Quest for the right Drug
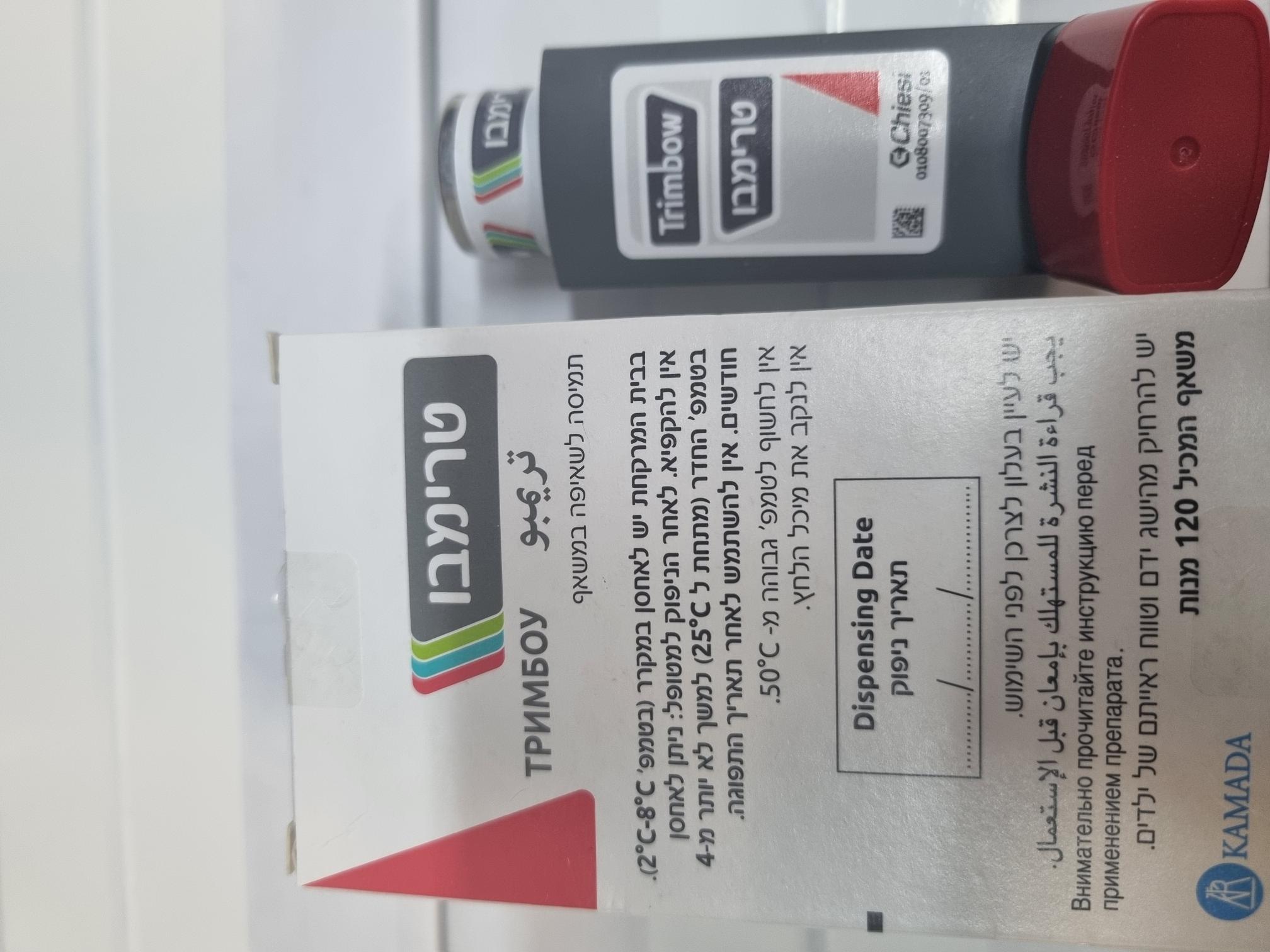
טרימבו 100/6/12.5 TRIMBOW 100/6/12.5 (BECLOMETASONE DIPROPIONATE, FORMOTEROL FUMARATE DIHYDRATE, GLYCOPYRRONIUM AS BROMIDE, GLYCOPYRRONIUM BROMIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
שאיפה : INHALATION
צורת מינון:
אין פרטים : PRESSURISED SOLUTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Drugs for obstructive airway diseases, adrenergics in combination with anticholinergics incl. triple combinations with corticosteroids. ATC code: R03AL09. Mechanism of action and pharmacodynamic effects Trimbow contains beclometasone dipropionate, formoterol and glycopyrronium (BDP/FF/G) in a solution formulation resulting in an aerosol with extrafine particles with an average mass median aerodynamic diameter (MMAD) of around 1.1 micrometres and co-deposition of the three components. The aerosol particles of Trimbow are on average much smaller than the particles delivered in non-extrafine formulations. For beclometasone dipropionate, this results in a more potent effect than formulations with a non-extrafine particle size distribution (100 micrograms of beclometasone dipropionate extrafine in Trimbow are equivalent to 250 micrograms of beclometasone dipropionate in a non-extrafine formulation). Beclometasone dipropionate Beclometasone dipropionate given by inhalation at recommended doses has a glucocorticoid anti- inflammatory action within the lungs. Glucocorticoids are widely used for the suppression of inflammation in chronic inflammatory diseases of the airways. Their action is mediated by the binding to glucocorticoid receptors in the cytoplasm resulting in the increased transcription of genes coding for anti-inflammatory proteins. Formoterol Formoterol is a selective beta2-adrenergic agonist that produces relaxation of bronchial smooth muscle in patients with reversible airways obstruction. The bronchodilating effect sets in rapidly, within 1-3 minutes after inhalation, and has a duration of 12 hours after a single dose. Glycopyrronium Glycopyrronium is a high-affinity, long-acting muscarinic receptor antagonist (anticholinergic) used for inhalation as bronchodilator treatment . Glycopyrronium works by blocking the bronchoconstrictor action of acetylcholine on airway smooth muscle cells, thereby dilating the airways. Glycopyrronium bromide is a high affinity muscarinic receptor antagonist with a greater than 4-fold selectivity for the human M3 receptors over the human M2 receptor as it has been demonstrated. Clinical efficacy and safety COPD The Phase III clinical development programme in COPD was conducted with BDP/FF/G 87/5/9 and included two 52-week active-controlled studies. The TRILOGY study compared BDP/FF/G with a fixed combination of beclometasone dipropionate and formoterol 100/6 micrograms two inhalations twice daily (1,368 randomised patients). The TRINITY study compared BDP/FF/G with tiotropium 18 micrograms inhalation powder, hard capsule, one inhalation once daily; in addition, effects were compared with an extemporary triple combination made of a fixed combination of beclometasone dipropionate and formoterol 100/6 micrograms (corresponding to a delivered dose of 84.6/5.0 micrograms) two inhalations twice daily plus tiotropium 18 micrograms inhalation powder, hard capsule, one inhalation once daily (2,691 randomised patients). Both studies were conducted in patients with a clinical diagnosis of COPD with severe to very severe airflow limitation (FEV1 less than 50% predicted), with