Quest for the right Drug
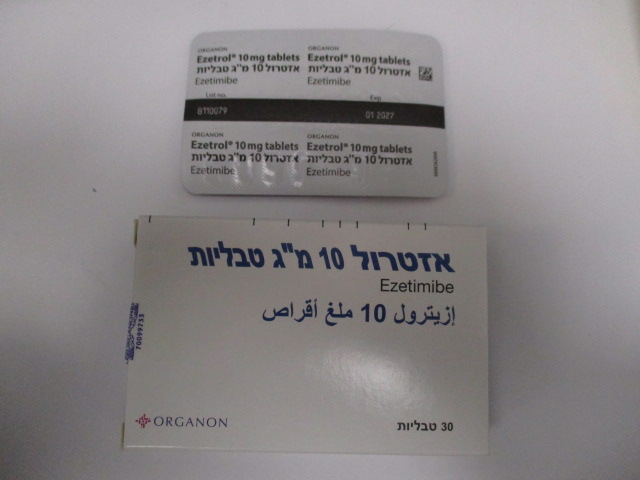
אזטרול 10 מ"ג טבליות EZETROL 10 MG TABLETS (EZETIMIBE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use When Ezetrol is co-administered with a statin, please refer to the SPC for that particular medicinal product. Liver Enzymes In controlled co-administration trials in patients receiving Ezetrol with a statin, consecutive transaminase elevations (≥ 3 X the upper limit of normal [ULN]) have been observed. When Ezetrol is co-administered with a statin, liver function tests should be performed at initiation of therapy and according to the recommendations of the statin. (see section 4.8). In the IMProved Reduction of Outcomes: Vytorin Efficacy International Trial (IMPROVE-IT), 18,144 patients with coronary heart disease and ACS event history were randomized to receive ezetimibe/simvastatin 10/40 mg daily (n=9067) or simvastatin 40 mg daily (n=9077). During a median follow-up of 6.0 years, the incidence of consecutive elevations of transaminases (≥3 X ULN) was 2.5% for ezetimibe/simvastatin and 2.3% for simvastatin. (See section 4.8) In a controlled clinical study in which over 9000 patients with chronic kidney disease were randomized to receive Ezetrol 10 mg combined with simvastatin 20 mg daily (n=4650) or placebo (n=4620) (median follow-up period of 4.9 years), the incidence of consecutive elevations of transaminases (>3 X ULN) was 0.7% for Ezetrol combined with simvastatin and 0.6% for placebo (see section 4.8). Skeletal Muscle In post-marketing experience with Ezetrol, cases of myopathy and rhabdomyolysis have been reported. Most patients who developed rhabdomyolysis were taking a statin concomitantly with Ezetrol. However, rhabdomyolysis has been reported very rarely with Ezetrol monotherapy and very rarely with the addition of Ezetrol to other agents known to be associated with increased risk of rhabdomyolysis. If myopathy is suspected based on muscle symptoms or is confirmed by a creatine phosphokinase (CPK) level >10 times the ULN, Ezetrol, any statin, and any of these other agents that the patient is taking concomitantly should be immediately discontinued. All patients starting therapy with Ezetrol should be advised of the risk of myopathy and told to report promptly any unexplained muscle pain, tenderness or weakness (see section 4.8). In IMPROVE-IT, 18,144 patients with coronary heart disease and ACS event history were randomized to receive ezetimibe/simvastatin 10/40 mg daily (n=9067) or simvastatin 40 mg daily (n=9077). During a median follow-up of 6.0 years, the incidence of myopathy was 0.2% for ezetimibe/simvastatin and 0.1% for simvastatin, where myopathy was defined as unexplained muscle weakness or pain with a serum CK ≥10 times ULN or two consecutive observations of CK ≥5 and <10 times ULN. The incidence of rhabdomyolysis was 0.1% for ezetimibe/simvastatin and 0.2% for simvastatin, where rhabdomyolysis was defined as unexplained muscle weakness or pain with a serum CK ≥10 times ULN with evidence of renal injury, ≥5 times ULN and <10 times ULN on two consecutive occasions with evidence of renal injury or CK ≥10,000 IU/L without evidence of renal injury. (See section 4.8.) In a clinical trial in which over 9000 patients with chronic kidney disease were randomized to receive Ezetrol 10 mg combined with simvastatin 20 mg daily (n=4650) or placebo (n=4620) (median follow-up 4.9 years), the incidence of myopathy/rhabdomyolysis was 0.2% for Ezetrol combined with simvastatin and 0.1% for