Quest for the right Drug
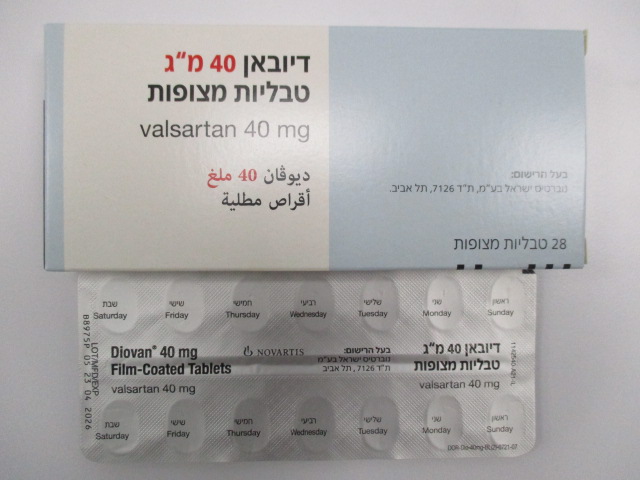
דיובאן ® 40 מ"ג טבליות מצופות DIOVAN ® 40 MG FILM-COATED TABLETS (VALSARTAN)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Angiotensin II antagonists.plain, ATC code: C09CA03. Valsartan is an orally active, potent and specific angiotensin II (Ang II) receptor antagonist. It acts selectively on the AT1 receptor subtype, which is responsible for the known actions of angiotensin II. The increased plasma levels of Ang II following AT1 receptor blockade with valsartan may stimulate the unblocked AT2 receptor, which appears to counterbalance the effect of the AT1 receptor. Valsartan does not exhibit any partial agonist activity at the AT1 receptor and has much (about 20,000 fold) greater affinity for the AT1 receptor than for the AT2 receptor. Valsartan is not known to bind to or block other hormone receptors or ion channels known to be important in cardiovascular regulation. Valsartan does not inhibit ACE (also known as kininase II) which converts Ang I to Ang II and degrades bradykinin. Since there is no effect on ACE and no potentiation of bradykinin or substance P, angiotensin II antagonists are unlikely to be associated with coughing. In clinical trials where valsartan was compared with an ACE inhibitor, the incidence of dry cough was significantly (P < 0.05) less in patients treated with valsartan than in those treated with an ACE inhibitor (2.6% versus 7.9% respectively). In a clinical trial of patients with a history of dry cough during ACE inhibitor therapy, 19.5% of trial subjects receiving valsartan and 19.0% of those receiving a thiazide diuretic experienced cough compared to 68.5% of those treated with an ACE inhibitor (P < 0.05). Hypertension (only 80 mg and 160 mg) Administration of Diovan to patients with hypertension results in reduction of blood pressure without affecting pulse rate. In most patients, after administration of a single oral dose, onset of antihypertensive activity occurs within 2 hours, and the peak reduction of blood pressure is achieved within 4-6 hours. The antihypertensive effect persists over 24 hours after dosing. During repeated dosing, the antihypertensive effect is substantially present within 2 weeks, and maximal effects are attained within 4 weeks and persist during long-term therapy. Combined with hydrochlorothiazide, a significant additional reduction in blood pressure is achieved. Abrupt withdrawal of Diovan has not been associated with rebound hypertension or other adverse clinical events. DIO SPI SEP23 V1.3 In hypertensive patients with type 2 diabetes and microalbuminuria, valsartan has been shown to reduce the urinary excretion of albumin. The MARVAL (Micro Albuminuria Reduction with Valsartan) study assessed the reduction in urinary albumin excretion (UAE) with valsartan (80-160 mg/od) versus amlodipine (5-10 mg/od), in 332 type 2 diabetic patients (mean age: 58 years; 265 men) with microalbuminuria (valsartan: 58 μg/min; amlodipine: 55.4 μg/min), normal or high blood pressure and with preserved renal function (blood creatinine <120 μmol/l). At 24 weeks, UAE was reduced (p<0.001) by 42% (–24.2 μg/min; 95% CI: –40.4 to – 19.1) with valsartan and approximately 3% (–1.7 μg/min; 95% CI: –5.6 to 14.9) with amlodipine despite similar rates of blood pressure reduction in both groups. The Diovan Reduction of Proteinuria (DROP) study further examined the efficacy of valsartan in reducing UAE in 391 hypertensive patients (BP=150/88 mmHg) with type 2 diabetes, albuminuria (mean=102 μg/min; 20-700 μg/min) and preserved renal function (mean serum creatinine = 80 μmol/l). Patients were randomized to one of 3 doses of valsartan (160, 320 and 640 mg/od) and treated for 30 weeks. The purpose of the study was to determine the optimal dose of valsartan for reducing UAE in hypertensive patients with type 2 diabetes. At 30 weeks, the percentage change in UAE was significantly reduced by 36% from baseline with valsartan 160 mg (95%CI: 22 to 47%), and by 44% with valsartan 320 mg (95%CI: 31 to 54%). It was concluded that 160-320 mg of valsartan produced clinically relevant reductions in UAE in hypertensive patients with type 2 