symptoms assessed as a COPD Assessment Test (CAT) score of 10 or above, and with at least one COPD exacerbation in the previous year. The two studies included approximately 20% of patients who used the AeroChamber Plus spacer. In addition, two Phase IIIb studies were conducted to support the clinical efficacy and safety of BDP/FF/G. TRISTAR was a 26-week active-controlled open label study comparing BDP/FF/G with an extemporary combination made of a fixed combination of fluticasone/vilanterol 92/22 micrograms inhalation powder, one inhalation once daily plus tiotropium 18 micrograms inhalation powder, hard capsule, one inhalation once daily (1,157 randomised patients). TRIBUTE was a 52-week active-controlled study comparing BDP/FF/G with a fixed combination of indacaterol/glycopyrronium 85/43 micrograms inhalation powder, hard capsule, one inhalation once daily (1,532 randomised patients). Both studies were conducted in a similar population of COPD patients as studies TRILOGY and TRINITY. Reduction of COPD exacerbations Compared with a fixed combination of beclometasone dipropionate and formoterol, BDP/FF/G reduced the rate of moderate/severe exacerbations over 52 weeks by 23% (rate: 0.41 versus 0.53 events per patient/year; p = 0.005). Compared with tiotropium, BDP/FF/G reduced the rate of moderate/severe exacerbations over 52 weeks by 20% (rate: 0.46 versus 0.57 events per patient/year; p = 0.003). Compared with a fixed combination of indacaterol and glycopyrronium, BDP/FF/G reduced the rate of moderate/severe exacerbations over 52 weeks by 15% (rate: 0.50 versus 0.59 events per patient/year; p = 0.043). Compared with tiotropium, BDP/FF/G also reduced the rate of severe exacerbations (i.e. excluding moderate exacerbations) by 32% (rate: 0.067 versus 0.098 events per patient/year; p = 0.017). No differences were observed when comparing BDP/FF/G with the extemporary triple combination made of beclometasone dipropionate and formoterol fixed combination plus tiotropium (moderate/severe exacerbation rate: 0.46 versus 0.45 events per patient/year). In addition, compared with both a fixed combination of beclometasone dipropionate and formoterol and with tiotropium, BDP/FF/G significantly prolonged the time to first exacerbation (hazard ratio 0.80 and 0.84 respectively; p = 0.020 and 0.015 respectively), with no differences between BDP/FF/G and the extemporary triple combination made of beclometasone dipropionate and formoterol fixed combination plus tiotropium (hazard ratio 1.06). Effects on lung function Pre-dose FEV1 Compared with a fixed combination of beclometasone dipropionate and formoterol, BDP/FF/G improved pre-dose FEV1 by 81 mL after 26 weeks of treatment and by 63 mL after 52 weeks of treatment. Compared with tiotropium, BDP/FF/G improved pre-dose FEV1 by 51 mL after 26 weeks of treatment and by 61 mL after 52 weeks of treatment. These improvements were statistically significant (p < 0.001). Compared with a fixed combination of indacaterol and glycopyrronium, BDP/FF/G improved average pre-dose FEV1 over the 52-week treatment period by 22 mL (p=0.018). Similar improvements, although not statistically significant, were observed at weeks 26 and 52. No differences were observed when comparing BDP/FF/G and the extemporary triple combination made of a fixed combination of beclometasone dipropionate and formoterol plus tiotropium (difference of 3 mL in pre- dose FEV1 after 52 weeks of treatment). 