Quest for the right Drug
יסקרטה YESCARTA (AXICABTAGENE CILOLEUCEL)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אין פרטים : DISPERSION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
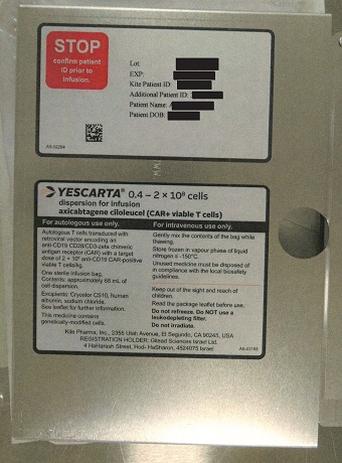
4.4 Special warnings and precautions for use Traceability The traceability requirements of cell-based advanced therapy medicinal products must apply. To ensure traceability the name of the product, the batch number and the name of the treated patient must be kept for a period of 30 years after expiry date of the medicinal product. Autologous use Yescarta is intended solely for autologous use and must not, under any circumstances, be administered to other patients. Before infusion, the patient’s identity must match the patient identifiers on the Yescarta infusion bag and cassette. Yescarta must not be administered if the information on the patient- specific infusion bag and cassette label does not match the patient’s identity. Reasons to delay treatment Due to the risks associated with Yescarta treatment, infusion must be delayed if a patient has any of the following conditions: • Unresolved serious adverse reactions (especially pulmonary reactions, cardiac reactions, or hypotension) including from preceding chemotherapies. • Active uncontrolled infection. • Active graft-versus-host disease (GVHD). Monitoring after infusion Patients must be monitored daily for the first 10 days following infusion for signs and symptoms of potential CRS, neurologic events and other toxicities. Physicians should consider hospitalisation for the first 10 days post infusion or at the first signs/symptoms of CRS and/or neurologic events. After the first 10 days following infusion, the patient is to be monitored at the physician’s discretion. Patients are to be counselled to remain within the proximity of a qualified treatment centre for at least 4 weeks following infusion and to seek immediate medical attention should signs or symptoms of CRS or neurological adverse reactions occur. Vital signs and organ function must be monitored depending on the severity of the reaction. Transmission of an infectious agent Although Yescarta is tested for sterility and mycoplasma, a risk of transmission of infectious agents exists. Healthcare professionals administering Yescarta must, therefore, monitor patients for signs and symptoms of infection after treatment and treat appropriately, if needed. Serological testing Screening for HBV, HCV, and HIV must be performed before collection of cells for manufacturing of Yescarta (see section 4.2). Blood, organ, tissue and cell donation Patients treated with Yescarta must not donate blood, organs, tissues, or cells for transplantation. Concomitant disease Patients with active CNS disorder or inadequate renal, hepatic, pulmonary, or cardiac function are likely to be more vulnerable to the consequences of the adverse reactions described below and require special attention. Primary central nervous system (CNS) lymphoma There is no experience of use of Yescarta in patients with primary CNS lymphoma. Therefore, the risk/benefit of Yescarta has not been established in this population. Yescarta is not indicated for the treatment of patients with primary or secondary central nervous system lymphoma. Cytokine release syndrome Nearly all patients experienced some degree of CRS. Severe CRS, including life-threatening and fatal reactions, was very commonly observed with Yescarta with a time to onset of 1 to 12 days in ZUMA-1 and ZUMA-7, and 1 to 11 days in ZUMA-5 (see section 4.8). CRS should be managed at the physician’s discretion, based on the patient’s clinical presentation and according to the CRS management algorithm provided in Table 1. Interleukin-6 (IL-6) receptor inhibitor based therapy such as tocilizumab has been administered for moderate or severe CRS associated with Yescarta. At least 1 dose of tocilizumab per patient must be on site and available for administration prior to Yescarta infusion. The treatment centre must have access to an additional dose of tocilizumab within 8 hours of each previous dose. Patients must be monitored