diabetes. Recent myocardial infarction (40 mg, 80 mg and 160 mg) The VALsartan In Acute myocardial iNfarcTion trial (VALIANT) was a randomized, controlled, multinational, double-blind study in 14,703 patients with acute myocardial infarction and signs, symptoms or radiological evidence of congestive heart failure and/or evidence of left ventricular systolic dysfunction (manifested as an ejection fraction ≤ 40% by radionuclide ventriculography or ≤ 35% by echocardiography or ventricular contrast angiography). Patients were randomized within 12 hours to 10 days after the onset of myocardial infarction symptoms to valsartan, captopril, or the combination of both. The mean treatment duration was two years. The primary endpoint was time to all-cause mortality. Valsartan was as effective as captopril in reducing all-cause mortality after myocardial infarction. All-cause mortality was similar in the valsartan (19.9%), captopril (19.5%), and valsartan + captopril (19.3%) groups. Combining valsartan with captopril did not add further benefit over captopril alone. There was no difference between valsartan and captopril in all-cause mortality based on age, gender, race, baseline therapies or underlying disease. Valsartan was also effective in prolonging the time to and reducing cardiovascular mortality, hospitalization for heart failure, recurrent myocardial infarction, resuscitated cardiac arrest, and non-fatal stroke (secondary composite endpoint). The safety profile of valsartan was consistent with the clinical course of patients treated in the post-myocardial infarction setting. Regarding renal function, doubling of DIO SPI SEP23 V1.3 serum creatinine was observed in 4.2% of valsartan-treated patients, 4.8 % of valsartan + captopril-treated patients and 3.4% of captopril-treated patients. Discontinuations due to various types of renal dysfunction occurred in 1.1% of valsartan-treated patients, 1.3% in valsartan + captopril patients, and 0.8% of captopril patients. An assessment of renal function should be included in the evaluation of patients post-myocardial infarction. There was no difference in all-cause mortality or cardiovascular mortality or morbidity when beta-blockers were administered together with the combination of valsartan + captopril, valsartan alone, or captopril alone. Irrespective of treatment, mortality was lower in the group of patients treated with a beta-blocker, suggesting that the known beta blocker benefit in this population was maintained in this trial. Heart failure (40 mg, 80 mg and 160 mg) Val-HeFT was a randomized, controlled, multinational clinical trial of valsartan compared with placebo on morbidity and mortality in 5,010 NYHA class II (62%), III (36%) and IV (2%) heart failure patients receiving usual therapy with LVEF <40% and left ventricular internal diastolic diameter (LVIDD) >2.9 cm/m2 . Baseline therapy included ACE inhibitors (93%), diuretics (86%), digoxin (67%) and beta blockers (36%). The mean duration of follow-up was nearly two years. The mean daily dose of Diovan in Val-HeFT was 254 mg. The study had two primary endpoints: all-cause mortality (time to death) and composite mortality and heart failure morbidity (time to first morbid event) defined as death, sudden death with resuscitation, hospitalization for heart failure, or administration of intravenous inotropic or vasodilator drugs for four hours or more without hospitalization. All cause mortality was similar (p=NS) in the valsartan (19.7%) and placebo (19.4%) groups. The primary benefit was a 27.5% (95% CI: 17 to 37%) reduction in risk for time to first heart failure hospitalization (13.9% vs. 18.5%). Results appearing to favour placebo (composite mortality and morbidity was 21.9% in placebo vs. 25.4% in valsartan group) were observed for those patients receiving the triple combination of an ACE inhibitor, a beta blocker and valsartan. In a subgroup of patients not receiving an ACE inhibitor (n=366), the morbidity benefits were greatest. In this subgroup all-cause mortality was significantly reduced with valsartan compared to placebo by 33% (95% CI: –6% to 58%) (17.3% valsartan vs. 27.1% placebo) and the composite mortality and morbidity