Quest for the right Drug
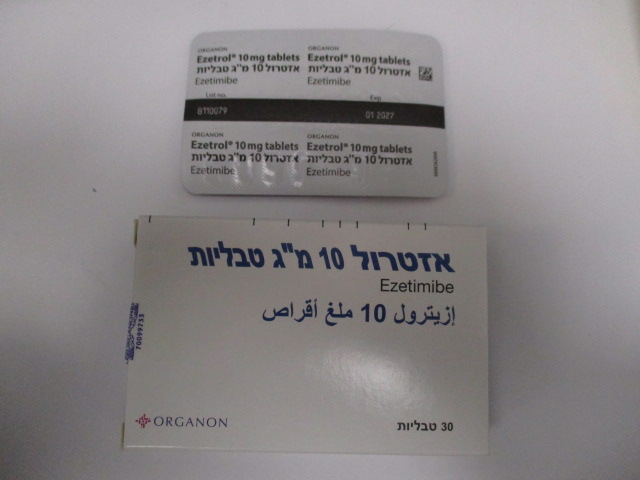
אזטרול 10 מ"ג טבליות EZETROL 10 MG TABLETS (EZETIMIBE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Tabulated list of adverse reactions (clinical studies and post-marketing experience) In clinical studies of up to 112 weeks duration, Ezetrol 10 mg daily was administered alone in 2396 patients, with a statin in 11,308 patients or with fenofibrate in 185 patients. Adverse reactions were usually mild and transient. The overall incidence of side effects was similar between Ezetrol and placebo. Similarly, the discontinuation rate due to adverse experiences was comparable between Ezetrol and placebo. Ezetrol administered alone or co-administered with a statin: The following adverse reactions were observed in patients treated with Ezetrol (n=2396) and at a greater incidence than placebo (n=1159) or in patients treated with Ezetrol coadministered with a statin (n=11308) and at a greater incidence than statin administered alone (n=9361). Post-marketing Adverse reactions were derived from reports containing Ezetrol either administered alone or with a statin. Adverse reactions observed in clinical studies of Ezetrol (as a monotherapy or co-administered with a statin) or Ezetrol reported from post-marketing use either administered alone or with a statin are listed in Table 1. These reactions are presented by system organ class and by frequency. Frequencies are defined as: very common (≥1/10); common (≥1/100 to <1/10); uncommon (≥1/1,000 to <1/100); rare (≥1/10,000 to <1/1,000), very rare (<1/10,000) and not known (cannot be estimated from the available data) Table 1 Adverse Recations System organ class Adverse reaction Frequency Blood and lymphatic system disorders Not known thrombocytopaenia Immune system disorders Not known hypersensitivity; including rash; urticaria; anaphylaxis and angio-oedema Metabolism and nutrition disorders Uncommon decreased appetite Psychiatric disorders Not known depression Nervous system disorders Common headache Uncommon paraesthesia Not known dizziness Vascular disorders Uncommon hot flush; hypertension Respiratory, thoracic and mediastinal disorders Uncommon cough Not known dyspnoea Gastrointestinal disorders Common abdominal pain; diarrhoea; flatulence Uncommon dyspepsia; gastrooesophageal reflux disease; nausea; dry mouth; gastritis Not known pancreatitis; constipation Hepatobiliary disorders Not known hepatitis; cholelithiasis; cholecystitis Skin and subcutaneous tissue disorders Uncommon pruritus; rash; urticaria Not known erythema multiforme Musculoskeletal and connective tissue disorders Common myalgia Uncommon arthralgia; muscle spasms; neck pain; back pain; muscular weakness; pain in extremity Not known myopathy/rhabdomyolysis (see section 4.4) General disorders and administration site conditions Common fatigue Uncommon chest pain; pain; asthenia; oedema peripheral Investigations Common ALT and/or AST increased Uncommon blood CPK increased; gamma-glutamyltransferase increased; liver function test abnormal Ezetrol monotherapy System organ class Adverse reactions Frequency Investigations ALT and/or AST increased; blood CPK Uncommon increased; gamma-glutamyltransferase increased; liver function test abnormal Respiratory, Thoracic and Mediastinal cough Uncommon Disorders Gastrointestinal Disorders abdominal pain; diarrhoea; flatulence Common dyspepsia; gastrooesophageal reflux disease; Uncommon nausea Musculoskeletal And Connective arthralgia; muscle spasms; neck pain Uncommon Tissue Disorders Metabolism and Nutrition Disorders decreased appetite Uncommon Vascular Disorders hot flush; hypertension Uncommon General Disorders And fatigue Common Administration Site Condition chest pain, pain Uncommon Additional adverse reactions with Ezetrol