Quest for the right Drug
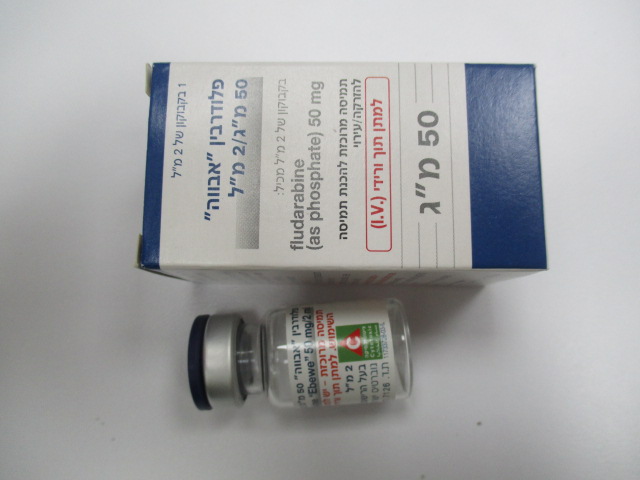
פלודרבין "אבווה" 50 מ"ג/2 מ"ל FLUDARABIN "EBEWE" 50 MG/2 ML (FLUDARABINE PHOSPHATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תרכיז להכנת תמיסה לאינפוזיההזרקה : CONCENTRATE FOR SOLUTION FOR INJECTION / INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Neurotoxicity When used at high doses in dose-ranging studies in patients with acute leukaemia, intravenous fludarabine phosphate was associated with severe neurologic effects including blindness, coma, and death. Symptoms appeared from 21 to 60 days from last dose. This severe central nervous system toxicity occured in 36% of patients treated intravenously with doses approximately four times greater (96 mg/m²/day for 5-7 days) than the recommended dose. In patients treated at doses in the range of the dose recommended for chronic lymphocytic leukaemia, severe central nervous system toxicity occurred rarely (coma, seizures, and agitation) or uncommonly (confusion) (see section 4.8). Patients should be closely observed for signs of neurologic effects. The effect of chronic administration of fludarabine phosphate on the central nervous system is unknown. However, patients tolerated the recommended dose, in some studies for relatively long treatment times (for up to 26 courses of therapy). In postmarketing experience neurotoxicity has been reported to occur earlier or later than in clinical trials. Administration of fludarabine phosphate can be associated with leukoencephalopathy (LE), acute toxic leukoencephalopathy (ATL) or reversible posterior leukoencephalopathy syndrome (RPLS). These may occur: • at the recommended dose o when fludarabine phosphate is given following, or in combination with, medications known to be associated with LE, ATL or RPLS o or when fludarabine phosphate is given in patients with other risk factors such as cranial or total body irradiation, Hematopoietic Cell Transplantation, Graft versus Host Disease, renal impairment, or hepatic encephalopathy. • at doses higher than the recommended dose LE, ATL or RPLS symptoms may include headache, nausea and vomiting, seizures, visual disturbances such as vision loss, altered sensorium, and focal neurological deficits. Additional effects may include optic neuritis, and papillitis, confusion, somnolence, agitation, paraparesis/ quadriparesis, muscle spasticity and incontinence. LE/ ATL/ RPLS may be irreversible, life-threatening, or fatal. Whenever LE, ATL or RPLS is suspected, fludarabine treatment should be stopped. Patients should be monitored and should undergo brain imaging, preferably utilizing MRI. If the diagnosis is confirmed, fludarabine therapy should be permanently discontinued. Impaired state of health In patients with impaired state of health, fludarabine phosphate should be given with caution and after careful risk/benefit consideration. This applies especially for patients with severe impairment of bone marrow function (thrombocytopenia, anaemia, and/or granulocytopenia), immunodeficiency or with a history of opportunistic infection. Renal impairment The total body clearance of the principle plasma metabolite 2-F-ara-A shows a correlation with creatinine clearance, indicating the importance of the renal excretion pathway for the elimination of the compound. Patients with reduced renal function demonstrated an increased total body exposure (AUC of 2F-ara-A). There are limited clinical data available in patients with impairment of renal function (creatinine clearance < 70 ml/min). Fludarabine phosphate must be administered cautiously in patients with renal insufficiency. In patients with moderate impairment of renal function (creatinine clearance between 30 and 70 ml/min), the dose should be reduced by up to 50% and the patient should be monitored closely (see section 4.2). Fludarabine phosphate treatment is contraindicated if creatinine clearance is < 30 ml/min (see section 4.3). Myelosuppression Severe bone marrow suppression, notably anaemia, thrombocytopenia and neutropenia, has been reported in patients treated with fludarabine phosphate. In a Phase I intravenous study in adult solid tumour patients, the median time to nadir counts was 13 days (range: 3-25 days) for granulocytes and 16 days (range: 2-32 days) for platelets. Most patients had haematologic impairment at baseline either as a result of disease or as a result of prior myelosuppressive therapy. Cumulative myelosuppression may be seen. While chemotherapy-induced myelosuppression is often reversible, administration of fludarabine phosphate requires careful haematologic monitoring. Fludarabine phosphate is a potent antineoplastic agent with potentially significant toxic side effects. Patients undergoing therapy should be closely observed for signs of haematologic and non-haematologic toxicity. Periodic assessment of peripheral blood counts is recommended to detect the development of anaemia, neutropenia, and thrombocytopenia. Several instances of trilineage bone marrow hypoplasia or aplasia resulting in pancytopenia, sometimes resulting in death, have been reported in adult patients. The duration of clinically significant cytopenia in the reported cases has ranged from approximately 2 months to approximately 1 year. These episodes have