Quest for the right Drug
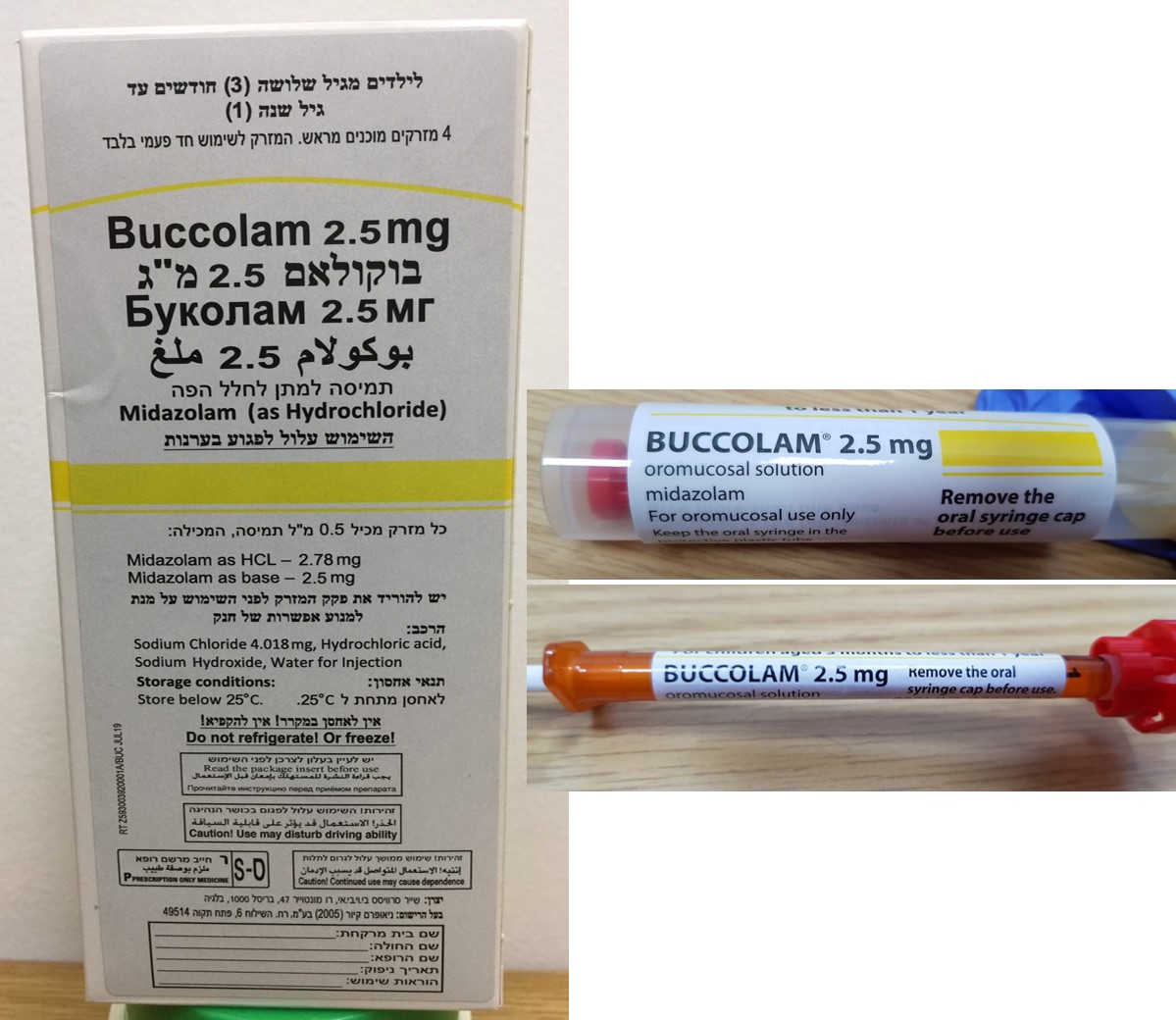
בוקולאם 2.5 מ"ג BUCCOLAM 2.5 MG (MIDAZOLAM AS HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פנים הלחי : BUCCAL
צורת מינון:
תמיסה לחלל הפה : OROMUCOSAL SOLUTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Psycholeptics, benzodiazepine derivatives ATC code: N05CD08 Mechanism of action Midazolam is a derivative of the imidazobenzodiazepine group. The free base is a lipophilic substance with low solubility in water. The basic nitrogen in position 2 of the imidazobenzodiazepine ring system enables midazolam to form the hydrochloride salt with acids. These produce a stable solution suitable for oromucosal administration. Pharmacodynamic effects The pharmacological action of midazolam is characterized by short duration because of rapid metabolic transformation. Midazolam has an anticonvulsant effect. It also exerts a sedative and sleep-inducing effect of pronounced intensity, and an anxiolytic and a muscle-relaxant effect. Clinical efficacy and safety In 4 rectal diazepam controlled studies and one study versus intravenous diazepam, in a total of 688 children, cessation of visible signs of seizures within 10 minutes was observed in 65% to 78% of children receiving oromucosal midazolam. Additionally, in 2 of the studies, cessation of visible signs of seizures within 10 minutes without recurrence within 1 hour after administration was observed in 56% to 70% of children. The frequency and severity of adverse drug reactions reported for oromucosal midazolam during published clinical trials were similar to the adverse drug reactions reported in the comparative group using rectal diazepam.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Simulated pharmacokinetic parameters for the recommended posology in children aged 3 months to less than 18 years, based on a population pharmacokinetic study are provided in tabulated format below: Dose Age Parameter Mean SD 2.5 mg 3 m < 1 yr AUC0-inf (ng.h/ml) 168 98 Cmax (ng/ml) 104 46 5 mg 1 yr < 5 yrs AUC0-inf (ng.h/ml) 242 116 Cmax (ng/ml) 148 62 7.5 mg 5 yrs <10 yrs AUC0-inf (ng.h/ml) 254 136 Cmax (ng/ml) 140 60 10 mg 10 yrs < 18 yrs AUC0-inf (ng.h/ml) 189 96 Cmax (ng/ml) 87 44 Absorption After oromucosal administration midazolam is absorbed rapidly. Maximum plasma concentration is reached within 30 minutes in children. The absolute bioavailability of oromucosal midazolam is about 75% in adults. The bioavailability of oromucosal midazolam has been estimated at 87% in children with severe malaria and convulsions. Distribution Midazolam is highly lipophilic and distributes extensively. The steady state volume of distribution following oromucosal administration is estimated to be 5.3 l/kg. Approximately 96-98% of midazolam is bound to plasma proteins. The major fraction of plasma protein binding is due to albumin. There is a slow and insignificant passage of midazolam into the cerebrospinal fluid. In humans, midazolam has been shown to cross the placenta slowly and to enter foetal circulation. Small quantities of midazolam are found in human milk. Biotransformation Midazolam is almost entirely eliminated by biotransformation. The fraction of the dose extracted by the liver has been estimated to be 30-60%. Midazolam is hydroxylated by the cytochrome P4503A4 isozyme and the major urinary and plasma metabolite is alpha-hydroxy-midazolam. Following