co-administered with a statin System organ class Adverse reactions Frequency Investigations ALT and/or AST increased Common Nervous System Disorders headache Common paraesthesia Uncommon Gastrointestinal Disorders dry mouth; gastritis Uncommon Skin And Subcutaneous Tissue pruritus; rash; urticaria Uncommon Disorders Musculoskeletal And Connective myalgia Common Tissue Disorders back pain; muscular weakness; pain in Uncommon extremity General Disorders And asthenia; oedema peripheral Uncommon Administration Site Condition Post-marketing Experience (with or without a statin) System organ class Adverse reactions Frequency Blood and lymphatic system disorders thrombocytopaenia Not known Nervous system disorders: dizziness; paraesthesia Not known Respiratory, thoracic and mediastinal dyspnoea Not known disorders Gastrointestinal disorders pancreatitis; constipation Not known Skin and subcutaneous tissue erythema multiforme Not known disorders Musculoskeletal and connective tissue myalgia; myopathy/rhabdomyolysis (see Not known disorder section 4.4) General disorders and administration asthenia Not known site conditions Immune system disorders hypersensitivity, including rash, urticaria, Not known anaphylaxis and angio-oedema Hepatobiliary disorders hepatitis; cholelithiasis; cholecystitis Not known Psychiatric disorders depression Not known Ezetrol co-administered with fenofibrate Gastrointestinal disorders: abdominal pain (common) In a multicentre, double-blind, placebo-controlled, clinical study in patients with mixed hyperlipidaemia, 625 patients were treated for up to 12 weeks and 576 patients for up to 1 year. In this study, 172 patients treated with Ezetrol and fenofibrate completed 12 weeks of therapy, and 230 patients treated with Ezetrol and fenofibrate (including 109 who received Ezetrol alone for the first 12 weeks) completed 1 year of therapy. This study was not designed to compare treatment groups for infrequent events. Incidence rates (95 % CI) for clinically important elevations (> 3 X ULN, consecutive) in serum transaminases were 4.5 % (1.9, 8.8) and 2.7 % (1.2, 5.4) for fenofibrate monotherapy and Ezetrol co-administered with fenofibrate, respectively, adjusted for treatment exposure. Corresponding incidence rates for cholecystectomy were 0.6 % (0.0, 3.1) and 1.7 % (0.6, 4.0) for fenofibrate monotherapy and Ezetrol co- administered with fenofibrate, respectively (see sections 4.4 and 4.5). Paediatric (10 to 17 years of age) Patients In a separate study involving adolescent (10 to 17 years of age) patients with heterozygous familial hypercholesterolaemia (n = 248), elevations of ALT and/or AST (≥3X ULN, consecutive) were observed in 3% (4 patients) of the ezetimibe/simvastatin patients compared to 2% (2 patients) in the simvastatin monotherapy group; these figures were respectively 2% (2 patients) and 0% for elevation of CPK (≥ 10X ULN). No cases of myopathy were reported. These trials were not suited for comparison of rare adverse drug reactions. Patients with Coronary Heart Disease and ACS Event History In the IMPROVE-IT study (see section 5.1), involving 18,144 patients treated with either ezetimibe/simvastatin 10/40 mg (n=9067; of whom 6% were uptitrated to ezetimibe/simvastatin 10/80 mg) or simvastatin 40 mg (n=9077; of whom 27% were uptitrated to simvastatin 80 mg), the safety profiles were similar during a median follow-up period of 6.0 years. Discontinuation rates due to adverse experiences were 10.6% for patients treated with ezetimibe/simvastatin and 10.1% for patients treated with simvastatin. The incidence of myopathy was 0.2% for ezetimibe/simvastatin and 0.1% for simvastatin, where myopathy was defined as unexplained muscle weakness or pain with a serum CK ≥10 times ULN or two consecutive observations of