placebo. (see section 4.8). Patients with hepatic impairment Due to the unknown effects of the increased exposure to ezetimibe in patients with moderate or severe hepatic impairment, Ezetrol is not recommended (see section 5.2). Paediatric population Efficacy and safety of Ezetrol in patients 6 to10 years of age with heterozygous familial or non-familial hypercholesterolemia have been evaluated in a 12-week placebo-controlled clinical trial. Effects of ezetimibe for treatment periods > 12 weeks have not been studied in this age group (see sections 4.2, 4.8, 5.1 and 5.2). Ezetrol has not been studied in patients younger than 6 years of age (see sections 4.2 and 4.8). Efficacy and safety of Ezetrol co-administered with simvastatin in patients 10 to 17 years of age with heterozygous familial hypercholesterolemia have been evaluated in a controlled clinical trial in adolescent boys (Tanner stage II or above) and in girls who were at least one year post-menarche. In this limited controlled study, there was generally no detectable effect on growth or sexual maturation in the adolescent boys or girls, or any effect on menstrual cycle length in girls. However, the effects of ezetimibe for a treatment period > 33 weeks on growth and sexual maturation have not been studied (see sections 4.2 and 4.8). The safety and efficacy of Ezetrol co-administered with doses of simvastatin above 40mg daily have not been studied in paediatric patients 10 to 17 years of age. The safety and efficacy of Ezetrol co-administered with simvastatin have not been studied in paediatric patients < 10 years of age (see sections 4.2 and 4.8). The long-term efficacy of therapy with Ezetrol in patients below 17 years of age to reduce morbidity and mortality in adulthood has not been studied. Fibrates The safety and efficacy of Ezetrol administered with fibrates have not been established. If cholelithiasis is suspected in a patient receiving Ezetrol and fenofibrate, gallbladder investigations are indicated and this therapy should be discontinued (see sections 4.5 and 4.8). Ciclosporin Caution should be exercised when initiating Ezetrol in the setting of ciclosporin. Ciclosporin concentrations should be monitored in patients receiving Ezetrol and ciclosporin (see section 4.5). Anticoagulants If Ezetrol is added to warfarin, another coumarin anticoagulant, or fluindione, the International Normalised Ratio (INR) should be appropriately monitored (see section 4.5). Excipient Patients with rare hereditary problems of galactose intolerance, the Lapp lactase deficiency or glucose- galactose malabsorption should not take this medicine. Ezetrol contains less than 1mmol (23 mg) sodium per tablet, that is to say essentially sodium-free.
Effects on Driving
4.7 Effects on ability to drive and use machines No studies on the effects on the ability to drive and use machines have been performed. However, when driving vehicles or operating machines, it should be taken into account that dizziness has been reported.

פרטי מסגרת הכללה בסל
התרופה האמורה תינתן להשגת ערך LDL נמוך או שווה ל-100 מ"ג % בחולה שמיצה טיפול תרופתי מירבי בסטטינים, והעונה על אחד מאלה: 1. חולה סוכרת הסובל גם ממחלה כלילית פעילה בשנה האחרונה. 2. חולה היפרכולסטרולמיה משפחתית (Familial hypercholesterolemia) בהמלצת מומחה ברפואה פנימית, ברפואת המשפחה או ברפואת ילדים המתמחה בליפידים או בקרדיולוגיה. 3. חולה שסבל ממחלה כלילית חדה בשנה האחרונה.
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
15/05/2006
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