daily for signs and symptoms of CRS for at least 10 days following infusion at the qualified clinical facility. After the first 10 days following infusion, the patient is to be monitored at the physician’s discretion. Patients are to be counselled to remain within proximity of a qualified clinical facility for at least 4 weeks following infusion and to seek immediate medical attention should signs or symptoms of CRS occur. Treatment algorithms have been developed to ameliorate some of the CRS symptoms experienced by patients on Yescarta. These include the use of tocilizumab or tocilizumab and corticosteroids for moderate, severe, or life-threatening CRS as summarised in Table 1. Patients who experience Grade 2 or higher CRS (e.g. hypotension, not responsive to fluids, or hypoxia requiring supplemental oxygenation) must be monitored with continuous cardiac telemetry and pulse oximetry. For patients experiencing severe CRS, consider performing an echocardiogram to assess cardiac function. For severe or life-threatening CRS, consider intensive-care supportive therapy. Yescarta must not be administered to patients with active infections or inflammatory disease until these conditions have resolved. CRS has been known to be associated with end organ dysfunction (e.g., hepatic, renal, cardiac, and pulmonary). In addition worsening of underlying organ pathologies can occur in the setting of CRS. Patients with medically significant cardiac dysfunction must be managed by standards of critical care and measures such as echocardiography are to be considered. Diagnosis of CRS requires excluding alternate causes of systemic inflammatory response, including infection. In the event of febrile neutropenia, infection is to be considered and managed with broad spectrum antibiotics, fluids, and other supportive care as medically indicated. Evaluation for haemophagocytic lymphohistiocytosis/macrophage activation syndrome (HLH/MAS) is to be considered in patients with severe or unresponsive CRS. Yescarta continues to expand and persist following administration of tocilizumab and corticosteroids. Tumour necrosis factor (TNF) antagonists are not recommended for management of Yescarta-associated CRS. Table 1: CRS grading and management guidance CRS Gradea Tocilizumab Corticosteroids Grade 1 If not improving after 24 hours, N/A Symptoms require manage as Grade 2. symptomatic treatment only (e.g., fever, nausea, fatigue, headache, myalgia, malaise). Grade 2 Administer tocilizumabc 8 mg/kg Manage per Grade 3 if no improvement Symptoms require and intravenously over 1 hour (not to within 24 hours after starting tocilizumab. respond to moderate exceed 800 mg). intervention. Repeat tocilizumab every 8 hours Oxygen requirement less than as needed if not responsive to 40% FiO2 or hypotension intravenous fluids or increasing responsive to fluids or low supplemental oxygen. dose of one vasopressor or Limit to a maximum of 3 doses in Grade 2 organ toxicityb. a 24 hour period; maximum total of 4 doses if no clinical improvement in the signs and symptoms of CRS, or if no response to second or subsequent doses of tocilizumab, consider alternate measures for treatment of CRS. Grade 3 Per Grade 2 Administer methylprednisolone 1 mg/kg Symptoms require and intravenously twice daily or equivalent respond to aggressive dexamethasone (e.g., 10 mg intravenously intervention. every 6 hours). Oxygen requirement greater Continue corticosteroids use until the than or equal to 40% FiO2 or event is Grade 1 or less, then taper. hypotension requiring If not improving, manage as Grade 4 high-dose or multiple (below). vasopressors or Grade 3 organ toxicity or Grade 4 transaminitis. Grade 4 Per Grade 2 Administer methylprednisolone 1 000 mg Life-threatening symptoms. intravenously per day for 3 days; if Requirements for ventilator improves, then manage as above. support or continuous veno-venous haemodialysis or Consider alternate immunosuppressants if Grade 4 organ toxicity no improvement or if condition worsens. (excluding transaminitis). N/A = not available/not applicable (a) Lee et al 2014. (b) Refer to Table 2 for