2-hour post-dose FEV1 Compared with a fixed combination of beclometasone dipropionate and formoterol, BDP/FF/G significantly improved 2-hour post dose FEV1 by 117 mL after 26 weeks of treatment and by 103 mL after 52 weeks of treatment (p < 0.001). This endpoint was only measured in the TRILOGY study. Inspiratory Capacity (IC) Compared with tiotropium, BDP/FF/G significantly improved IC by 39 mL (p = 0.025) and 60 mL (p = 0.001) after 26 and 52 weeks of treatment respectively. Similar effects were seen when comparing BDP/FF/G with the extemporary triple combination. This endpoint was only measured in the TRINITY study. Symptomatic outcomes BDP/FF/G significantly improved dyspnoea (measured as the Transition Dyspnoea Index – TDI - focal score) after 26 weeks of treatment compared with baseline (by 1.71 units; p < 0.001), but the adjusted mean difference versus a fixed combination of beclometasone dipropionate and formoterol was not statistically significant (0.21 units; p = 0.160). A responder analysis showed that a significantly greater percentage of patients had a clinically significant improvement (focal score greater than or equal to 1) after 26 weeks with BDP/FF/G than with a fixed combination of beclometasone dipropionate and formoterol (57.4% versus 51.8%; p = 0.027). TDI was only measured in the TRILOGY study. BDP/FF/G was also statistically significantly superior to a fixed combination of beclometasone dipropionate and formoterol, to tiotropium and to a fixed combination of indacaterol and glycopyrronium in terms of improvement in quality of life (measured by the Saint George Respiratory Questionnaire – SGRQ - total score). No differences were observed when comparing BDP/FF/G and the extemporary triple combination made of fluticasone and vilanterol fixed combination plus tiotropium. A responder analysis showed that a significantly greater percentage of patients had a clinically significant improvement (reduction versus baseline of greater than or equal to 4) after 26 and 52 weeks with BDP/FF/G than with a fixed combination of beclometasone dipropionate and formoterol and with tiotropium. Asthma The Phase III clinical development programme in asthma included two randomized, double-blind, active- controlled studies of 52 weeks duration, one performed with the medium ICS dose strength (BDP/FF/G 87/5/9; TRIMARAN) and another one with the high ICS dose strength (BDP/FF/G 172/5/9; TRIGGER). Both studies were conducted in adult patients with a clinical diagnosis of asthma who were uncontrolled on dual maintenance treatment using a medium dose (TRIMARAN) or high dose (TRIGGER) ICS/LABA combination (ACQ-7 score ≥1.5). In order to be eligible, patients had to have experienced at least one asthma exacerbation requiring treatment with systemic corticosteroids or emergency department visit or in- patient hospitalisation in the previous year. The TRIMARAN study compared two twice-daily doses of BDP/FF/G 87/5/9 (N=579) with two twice-daily doses of a fixed combination of beclometasone dipropionate (BDP) and formoterol (FF) 100/6 micrograms (delivered dose of 84.6/5.0) (N=576). The TRIGGER study compared two twice-daily doses of BDP/FF/G 172/5/9 (N=573) with two twice-daily doses of a fixed combination of BDP and FF 200/6 micrograms alone (delivered dose 177.7/5.1) (N=576) or on top of two once-daily doses of tiotropium 2.5 micrograms (N=288) as an open-label extemporary triple combination arm. The primary objective of the studies was to demonstrate superiority of either BDP/FF/G 87/5/9 or BDP/FF/G 172/5/9 (two inhalations twice