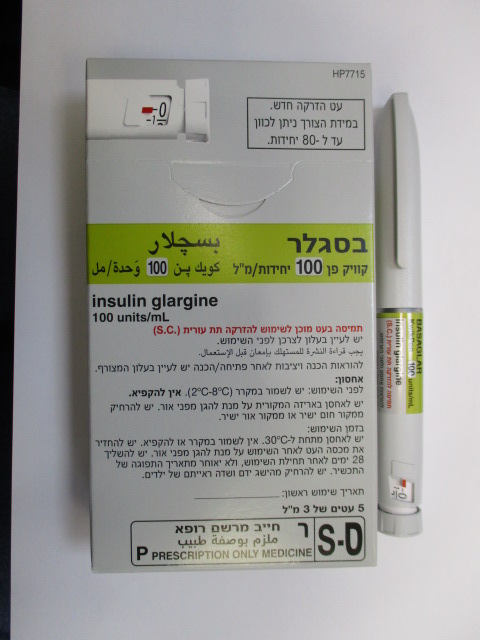
בסגלר BASAGLAR (INSULIN GLARGINE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תת-עורי : S.C
צורת מינון:
תמיסה להזרקה : SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Drugs used in diabetes. Insulins and analogues for injection, long- acting. ATC Code: A10AE04. Mechanism of action Insulin glargine is a human insulin analogue designed to have a low solubility at neutral pH. It is completely soluble at the acidic pH of the Basaglar injection solution (pH 4). After injection into the subcutaneous tissue, the acidic solution is neutralized, leading to formation of micro- precipitates from which small amounts of insulin glargine are continuously released, providing a smooth, peakless, predictable concentration/time profile with a prolonged duration of action. Insulin glargine is metabolized into 2 active metabolites M1 and M2 (see section 5.2). Insulin receptor binding: In vitro studies indicate that the affinity of insulin glargine and its metabolites M1 and M2 for the human insulin receptor is similar to the one of human insulin. IGF-1 receptor binding: The affinity of insulin glargine for the human IGF-1 receptor is approximately 5 to 8-fold greater than that of human insulin (but approximately 70 to 80-fold lower than the one of IGF-1), whereas M1 and M2 bind the IGF-1 receptor with slightly lower affinity compared to human insulin. The total therapeutic insulin concentration (insulin glargine and its metabolites) found in type 1 diabetic patients was markedly lower than what would be required for a half maximal occupation of the IGF-1 receptor and the subsequent activation of the mitogenic-proliferative pathway initiated by the IGF-1 receptor. Physiological concentrations of endogenous IGF-1 may activate the mitogenic-proliferative pathway; however, the therapeutic concentrations found in insulin therapy, including in Basaglar therapy, are considerably lower than the pharmacological concentrations required to activate the IGF-1 pathway. The primary activity of insulin, including insulin glargine, is regulation of glucose metabolism. Insulin and its analogues lower blood glucose levels by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production. Insulin inhibits lipolysis in the adipocyte, inhibits proteolysis and enhances protein synthesis. In clinical pharmacology studies, intravenous insulin glargine and human insulin have been shown to be equipotent when given at the same doses. As with all insulins, the time course of action of insulin glargine may be affected by physical activity and other variables. In euglycemic clamp studies in healthy subjects or in patients with type 1 diabetes, the onset of action of subcutaneous insulin glargine was slower than with human NPH insulin, its effect profile was smooth and peakless, and the duration of its effect was prolonged. The following graph shows the results from a study in patients: Figure 1: Activity profile in patients with type 1 diabetes ____ insulin glargine ------ NPH insulin Glucose Utilization Rate* (mg/kg/min) Time (h) after s.c injection End of observation period * Determined as amount of glucose infused to maintain constant plasma glucose levels (hourly mean values) The longer duration of action of subcutaneous insulin glargine is directly related to its slower rate of absorption and supports once daily administration. The time course of action of insulin and insulin analogues such as insulin glargine may vary considerably in different individuals or within the same individual. In a clinical study, symptoms of hypoglycemia or counter-regulatory hormone responses were similar after intravenous insulin glargine and human insulin both in healthy volunteers and patients with type 1 diabetes. In clinical studies, antibodies that cross-react with human insulin and insulin glargine were observed with the same frequency in both NPH-insulin and insulin glargine treatment groups. Effects of insulin glargine (once daily) on diabetic retinopathy were evaluated in an open-label 5- year NPH controlled study (NPH given bid) in 1,024 type 2 diabetic patients in which progression of retinopathy by 3 or more steps on the Early Treatment Diabetic Retinopathy Study (ETDRS) scale was investigated by fundus photography. No significant difference was seen in the progression of diabetic retinopathy when insulin glargine was compared to NPH insulin. The ORIGIN (Outcome Reduction with Initial Glargine INtervention) study was a multicenter, randomized, 2x2 factorial design study conducted in 12,537 participants at high cardiovascular (CV) risk with impaired fasting glucose (IFG) or impaired glucose tolerance (IGT) (12 % of participants) or type 2 diabetes mellitus treated with ≤1 antidiabetic oral agent (88 % of participants). Participants were randomized (1:1) to receive insulin glargine (n=6,264), titrated to reach FPG ≤95 mg/dL (5.3 mM), or standard care (n=6,273). The first co-primary efficacy outcome was the time to the first occurrence of CV death, nonfatal myocardial infarction (MI), or nonfatal stroke, and the second co-primary efficacy outcome was the time to the first occurrence of any of the first co-primary events, or revascularization procedure (coronary, carotid, or peripheral), or hospitalization for heart failure. Secondary endpoints included all-cause mortality and a composite microvascular outcome. Insulin glargine did not alter the relative risk for CV disease and CV mortality when compared to standard of care. There were no differences between insulin glargine and standard care for the two co-primary outcomes; for any component endpoint comprising these outcomes; for all-cause mortality; or for the composite microvascular outcome. Mean dose of insulin glargine by study end was 0.42 U/kg. At baseline, participants had a median HbA1c value of 6.4 % and median on-treatment HbA1c values ranged