risk was significantly reduced by 44% (24.9% valsartan vs. 42.5% placebo). In patients receiving an ACE inhibitor without a beta-blocker, all-cause mortality was similar (p=NS) in the valsartan (21.8%) and placebo (22.5%) groups. Composite mortality and morbidity risk was significantly reduced by 18.3% (95% CI: 8% to 28%) with valsartan compared with placebo (31.0% vs. 36.3%). DIO SPI SEP23 V1.3 In the overall Val-HeFT population, valsartan treated patients showed significant improvement in NYHA class, and heart failure signs and symptoms, including dyspnoea, fatigue, oedema and rales compared to placebo. Patients treated with valsartan had a better quality of life as demonstrated by change in the Minnesota Living with Heart Failure Quality of Life score from baseline at endpoint than placebo. Ejection fraction in valsartan treated patients was significantly increased and LVIDD significantly reduced from baseline at endpoint compared to placebo. Other: dual blockade of the renin-angiotensin-aldosterone system (RAAS) Two large randomised, controlled trials (ONTARGET (ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial) and VA NEPHRON-D (The Veterans Affairs Nephropathy in Diabetes)) have examined the use of the combination of an ACE-inhibitor with an angiotensin II receptor blocker. ONTARGET was a study conducted in patients with a history of cardiovascular or cerebrovascular disease, or type 2 diabetes mellitus accompanied by evidence of end-organ damage. VA NEPHRON-D was a study in patients with type 2 diabetes mellitus and diabetic nephropathy. These studies have shown no significant beneficial effect on renal and/or cardiovascular outcomes and mortality, while an increased risk of hyperkalaemia, acute kidney injury and/or hypotension as compared to monotherapy was observed. Given their similar pharmacodynamic properties, these results are also relevant for other ACE inhibitors and angiotensin II receptor blockers.ACE inhibitors and angiotensin II receptor blockers should therefore not be used concomitantly in patients with diabetic nephropathy. ALTITUDE (Aliskiren Trial in Type 2 Diabetes Using Cardiovascular and Renal Disease Endpoints) was a study designed to test the benefit of adding aliskiren to a standard therapy of an ACE inhibitor or an angiotensin II receptor blocker in patients with type 2 diabetes mellitus and chronic kidney disease, cardiovascular disease, or both. The study was terminated early because of an increased risk of adverse outcomes. Cardiovascular death and stroke were both numerically more frequent in the aliskiren group than in the placebo group and adverse events and serious adverse events of interest (hyperkalaemia, hypotension and renal dysfunction) were more frequently reported in the aliskiren group than in the placebo group.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption Following oral administration of valsartan alone, peak plasma concentrations of valsartan are reached in 2-4 hours. Mean absolute bioavailability for Diovan is 23%. Food decreases exposure (as measured by AUC) to valsartan by about 40% and peak plasma concentration (Cmax) by about 50%, although from about 8 h post dosing plasma valsartan concentrations are similar for the fed and fasted groups. This reduction in AUC is not, however, accompanied by a clinically significant reduction in DIO SPI SEP23 V1.3 the therapeutic effect, and valsartan can therefore be given either with or without food. Distribution The steady-state volume of distribution of valsartan after intravenous administration is about 17 litres, indicating that valsartan is not distributed into tissues extensively. Valsartan is highly bound to serum protein (94-97%), mainly serum albumin. Biotransformation Valsartan is not biotransformed to a high extent as only about 20% of dose is recovered as metabolites. A hydroxy metabolite has been identified in plasma at low concentrations (less than 10% of the valsartan AUC). This metabolite is pharmacologically inactive. Elimination Valsartan shows multiexponential decay kinetics (t1/2α < 1h and t1/2β about 9 h). Valsartan is primarily eliminated by biliary excretion in faeces (about 83% of dose) and