daily) over the respective fixed dual combination product (medium or high dose ICS/LABA) in terms of the co-primary endpoints (change from baseline in pre-dose FEV1 at Week 26 and the rate of moderate and severe exacerbation rate over 52 weeks). The TRIGGER study was not powered to evaluate the comparative efficacy of BDP/FF/G 172/5/9 vs. BDP/FF + tiotropium 2.5 micrograms. Descriptive results are included in Table 1. Median age of patients enrolled in the two pivotal studies was 54 years. Less than 20% of patients were aged 65 years or more and approximately 60% of patients were female. During the study, about 16% (TRIMARAN) and 23% (TRIGGER) of patients used the AeroChamber Plus spacer. Reduction of asthma exacerbations In the TRIMARAN study, BDP/FF/G 87/5/9 significantly reduced the rate of moderate/severe exacerbations compared with the fixed combination of BDP/FF 100/6 micrograms (adjusted rate ratio 0.846, 95%CI [0.725; 0.987]). In the TRIGGER study, BDP/FF/G 172/5/9 also reduced the rate of moderate/severe exacerbations more than the fixed combination of BDP/FF 200/6 micrograms but this effect did not achieve statistical significance (adjusted rate ratio 0.880, 95%CI [0.751;1.030], p=0.11). Due to the hierarchical testing, all TRIGGER efficacy endpoints and the pre-specified analysis of severe exacerbations (data pooled across TRIMARAN and TRIGGER studies) resulted in nominal p-values only (Table 1). Data of TRIMARAN and TRIGGER studies suggest that the time to first moderate/severe exacerbation (secondary endpoint) was prolonged in the triple combination arm when compared with the respective dual combination arm. Effects on lung function In both studies, BDP/FF/G 87/5/9 and BDP/FF/G 172/5/9 improved the lung function parameters of pre-dose FEV1 (co-primary endpoint), peak0-3h FEV1, and morning peak expiratory flow (key secondary endpoints), compared with a fixed combination of beclometasone dipropionate and formoterol 100/6 micrograms and 200/6 micrograms, respectively, after 26 weeks of treatment. All improvements were statistically significant (see Table 1). Table 1 - Results of primary and secondary endpoints Study TRIMARAN TRIGGER Comparison of interest BDP/FF/G 172/5/9 BDP/FF/G 87/5/9 BDP/FF/G 172/5/9 (N=573) (N=579) (N=573) N = randomised patients vs vs vs 1 per treatment arm BDP/FF 177.7/5.1 + BDP/FF1 84.6/5 BDP/FF1 177.7/5.1 tiotropium 2.52 N=576) (N=576) (N=288) Primary endpoints Pre-dose FEV1 after 26 weeks (co-primary endpoint) Treatment difference +57 mL +73 mL -45 mL p-value p = 0.008 p = 0.003* p = 0.125* Moderate/severe exacerbations over 52 weeks (co-primary endpoint) Adjusted rate per patient/year 1.83 vs 2.16 1.73 vs 1.96 1.73 vs 1.63 Rate change -15.4% -12.0% +7.0% p-value p = 0.033 p = 0.110 (n.s.) p = 0.502* Key secondary and secondary endpoints Peak0-3h FEV1 after 26 weeks (key secondary endpoint) Treatment difference +84 mL +105 mL -33 mL p-value p < 0.001 p < 0.001* p = 0.271* Morning peak expiratory flow (PEF) over 26 weeks (key secondary endpoint) Treatment difference +8 L/min +8 L/min -0.2 L/min p-value p < 0.001 p = 0.001* p = 0.951* Rate of severe exacerbations over 52 weeks, pooled analysis (key secondary endpoint) Adjusted rate per patient/year 0.24 vs 0.31 n. a. Rate change -23.0% p-value p = 0.008* Time to the first moderate/severe exacerbation over 52 weeks (secondary endpoint) Hazard ratio 0.84 0.80 1.03 p-value p = 0.022* p = 0.003* p = 0.777* Time to the first severe exacerbation over 52 weeks, pooled analysis (secondary