management of neurologic adverse reactions. (c) Refer to tocilizumab summary of product characteristics for details. Neurologic adverse reactions Severe neurologic adverse reactions, also known as immune effector cell-associated neurotoxicity syndrome (ICANS), have been very commonly observed in patients treated with Yescarta, which could be life-threatening or fatal (see section 4.8). Patients with a history of CNS disorders such as seizures or cerebrovascular ischaemia may be at increased risk. Fatal and serious cases of cerebral oedema have been reported in patients treated with Yescarta. Patients must be monitored for signs and symptoms of neurologic adverse reactions (Table 2). Patients must be monitored at least daily for 10 days at the qualified clinical facility following infusion for signs and symptoms of neurologic toxicity/ICANS. After the first 10 days following the infusion, the patient is to be monitored at the physician’s discretion. Patients are to be counselled to remain within proximity of a qualified clinical facility for at least 4 weeks following infusion and to seek immediate medical attention should signs or symptoms of neurologic toxicity/ICANS occur. Vital signs and organ functions must be monitored depending on the severity of the reaction. Patients who experience Grade 2 or higher neurologic toxicities /ICANS must be monitored with continuous cardiac telemetry and pulse oximetry. Intensive-care supportive therapy must be provided for severe or life-threatening neurologic toxicities. Non-sedating, anti-seizure medicines are to be considered for seizure prophylaxis as clinically indicated for Grade 2 or higher adverse reactions. Treatment algorithms have been developed to ameliorate the neurologic adverse reactions experienced by patients on Yescarta. These include the use of tocilizumab (if concurrent CRS) and/or corticosteroids for moderate, severe, or life-threatening neurologic adverse reactions as summarised in Table 2. Table 2: Neurologic adverse reaction/ICANS grading and management guidance Grading Concurrent CRS No concurrent CRS assessment Grade 2 Administer tocilizumab per Administer dexamethasone 10 mg intravenously every 6 Table 1 for management of hours. Grade 2 CRS. Continue dexamethasone use until the event is Grade 1 or If no improvement within 24 less, then taper. hours after starting tocilizumab, administer dexamethasone 10 mg intravenously every 6 hours if not already taking other corticosteroids. Continue dexamethasone use until the event is Grade 1 or less, then taper. Consider non-sedating, anti-seizure medicines (e.g., levetiracetam) for seizure prophylaxis. Grade 3 Administer tocilizumab per Administer dexamethasone 10 mg intravenously every 6 Table 1 for management of hours. Grade 2 CRS. Continue dexamethasone use until the event is Grade 1 or In addition, administer less, then taper. dexamethasone 10 mg intravenously with the first dose of tocilizumab and repeat dose every 6 hours. Continue dexamethasone use until the event is Grade 1 or less, then taper. Consider non-sedating, anti-seizure medicines (e.g., levetiracetam) for seizure prophylaxis. Grade 4 Administer tocilizumab per Administer methylprednisolone 1 000 mg intravenously per Table 1 for management of day for 3 days; if improves, then manage as above. Grade 2 CRS. Administer methylprednisolone If not improving, consider 1 000 mg of methylprednisolone 1 000 mg intravenously per day intravenously 3 times a day or alternate therapy. a with first dose of tocilizumab and continue methylprednisolone 1 000 mg intravenously per day for 2 more days; if improves, then manage as above. If not improving, consider 1 000 mg of methylprednisolone intravenously 3 times a day or alternate therapy.a Consider non-sedating, anti-seizure medicines (e.g., levetiracetam) for seizure prophylaxis. a. Alternate therapy includes (but is not limited to): anakinra, siltuximab, ruxolitinib, cyclophosphamide, IVIG and ATG. Infections and febrile neutropenia Serious infections have been very commonly observed with Yescarta (see section 4.8). Patients must be monitored for signs and