occurred both in previously treated or untreated patients. As with other cytotoxics, caution should be exercised with fludarabine phosphate when further hematopoietic stem cell sampling is considered. Transfusion-associated graft-versus-host disease Transfusion-associated graft-versus-host disease (reaction by the transfused immunocompetent lymphocytes to the host) has been observed after transfusion of non-irradiated blood in fludarabine phosphate treated patients. Fatal outcome as a consequence of this disease has been reported with a high frequency. Therefore, to minimize the risk of transfusion-associated graft-versus-host disease, patients who require blood transfusion and who are undergoing, or who have received, treatment with fludarabine phosphate should receive irradiated blood only. Skin cancer The worsening or flare up of pre-existing skin cancer lesions as well as new onset of skin cancer has been reported in some patients during or after fludarabine phosphate therapy. Tumour lysis syndrome Tumour lysis syndrome has been reported in CLL patients with large tumour burdens. Since fludarabine phosphate can induce a response as early as within the first week of treatment, precautions should be taken in those patients at risk of developing this complication, and hospitalisation may be recommended for these patients during the first course of treatment. Autoimmune disorders Irrespective of any previous history of autoimmune processes or Coombs test status, life-threatening and sometimes fatal autoimmune phenomena (e.g. autoimmune haemolytic anaemia, autoimmune thrombocytopenia, thrombocytopenic purpura, pemphigus, Evans' syndrome) have been reported to occur during or after treatment with fludarabine phosphate. The majority of patients experiencing haemolytic anaemia developed a recurrence in the haemolytic process after rechallenge with fludarabine phosphate. Patients treated with fludarabine phosphate should be closely monitored for signs of haemolysis. Discontinuation of therapy with fludarabine phosphate is recommended in case of haemolysis. Blood transfusions (irradiated, see above) and adrenocorticoid preparations are the most common treatment measures for autoimmune haemolytic anaemia. Older people Since there are limited data for the use of fludarabine phosphate in elderly persons (> 75 years), caution should be exercised with the administration of fludarabine phosphate in these patients (see also section 4.2). In patients aged 65 years or older, creatinine clearance should be measured before start of treatment, see Renal impairment and section 4.2 Pregnancy Fludarabine should not be used during pregnancy unless clearly necessary (e.g. life-threatening situation, no alternative safer treatment available without compromising the therapeutic benefit, treatment cannot be avoided). It has the potential to cause fetal harm (see sections 4.6 and 5.3). Prescribers may only consider the use of fludarabine, if the potential benefits justify the potential risks to the foetus. Women should avoid becoming pregnant while on fludarabine therapy. Women of childbearing potential must be apprised of the potential hazard to the foetus. Contraception Women of child-bearing potential or fertile males must take effective contraceptive measures during and at least for 6 months after cessation of therapy (see section 4.6). Vaccination During and after treatment with fludarabine phosphate vaccination with live vaccines should be avoided. Retreatment options after initial fludarabine treatment A crossover from initial treatment with fludarabine phosphate to chlorambucil for non responders to fludarabine phosphate should be avoided because most patients who have been resistant to fludarabine phosphate have shown resistance to chlorambucil. Fludarabine "Ebewe" 50 mg/2 ml contains sodium This medicinal product contains less than 1 mmol sodium (23 mg) per 45 mg (average dose), that is to say essentially ‘sodium-free.
Effects on Driving
4.7 Effects on ability to drive and use machines Fludarabine phosphate may reduce the ability to drive and use machines, since e.g. fatigue, weakness, visual disturbances, confusion, agitation and seizures have been observed.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים הבאים: א. טיפול תומך בלוקמיה לימפוציטית כרונית (CLL) שאינה מגיבה לטיפול אחר. ב. טיפול התחלתי בלוקמיה לימפוציטית כרונית (CLL) ג. טיפול בלימפומה מסוג Non Hodgkin's שלב 3 עד 4 בחולים שלא הגיבו לטיפול בתכשיר ממשפחת ה-Alkylating agents או בחולים שמחלתם התקדמה במהלך טיפול או לאחריו. ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה רופא מומחה בהמטולוגיה או רופא מומחה בגינקולוגיה המטפל באונקולוגיה גינקולוגית.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| טיפול בלימפומה מסוג Non Hodgkin's שלב 3 עד 4 בחולים שלא הגיבו לטיפול בתכשיר ממשפחת ה-Alkylating agents או בחולים שמחלתם התקדמה במהלך טיפול או לאחריו. | 16/12/1997 | |||
| טיפול התחלתי בלוקמיה לימפוציטית כרונית (CLL) | 16/12/1997 | |||
| טיפול תומך בלוקמיה לימפוציטית כרונית (CLL) שאינה מגיבה לטיפול אחר. | 16/12/1997 |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
16/12/1997
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לרופא
11.10.21 - עלון לרופאעלון מידע לצרכן
11.10.21 - החמרה לעלוןלתרופה במאגר משרד הבריאות
פלודרבין "אבווה" 50 מ"ג/2 מ"ל