endpoint) Hazard ratio 0.79 n.a. p-value p = 0.011* Co-primary endpoints (pre-dose FEV1 at Week 26 and the rate of moderate and severe exacerbation rate over 52 weeks) and the key secondary endpoints (peak0-3h FEV1 at Week 26, morning PEF over 26 weeks and the rate of severe exacerbations [pooled analysis of TRIMARAN and TRIGGER] over 52 weeks) were part of the step-down, closed confirmatory testing strategy and thus controlled for multiplicity. Since the superiority test of one of the co-primary endpoints in the TRIGGER study did not achieve statistical significance, results for TRIGGER efficacy endpoints and the rate of severe exacerbations (pooled analysis) are nominal p-values and presented for descriptive purposes. Since the TRIGGER study was not powered to evaluate the comparative efficacy of BDP/FF/G 172/5/9 vs. BDP/FF 177.7/5.1 plus tiotropium 2.5, it is not clear whether the observed differences are real or a random result. n.a. =not applicable n.s. = not statistically significant 1 = fixed combination of beclometasone dipropionate (BDP) plus formoterol fumarate (FF) 2 = open-label extemporaneous group * = nominal p-values Paediatric population Trimbow is not indicated for children and adolescents under 18 years of age.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Trimbow – fixed combination The systemic exposure to beclometasone dipropionate, formoterol and glycopyrronium has been investigated in a pharmacokinetic study conducted in healthy subjects. The study compared data obtained after treatment with a single dose of Trimbow (4 inhalations of 100/6/25 micrograms, a non-marketed formulation containing twice the approved strength of glycopyrronium) or a single dose of the extemporary combination of beclometasone dipropionate/formoterol (4 inhalations of 100/6 micrograms) plus glycopyrronium (4 inhalations of 25 micrograms). The maximum plasma concentration and systemic exposure of beclometasone dipropionate main active metabolite (beclometasone 17-monopropionate) and formoterol were similar after administration of the fixed or extemporary combination. For glycopyrronium, the maximum plasma concentration was similar after administration of the fixed or extemporary combination, while the systemic exposure was slightly higher after administration of Trimbow than with the extemporary combination. This study also investigated the potential pharmacokinetic interaction between the active components of Trimbow by comparing the pharmacokinetic data obtained after a single dose of the extemporary combination or after a single dose of the single components beclometasone dipropionate/formoterol or glycopyrronium. There was no clear evidence of pharmacokinetic interaction, however the extemporary combination showed formoterol and glycopyrronium levels transiently slightly higher immediately after dosing compared with the single components. It is noted that single component glycopyrronium, formulated as pressurised metered dose inhaler, which was used in the PK studies, is not available on the market. The dose proportionality of systemic and lung exposure to beclometasone dipropionate has been investigated in a pharmacokinetic study conducted in healthy subjects with non-marketed Trimbow formulations, containing twice the approved strength of glycopyrronium (given as metered dose). The study compared data obtained after treatment with a single dose (4 inhalations) of Trimbow 200/6/25 micrograms or a single dose (4 inhalations) of Trimbow 100/6/25 micrograms (both are non-marketed formulations containing twice the approved strength of glycopyrronium). Trimbow 200/6/25 micrograms treatment resulted in a two times higher systemic and lung exposure to beclometasone dipropionate and to its main active metabolite (beclometasone 17-monopropionate) in comparison to Trimbow 100/6/25 micrograms, which is consistent with the different strengths of the two formulations. The systemic and lung exposure to glycopyrronium and formoterol was similar after the two treatments, although a high variability was observed for glycopyrronium bromide Cmax. A comparison across studies showed that the pharmacokinetics of beclometasone 17-monopropionate, formoterol and glycopyrronium is similar in COPD patients, in patients with asthma and in healthy subjects. Effect of a spacer In patients with COPD, the use of Trimbow with the AeroChamber Plus spacer increased the lung delivery of beclometasone 17-monopropionate, formoterol and glycopyrronium (maximum plasma concentration increased by 15%, 58% and 60% respectively). The total systemic exposure (as measured by AUC0-t) was slightly reduced for beclometasone 17-monopropionate (by 37%) and formoterol (by 24%), while it was increased for glycopyrronium (by 45%). See also section 4.2. Effect of renal impairment Systemic exposure (AUC0-t) to beclometasone dipropionate, to its metabolite beclometasone 17-monopropionate and to formoterol was not affected by mild to severe renal impairment. For glycopyrronium, there was no impact in subjects with mild and moderate renal impairment. However, an increase in total systemic exposure of up to 2.5-fold was observed in subjects with severe renal impairment (glomerular filtration rate below 30 mL/min/1.73 m2), as a consequence of a significant reduction of the amount excreted in urine (approximately 90% reduction of glycopyrronium renal clearance). Simulations performed with a pharmacokinetic model showed that even when covariates had extreme values (body weight less than 40 kg and concomitant glomerular filtration rate below 27 mL/min/1.73 m²), exposure to Trimbow active substances remains in approximately a 2.5-fold range compared to the exposure in a typical patient with median covariate values. Beclometasone dipropionate Beclometasone dipropionate is a pro-drug with weak glucocorticoid receptor binding affinity that is hydrolysed via esterase enzymes to an active metabolite beclometasone 17-monopropionate which has a more potent topical anti-inflammatory activity compared with the pro-drug beclometasone dipropionate. Absorption, distribution and biotransformation Inhaled beclometasone dipropionate is rapidly absorbed through the lungs; prior to absorption there is extensive conversion to beclometasone 17-monopropionate via esterase enzymes that are found in most tissues. The systemic availability of the active metabolite arises from lung (36%) and from gastrointestinal absorption of the swallowed dose. The bioavailability of swallowed beclometasone dipropionate is negligible; however, pre-systemic conversion to beclometasone 17-monopropionate results in 41% of the dose being absorbed as the active metabolite. There is an approximately linear increase in systemic exposure with increasing inhaled dose. The absolute bioavailability following inhalation is approximately 2% and 62% of the nominal dose for unchanged beclometasone dipropionate and beclometasone 17-monopropionate respectively. Following intravenous dosing, the disposition of beclometasone dipropionate