CK ≥5 and <10 times ULN. The incidence of rhabdomyolysis was 0.1% for ezetimibe/simvastatin and 0.2% for simvastatin, where rhabdomyolysis was defined as unexplained muscle weakness or pain with a serum CK ≥10 times ULN with evidence of renal injury, ≥5 times ULN and <10 times ULN on two consecutive occasions with evidence of renal injury or CK ≥10,000 IU/L without evidence of renal injury. The incidence of consecutive elevations of transaminases (≥3 X ULN) was 2.5% for ezetimibe/simvastatin and 2.3% for simvastatin. (See section 4.4.) Gallbladder-related adverse effects were reported in 3.1% vs 3.5% of patients allocated to ezetimibe/simvastatin and simvastatin, respectively. The incidence of cholecystectomy hospitalizations was 1.5% in both treatment groups. Cancer (defined as any new malignancy) was diagnosed during the trial in 9.4% vs 9.5%, respectively. Patients with Chronic Kidney Disease In the Study of Heart and Renal Protection (SHARP) (see section 5.1), involving over 9000 patients treated with a fixed dose combination of Ezetrol 10 mg with simvastatin 20 mg daily (n=4650) or placebo (n=4620), the safety profiles were comparable during a median follow-up period of 4.9 years. In this trial, only serious adverse events and discontinuations due to any adverse events were recorded. Discontinuation rates due to adverse events were comparable (10.4% in patients treated with Ezetrol combined with simvastatin, 9.8% in patients treated with placebo). The incidence of myopathy/rhabdomyolysis was 0.2% in patients treated with Ezetrol combined with simvastatin and 0.1% in patients treated with placebo. Consecutive elevations of transaminases (> 3X ULN) occurred in 0.7% of patients treated with Ezetrol combined with simvastatin compared with 0.6% of patients treated with placebo. (See section 4.4.) In this trial, there were no statistically significant increases in the incidence of pre-specified adverse events, including cancer (9.4% for Ezetrol combined with simvastatin, 9.5% for placebo), hepatitis, cholecystectomy or complications of gallstones or pancreatitis. Laboratory values: In controlled clinical monotherapy trials, the incidence of clinically important elevations in serum transaminases (ALT and/or AST ≥ 3 X ULN, consecutive) was similar between Ezetrol (0.5 %) and placebo (0.3 %). In co-administration trials, the incidence was 1.3 % for patients treated with Ezetrol co- administered with a statin and 0.4 % for patients treated with a statin alone. These elevations were generally asymptomatic, not associated with cholestasis, and returned to baseline after discontinuation of therapy or with continued treatment. (see section 4.4.). In clinical trials, CPK >10 X ULN was reported for 4 of 1674 (0.2 %) patients administered Ezetrol alone vs 1 of 786 (0.1 %) patients administered placebo, and for 1 of 917 (0.1 %) patients co-administered Ezetrol and a statin vs 4 of 929 (0.4 %) patients administered a statin alone. There was no excess of myopathy or rhabdomyolysis associated with Ezetrol compared with the relevant control arm (placebo or statin alone). (see section 4.4). Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form http://forms.gov.il/globaldata/getsequence/getsequence.aspx?formType=AdversEffectMedic@moh.gov.il

פרטי מסגרת הכללה בסל
התרופה האמורה תינתן להשגת ערך LDL נמוך או שווה ל-100 מ"ג % בחולה שמיצה טיפול תרופתי מירבי בסטטינים, והעונה על אחד מאלה: 1. חולה סוכרת הסובל גם ממחלה כלילית פעילה בשנה האחרונה. 2. חולה היפרכולסטרולמיה משפחתית (Familial hypercholesterolemia) בהמלצת מומחה ברפואה פנימית, ברפואת המשפחה או ברפואת ילדים המתמחה בליפידים או בקרדיולוגיה. 3. חולה שסבל ממחלה כלילית חדה בשנה האחרונה.
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
15/05/2006
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