oromucosal administration in children the area under the curve ratio for alpha-hydroxy midazolam to midazolam is 0.46. In a population pharmacokinetic study, the metabolite levels are shown to be higher in younger than older paediatric patients and thus likely to be of more importance in children than in adults. Elimination Plasma clearance of midazolam in children following oromucosal administration is 30 ml/kg/min. The initial and terminal elimination half-lives are 27 and 204 minutes, respectively. Midazolam is excreted mainly by the renal route (60-80% of the injected dose) and recovered as glucuroconjugated alpha-hydroxy-midazolam. Less than 1% of the dose is recovered in urine as unchanged medicinal product. Pharmacokinetics in special populations Obese The mean half-life is greater in obese than in non-obese patients (5.9 versus 2.3 hours). This is due to an increase of approximately 50% in the volume of distribution corrected for total body weight. The clearance is not significantly different in obese and non-obese patients. Hepatic impairment The elimination half-life in cirrhotic patients may be longer and the clearance lower as compared to those in healthy volunteers (see section 4.4). Renal impairment The elimination half-life in patients with chronic renal failure is similar to that in healthy volunteers. The elimination half-life of midazolam is prolonged up to six times in the critically ill. Cardiac insufficiency The elimination half-life is longer in patients with congestive heart failure compared with that in healthy subjects (see section 4.4). Exposure following a second dose in the same seizure episode Simulated exposure data show that the overall AUC approximately doubles when a second dose is administered at 10, 30 and 60 minutes following the first dose. A second dose at 10 minutes results in a significant increase in mean Cmax of between 1.7 to 1.9-fold. At 30 and 60 minutes, significant elimination of midazolam has already occurred and therefore the increase in mean Cmax is less pronounced; 1.3 to 1.6 and 1.2 to 1.5-fold respectively. (see section 4.2). Race Clinical studies have included patients from Japanese and non-Japanese groups, and no differences in the pharmacokinetic profile have been identified on exposure to BUCCOLAM. No dose adjustment is warranted.

פרטי מסגרת הכללה בסל
התרופה תינתן לטיפול בהתקפי פרכוסים חריפים ממושכים בחולי אפילפסיה בגילאי 3 חודשים עד גיל 18 שנים.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| טיפול בהתקפי פרכוסים חריפים ממושכים בחולי אפילפסיה בגילאי 3 חודשים עד גיל 18 שנים. | ||||
| סטטוס אפילפטיקוס | ||||
| ATARALGESIA בשילוב עם קטאמין בילדים | ||||
| אינדוקציה ואחזקה של הרדמה | ||||
| סדציה בסיסית לפני התערבות אבחונית או כירורגית המבוצעת תחת הרדמה מקומית | ||||
| פרה-מדיקציה לפני אינדוקציה להרדמה |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
09/01/2013
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
12.10.22 - עלון לצרכן אנגלית 29.08.22 - עלון לצרכן עברית 12.10.22 - עלון לצרכן ערבית 12.10.22 - עלון לצרכן עברית 08.03.23 - עלון לצרכן אנגלית 08.03.23 - עלון לצרכן ערבית 02.04.24 - עלון לצרכן אנגלית 02.04.24 - עלון לצרכן עברית 19.09.24 - עלון לצרכן אנגלית 19.09.24 - עלון לצרכן עברית 19.09.24 - עלון לצרכן ערבית 14.07.19 - החמרה לעלון 12.01.21 - החמרה לעלון 13.04.22 - החמרה לעלון 12.10.22 - החמרה לעלון 03.04.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
בוקולאם 2.5 מ"ג