renally in urine (about 13% of dose), mainly as unchanged drug. Following intravenous administration, plasma clearance of valsartan is about 2 L/h and its renal clearance is 0.62 L/h (about 30% of total clearance). The half-life of valsartan is 6 hours. In heart failure patients (40mg,80 mg, 160mg): The average time to peak concentration and elimination half-life of valsartan in heart failure patients are similar to that observed in healthy volunteers. AUC and Cmax values of valsartan are almost proportional with increasing dose over the clinical dosing range (40 to 160 mg twice a day). The average accumulation factor is about 1.7. The apparent clearance of valsartan following oral administration is approximately 4.5 L/h. Age does not affect the apparent clearance in heart failure patients. Special populations Older people A somewhat higher systemic exposure to valsartan was observed in some elderly subjects than in young subjects; and a lower starting dose (40 mg) is recommended for the elderly. Impaired renal function As expected for a compound where renal clearance accounts for only 30% of total plasma clearance, no correlation was seen between renal function and systemic exposure to valsartan. Dose adjustment is therefore not required in patients with renal impairment (creatinine clearance - >10 ml/min). There is currently no experience on the safe use in patients with a creatinine clearance <10 ml/min and patients undergoing dialysis, therefore valsartan should be used with caution in these patients (see sections 4.2 and 4.4). Valsartan is highly bound to plasma protein and is unlikely to be removed by dialysis. DIO SPI SEP23 V1.3 Hepatic impairment Approximately 70% of the dose absorbed is eliminated in the bile, essentially in the unchanged form. Valsartan does not undergo any noteworthy biotransformation. A doubling of exposure (AUC) was observed in patients with mild to moderate hepatic impairment compared to healthy subjects. However, no correlation was observed between plasma valsartan concentrations versus degree of hepatic dysfunction. Diovan has not been studied in patients with severe hepatic dysfunction (see sections 4.2, 4.3 and 4.4). Impaired renal function Use in paediatric patients with a creatinine clearance <30 ml/min and paediatric patients undergoing dialysis has not been studied, therefore valsartan is not recommended in these patients. No dose adjustment is required for paediatric patients with a creatinine clearance >30 ml/min. Renal function and serum potassium should be closely monitored (see sections 4.2 and 4.4).

פרטי מסגרת הכללה בסל
התרופה האמורה תינתן במקרים האלה: א. חולה הסובל מיתר לחץ דם או אי ספיקת לב הסובל בנוסף מרגישות לטיפול בתכשירים השייכים למשפחת מעכבי ACE או שפיתח תופעות לוואי לטיפול כאמור; ב. לחולה הסובל מפרוטאינוריה מעל 1 גרם, בשילוב עם מעכבי ACE; ג. טיפול בחלבון בשתן מתחת ל-1 גרם ומעל ל-30 מ"ג, עבור חולה שלא סובל מיתר לחץ דם או אי ספיקת לב, הסובל בנוסף מרגישות לטיפול בתכשירים השייכים למשפחת מעכבי ACE או שפיתח תופעות לוואי לטיפול כאמור.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| OLMESARTAN MEDOXOMIL | ||||
| VALSARTAN | ||||
| LOSARTAN | ||||
| IRBESARTAN | ||||
| CANDESARTAN | ||||
| טיפול בחלבון בשתן מתחת ל-1 גרם ומעל ל-30 מ"ג, עבור חולה שלא סובל מיתר לחץ דם או אי ספיקת לב, הסובל בנוסף מרגישות לטיפול בתכשירים השייכים למשפחת מעכבי ACE או שפיתח תופעות לוואי לטיפול כאמור. | ||||
| חולה הסובל מפרוטאינוריה מעל 1 גרם, בשילוב עם מעכבי ACE | ||||
| חולה הסובל מיתר לחץ דם או אי ספיקת לב הסובל בנוסף מרגישות לטיפול בתכשירים השייכים למשפחת מעכבי ACE או שפיתח תופעות לוואי לטיפול |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/03/2002
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
10.11.13 - עלון לצרכן 09.11.20 - עלון לצרכן אנגלית 09.11.20 - עלון לצרכן עברית 09.11.20 - עלון לצרכן ערבית 06.12.22 - עלון לצרכן אנגלית 06.12.22 - עלון לצרכן עברית 06.12.22 - עלון לצרכן ערבית 27.09.23 - עלון לצרכן עברית 01.11.23 - עלון לצרכן אנגלית 01.11.23 - עלון לצרכן ערבית 08.03.12 - החמרה לעלון 16.01.14 - החמרה לעלון 05.03.15 - החמרה לעלון 05.08.20 - החמרה לעלון 11.10.20 - החמרה לעלון 06.12.22 - החמרה לעלון 27.09.23 - החמרה לעלוןלתרופה במאגר משרד הבריאות
דיובאן ® 40 מ"ג טבליות מצופות