and its active metabolite is characterised by high plasma clearance (150 and 120 L/h respectively), with a small volume of distribution at steady state for beclometasone dipropionate (20 L) and larger tissue distribution for its active metabolite (424 L). Plasma protein binding is moderately high. Elimination Faecal excretion is the major route of beclometasone dipropionate elimination mainly as polar metabolites. The renal excretion of beclometasone dipropionate and its metabolites is negligible. The terminal elimination half-lives are 0.5 hours and 2.7 hours for beclometasone dipropionate and beclometasone 17-monopropionate respectively. Patients with hepatic impairment The pharmacokinetics of beclometasone dipropionate in patients with hepatic impairment has not been studied, however, as beclometasone dipropionate undergoes a very rapid metabolism via esterase enzymes present in intestinal fluid, serum, lungs and liver to form the more polar products beclometasone 21-monopropionate, beclometasone 17-monopropionate and beclometasone, hepatic impairment is not expected to modify the pharmacokinetics and safety profile of beclometasone dipropionate. Formoterol Absorption and distribution Following inhalation, formoterol is absorbed from both the lung and the gastrointestinal tract. The fraction of an inhaled dose that is swallowed after administration with a metered dose inhaler may range between 60% and 90%. At least 65% of the fraction that is swallowed is absorbed from the gastrointestinal tract. Peak plasma concentrations of the unchanged active substance occur within 0.5 to 1 hours after oral administration. Plasma protein binding of formoterol is 61-64% with 34% bound to albumin. There was no saturation of binding in the concentration range attained with therapeutic doses. The elimination half-life determined after oral administration is 2-3 hours. Absorption of formoterol is linear following inhalation of 12 to 96 micrograms of formoterol. Biotransformation Formoterol is widely metabolised and the prominent pathway involves direct conjugation at the phenolic hydroxyl group. Glucuronide acid conjugate is inactive. The second major pathway involves O- demethylation followed by conjugation at the phenolic 2'-hydroxyl group. Cytochrome P450 isoenzymes CYP2D6, CYP2C19 and CYP2C9 are involved in the O-demethylation of formoterol. Liver appears to be the primary site of metabolism. Formoterol does not inhibit CYP450 enzymes at therapeutically relevant concentrations. Elimination The cumulative urinary excretion of formoterol after single inhalation from a dry powder inhaler increased linearly in the 12-96 micrograms dose range. On average, 8% and 25% of the dose was excreted as unchanged and total formoterol, respectively. Based on plasma concentrations measured following inhalation of a single 120 micrograms dose by 12 healthy subjects, the mean terminal elimination half-life was determined to be 10 hours. The (R,R)- and (S,S)-enantiomers represented about 40% and 60% of unchanged active substance excreted in the urine, respectively. The relative proportion of the two enantiomers remained constant over the dose range studied and there was no evidence of relative accumulation of one enantiomer over the other after repeated dosing. After oral administration (40 to 80 micrograms), 6% to 10% of the dose was recovered in urine as unchanged active substance in healthy subjects; up to 8% of the dose was recovered as the glucuronide. A total 67% of an oral dose of