symptoms of infection before, during, and after Yescarta infusion and treated appropriately. Prophylactic anti-microbials should be administered according to standard institutional guidelines. Febrile neutropenia has been observed in patients after Yescarta infusion (see section 4.8) and may be concurrent with CRS. In the event of febrile neutropenia, infection is to be considered and managed with broad spectrum antibiotics, fluids, and other supportive care as medically indicated. Viral reactivation HBV reactivation, in some cases resulting in fulminant hepatitis, hepatic failure, and death, can occur in patients treated with drugs directed against B-cells. Screening for HBV, HCV, and HIV must be performed before collection of cells for manufacturing of Yescarta. Reactivation of JC virus, leading to progressive multifocal leukoencephalopathy (PML), has been reported in patients treated with Yescarta who have also received prior treatment with other immunosuppressive medications. Cases with fatal outcome have been reported. The possibility of PML should be considered in immunosuppressed patients with new onset or worsening neurological symptoms and appropriate diagnostic evaluations should be performed. Prolonged cytopenias Patients may exhibit cytopenias for several weeks following lymphodepleting chemotherapy and Yescarta infusion. Grade 3 or higher prolonged cytopenias following Yescarta infusion occurred very commonly and included thrombocytopenia, neutropenia, and anaemia. Blood counts are to be monitored after treatment with Yescarta. Hypogammaglobulinaemia B-cell aplasia leading to hypogammaglobulinaemia can occur in patients receiving treatment with Yescarta. Hypogammaglobulinaemia has been very commonly observed in patients treated with Yescarta. Immunoglobulin levels should be monitored after treatment with Yescarta and managed using infection precautions, antibiotic prophylaxis, and immunoglobulin replacement. Hypersensitivity reactions Allergic reactions may occur with the infusion of Yescarta. Serious hypersensitivity reactions including anaphylaxis, may be due to DMSO or residual gentamicin in Yescarta. Secondary malignancies including of T-cell origin Patients treated with Yescarta may develop secondary malignancies. T-cell malignancies have been reported following treatment of haematological malignancies with a BCMA- or CD19-directed CAR T- cell therapy, including Yescarta. T-cell malignancies, including CAR-positive malignancies, have been reported within weeks and up to several years following administration of a CD19- or BCMA-directed CAR T-cell therapy. There have been fatal outcomes. Patients are to be monitored life-long for secondary malignancies. In the event that a secondary malignancy of T-cell origin occurs, the company is to be contaced to obtain instructions on patient samples to collect for testing. Tumour lysis syndrome (TLS) TLS, which may be severe, has occasionally been observed. To minimise risk of TLS, patients with elevated uric acid or high tumour burden should receive allopurinol, or an alternative prophylaxis, prior to Yescarta infusion. Signs and symptoms of TLS must be monitored and events managed according to standard guidelines. CD19-negative disease There is limited experience with Yescarta in patients exposed to prior CD19-directed therapy. Yescarta is not recommended if the patient has relapsed with CD19-negative disease after prior anti-CD19 therapy. There are limited data available on CD19-negative patients treated with Yescarta and it is possible that CD19-negative patients may have less benefit compared with CD19-positive patients. Patients with CD19-negative status by immunohistochemistry may still express CD19 and have been shown to benefit from treatment with Yescarta. The potential risks and benefits associated with treatment of CD19-negative patients with Yescarta should be considered. Excipients (sodium) This medicinal product contains 300 mg sodium per infusion bag, equivalent to 15% of the WHO recommended maximum daily intake of 2 g sodium for an adult.
Effects on Driving