from 5.9 to 6.4% in the insulin glargine group, and 6.2 % to 6.6 % in the standard care group throughout the duration of follow-up. The rates of severe hypoglycemia (affected participants per 100 participant years of exposure) were 1.05 for insulin glargine and 0.30 for standard care group and the rates of confirmed non-severe hypoglycemia were 7.71 for insulin glargine and 2.44 for standard care group. Over the course of this 6-year study, 42 % of the insulin glargine group did not experience any hypoglycemia. At the last on-treatment visit, there was a mean increase in body weight from baseline of 1.4 kg in the insulin glargine group and a mean decrease of 0.8 kg in the standard care group. Pediatric population In a randomised, controlled clinical study, paediatric patients (age range 6 to 15 years) with type 1 diabetes (n = 349) were treated for 28 weeks with a basal-bolus insulin regimen where regular human insulin was used before each meal. Insulin glargine was administered once daily at bedtime and NPH human insulin was administered once or twice daily. Similar effects on glycohaemoglobin and the incidence of symptomatic hypoglycaemia were observed in both treatment groups; however, fasting plasma glucose decreased more from baseline in the insulin glargine group than in the NPH group. There was less severe hypoglycaemia in the insulin glargine group as well. One hundred forty three of the patients treated with insulin glargine in this study continued treatment with insulin glargine in an uncontrolled extension study with mean duration of follow-up of 2 years. No new safety signals were seen during this extended treatment with insulin glargine. A crossover study comparing insulin glargine plus lispro insulin to NPH plus regular human insulin (each treatment administered for 16 weeks in random order) in 26 adolescent type 1 diabetic patients aged 12 to 18 years was also performed. As in the paediatric study described above, fasting plasma glucose reduction from baseline was greater in the insulin glargine group than in the NPH group. HbA1c changes from baseline were similar between treatment groups; however, blood glucose values recorded overnight were significantly higher in the insulin glargine/ lispro group than the NPH/regular group, with a mean nadir of 5.4 mM vs 4.1 mM. Correspondingly, the incidences of nocturnal hypoglycaemia were 32 % in the insulin glargine / lispro group vs 52 % in the NPH / regular group. A 24-week parallel group study was conducted in 125 children with type 1 diabetes mellitus aged 2 to 6 years, comparing insulin glargine given once daily in the morning to NPH insulin given once or twice daily as basal insulin. Both groups received bolus insulin before meals. The primary aim of demonstrating non-inferiority of insulin glargine to NPH in all hypoglycaemia was not met and there was a trend to an increase of hypoglycemic events with insulin glargine [insulin glargine: NPH rate ratio (95% CI) = 1.18 (0.97-1.44)]. Glycohaemoglobin and glucose variabilities were comparable in both treatment groups. No new safety signals were observed in this study.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption In healthy subjects and diabetic patients, insulin serum concentrations indicated a slower and much more prolonged absorption and showed a lack of a peak after subcutaneous injection of insulin glargine in comparison to human NPH insulin. Concentrations were thus consistent with the time profile of the pharmacodynamic activity of insulin glargine. The graph above shows the activity profiles over time of insulin glargine and NPH insulin. Insulin glargine injected once daily will reach steady state levels in 2-4 days after the first dose. When given intravenously the elimination half-life of insulin glargine and human insulin were comparable. After subcutaneous injection of Basaglar in diabetic patients, insulin glargine is rapidly metabolized at the carboxyl terminus of the Beta chain with formation of two active metabolites M1 (21A-Gly-insulin) and M2 (21A-Gly-des-30B-Thr-insulin). In plasma, the principal circulating compound is the metabolite M1. The exposure to M1 increases with the administered dose of Basaglar. The pharmacokinetic and pharmacodynamic findings indicate that the effect of the subcutaneous injection with Basaglar is principally based on exposure to M1. Insulin glargine and the metabolite M2 were not detectable in the vast majority of subjects and, when they were detectable their concentration was independent of the administered dose of Basaglar. In clinical studies, subgroup analyses based on age and gender did not indicate any difference in safety and efficacy in insulin glargine-treated patients compared to the entire study population. Pediatric population Pharmacokinetics in children aged 2 to less than 6 years with type 1 diabetes mellitus was assessed in one clinical study (see section 5.1). Plasma “trough” levels of insulin glargine and its main M1 and M2 metabolites were measured in children treated with insulin glargine, revealing plasma concentration patterns similar to adults, and providing no evidence for accumulation of insulin glargine or its metabolites with chronic dosing.

פרטי מסגרת הכללה בסל
התרופה תינתן לחולי סוכרת
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| INSULIN GLARGINE | ||||
| INSULIN DETEMIR | ||||
| סכרת |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
15/04/2005
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לרופא
15.12.21 - עלון לרופאעלון מידע לצרכן
13.08.20 - עלון לצרכן אנגלית 13.08.20 - עלון לצרכן ערבית 21.12.21 - עלון לצרכן אנגלית 11.08.20 - עלון לצרכן עברית 21.12.21 - עלון לצרכן עברית 21.12.21 - עלון לצרכן ערבית 03.06.20 - החמרה לעלון 08.07.20 - החמרה לעלון 11.08.20 - החמרה לעלון 13.08.20 - החמרה לעלון 01.10.20 - החמרה לעלון 02.09.21 - החמרה לעלון 15.12.21 - החמרה לעלוןלתרופה במאגר משרד הבריאות
בסגלר