formoterol is excreted in urine (mainly as metabolites) and the remainder in the faeces. The renal clearance of formoterol is 150 mL/min. Patients with hepatic impairment The pharmacokinetics of formoterol has not been studied in patients with hepatic impairment; however, as formoterol is primarily eliminated via hepatic metabolism, an increased exposure can be expected in patients with severe hepatic impairment. Glycopyrronium Absorption and distribution Glycopyrronium has a quaternary ammonium structure which limits its passage across biological membranes and produces slow, variable and incomplete gastrointestinal absorption. Following glycopyrronium inhalation, the lung bioavailability was 10.5% (with activated charcoal ingestion) while the absolute bioavailability was 12.8% (without activated charcoal ingestion) confirming the limited gastrointestinal absorption and indicating that more than 80% of glycopyrronium systemic exposure was from lung absorption. After repeated inhalation of twice daily doses ranging from 12.5 to 50 micrograms via pressurised metered dose inhaler in COPD patients, glycopyrronium showed linear pharmacokinetics with little systemic accumulation at steady state (median accumulation ratio 2.2-2.5). The apparent volume of distribution (Vz) of inhaled glycopyrronium was increased compared to intravenous infusion (6,420 L versus 323 L), reflecting the slower elimination after inhalation. Biotransformation The metabolic pattern of glycopyrronium in vitro (humans, dogs, rats, mice and rabbits liver microsomes and hepatocytes) was similar among species and the main metabolic reaction was the hydroxylation on the phenyl or ciclopentyl rings. CYP2D6 was found to be the only enzyme responsible for glycopyrronium metabolism. Elimination The mean elimination half-life of glycopyrronium in healthy volunteers was approximately 6 hours after intravenous injection while after inhalation in COPD patients it ranged from 5 to 12 hours at steady state. After a glycopyrronium single intravenous injection, 40% of the dose was excreted in the urine within 24 hours. In COPD patients receiving repeated twice daily administration of inhaled glycopyrronium, the fraction of the dose excreted in urine ranged from 13.0% to 14.5% at steady state. Mean renal clearance was similar across the range of doses tested and after single and repeated inhalation (range 281-396 mL/min).

פרטי מסגרת הכללה בסל
א. מחלת ריאות חסימתית כרונית (COPD – Chronic Obstructive Pulmonary Disease). ב. טיפול אחזקה בחולים בגירים עם אסטמה שעונים על כל אלה:1. מטופלים במינון גבוה בטיפול משולב של קורטיקוסטרואידים בשאיפה (ICS) ותרופות ממשפחת ה-Long acting beta agonists (LABA).2. חוו לפחות החמרה (exacerbation) אחת של מחלתם בשנה האחרונה שחייבה טיפול בסטרואידים סיסטמיים.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| א. מחלת ריאות חסימתית כרונית (COPD – Chronic Obstructive Pulmonary Disease). ב. טיפול אחזקה בחולים בגירים עם אסטמה שעונים על כל אלה: 1. מטופלים במינון גבוה בטיפול משולב של קורטיקוסטרואידים בשאיפה (ICS) ותרופות ממשפחת ה-Long acting beta agonists (LABA). 2. חוו לפחות החמרה (exacerbation) אחת של מחלתם בשנה האחרונה שחייבה טיפול בסטרואידים סיסטמיים. | 17/03/2024 | רפואת ריאות | מחלת ריאות חסימתית כרונית, COPD – Chronic Obstructive Pulmonary Disease | |
| מחלת ריאות חסימתית כרונית (COPD – Chronic Obstructive Pulmonary Disease) בחולים עם FEV1 שווה או נמוך מ-60% במצב כרוני; |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
16/01/2019
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