4.7 Effects on ability to drive and use machines Yescarta has major influence on the ability to drive and use machines. Due to the potential for neurologic events, including altered mental status or seizures, patients must refrain from driving or operating heavy or potentially dangerous machines until at least 8 weeks after infusion or until resolution of neurologic adverse reactions.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. מבוגרים החולים בלימפומה מסוג DLBCL (Diffuse large B cell lymphoma) שחזרה בתוך 12 חודשים מתום כימואימונותרפיה שניתנה בקו טיפול ראשון, או עמידה לכימואימונותרפיה שניתנה בקו טיפול ראשון. במהלך מחלתו יהיה החולה זכאי לטיפול באחד מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. 2. מבוגרים החולים בלימפומה חוזרת או עמידה (רפרקטורית) מסוג Diffuse large B cell lymphoma, לאחר שני קווי טיפול ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. 3. מבוגרים החולים בלימפומה חוזרת או עמידה (רפרקטורית) מסוג Primary mediastinal B-cell lymphoma, לאחר שני קווי טיפול ומעלה.4. מבוגרים החולים בלימפומה מסוג HGBL (High grade B cell lymphoma) שחזרה בתוך 12 חודשים מתום כימואימונותרפיה שניתנה בקו טיפול ראשון, או עמידה לכימואימונותרפיה שניתנה בקו טיפול ראשון. במהלך מחלתו יהיה החולה זכאי לטיפול באחד מאלה – Axicabtagene ciloleucel, Tisagenlecleucel5. מבוגרים החולים בלימפומה פוליקולרית חוזרת או רפרקטורית לאחר שלושה קווי טיפול קודמים ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel.ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| מבוגרים החולים בלימפומה חוזרת או עמידה (רפרקטורית) מסוג Primary mediastinal B-cell lymphoma, לאחר שני קווי טיפול ומעלה | 30/01/2020 | אונקולוגיה | Primary mediastinal B-cell lymphoma | |
| מבוגרים החולים בלימפומה חוזרת או עמידה (רפרקטורית) מסוג Diffuse large B cell lymphoma, לאחר שני קווי טיפול ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. | 30/01/2020 | אונקולוגיה | Diffuse large b cell lymphoma | |
| מבוגרים החולים בלימפומה פוליקולרית חוזרת או רפרקטורית לאחר שלושה קווי טיפול קודמים ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. | 01/02/2023 | אונקולוגיה | Follicular lymphoma | |
| מבוגרים החולים בלימפומה מסוג HGBL (High grade B cell lymphoma) שחזרה בתוך 12 חודשים מתום כימואימונותרפיה שניתנה בקו טיפול ראשון, או עמידה לכימואימונותרפיה שניתנה בקו טיפול ראשון. במהלך מחלתו יהיה החולה זכאי לטיפול באחד מאלה – Axicabtagene ciloleucel, Tisagenlecleucel | 01/02/2023 | אונקולוגיה | HGBL, High grade B cell lymphoma | |
| מבוגרים החולים בלימפומה מסוג DLBCL (Diffuse large B cell lymphoma) שחזרה בתוך 12 חודשים מתום כימואימונותרפיה שניתנה בקו טיפול ראשון, או עמידה לכימואימונותרפיה שניתנה בקו טיפול ראשון. במהלך מחלתו יהיה החולה זכאי לטיפול באחד מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. | 01/02/2023 | אונקולוגיה | DLBCL, Diffuse large B cell lymphoma |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
30/01/2020
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
ATC
מידע נוסף
עלון מידע לצרכן
11.08.21 - עלון לצרכן אנגלית 11.08.21 - עלון לצרכן אנגלית 11.08.21 - עלון לצרכן אנגלית 11.08.21 - עלון לצרכן עברית 11.08.21 - עלון לצרכן ערבית 05.10.20 - עלון לצרכן אנגלית 05.10.20 - עלון לצרכן עברית 05.10.20 - עלון לצרכן ערבית 14.09.22 - עלון לצרכן אנגלית 14.09.22 - עלון לצרכן עברית 20.09.22 - עלון לצרכן ערבית 29.11.22 - עלון לצרכן אנגלית 29.11.22 - עלון לצרכן עברית 12.12.22 - עלון לצרכן ערבית 21.06.23 - עלון לצרכן אנגלית 11.05.23 - עלון לצרכן אנגלית 11.05.23 - עלון לצרכן עברית 11.05.23 - עלון לצרכן ערבית 12.09.23 - עלון לצרכן אנגלית 12.09.23 - עלון לצרכן עברית 27.09.23 - עלון לצרכן ערבית 12.10.23 - עלון לצרכן אנגלית 12.10.23 - עלון לצרכן אנגלית 12.10.23 - עלון לצרכן עברית 12.10.23 - עלון לצרכן אנגלית 15.10.23 - עלון לצרכן ערבית 01.01.24 - עלון לצרכן אנגלית 31.12.23 - עלון לצרכן עברית 12.01.24 - עלון לצרכן ערבית 28.03.24 - עלון לצרכן אנגלית 28.03.24 - עלון לצרכן עברית 28.03.24 - עלון לצרכן ערבית 13.09.24 - עלון לצרכן אנגלית 13.09.24 - עלון לצרכן עברית 13.09.24 - עלון לצרכן ערבית 05.10.20 - החמרה לעלון 14.09.22 - החמרה לעלון 29.11.22 - החמרה לעלון 11.01.23 - החמרה לעלון 11.05.23 - החמרה לעלון 12.09.23 - החמרה לעלון 06.12.23 - החמרה לעלון 01.01.24 - החמרה לעלון 28.03.24 - החמרה לעלון 13.09.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
יסקרטה