Quest for the right Drug
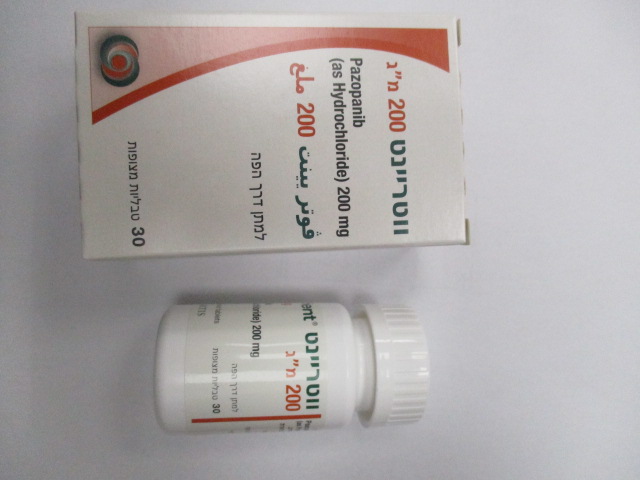
ווטריינט 200 מ"ג VOTRIENT 200 MG (PAZOPANIB AS HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antineoplastic agents, protein kinase inhibitors, other protein kinase inhibitors, ATC code: L01EX03 Mechanism of action Pazopanib is an orally administered, potent multi-target tyrosine kinase inhibitor (TKI) of vascular endothelial growth factor receptors (VEGFR)-1, -2, and -3, platelet-derived growth factor (PDGFR)-α and – β, and stem cell factor receptor (c-KIT), with IC50 values of 10, 30, 47, 71, 84 and 74 nM, respectively. In preclinical experiments, pazopanib dose-dependently inhibited ligand-induced auto-phosphorylation of VEGFR-2, c-Kit and PDGFR-β receptors in cells. In vivo, pazopanib inhibited VEGF-induced VEGFR-2 phosphorylation in mouse lungs, angiogenesis in various animal models, and the growth of multiple human tumour xenografts in mice. Pharmacogenomics In a pharmacogenetic meta-analysis of data from 31 clinical studies of pazopanib administered either as monotherapy or in combination with other agents, ALT >5 x ULN (NCI CTC Grade 3) occurred in 19% of HLA-B*57:01 allele carriers and in 10% of non-carriers. In this dataset, 133/2235 (6%) of the patients VOT SPI Jan22 V3 EU SmPC 12-Nov-2021 carried the HLA-B*57:01 allele (see section 4.4). Clinical studies Renal cell carcinoma (RCC) The safety and efficacy of pazopanib in RCC were evaluated in a randomised, double-blind, placebo- controlled multicentre study. Patients (N = 435) with locally advanced and/or metastatic RCC were randomised to receive pazopanib 800 mg once daily or placebo. The primary objective of the study was to evaluate and compare the two treatment arms for progression-free survival (PFS) and the principle secondary endpoint was overall survival (OS). The other objectives were to evaluate the overall response rate and duration of response. From the total of 435 patients in this study, 233 patients were treatment naïve and 202 were second-line patients who had received one prior IL-2 or INFα-based therapy. The performance status (ECOG) was similar between the pazopanib and placebo groups (ECOG 0: 42% vs. 41%, ECOG 1: 58% vs. 59%). The majority of patients had either favourable (39%) or intermediate (54%), MSKCC (Memorial Sloan Kettering Cancer Centre) / Motzer prognostic factors. All patients had clear cell histology or predominantly clear cell histology. Approximately half of all patients had 3 or more organs involved in their disease and most patients had the lung (74%), and/or lymph nodes (54%) as a metastatic location for disease at baseline. A similar proportion of patients in each arm were treatment-naïve and cytokine pre-treated (53% and 47% in pazopanib arm, 54% and 46% in placebo arm). In the cytokine pre-treated subgroup, the majority (75%) had received interferon-based treatment. Similar proportions of patients in each arm had prior nephrectomy (89% and 88% in the pazopanib and placebo arms, respectively) and/or prior radiotherapy (22% and 15% in the pazopanib and placebo arms, respectively). The primary analysis of the primary endpoint PFS is based on disease assessment by independent radiological review in the entire study population (treatment naïve and cytokine pre-treated). Table 4 Overall efficacy results in RCC by independent assessment (VEG105192) P value Endpoints/Study population Pazopanib Placebo HR (95% CI) (one-sided) PFS Overall* ITT N = 290 N = 145 Median (months) 9.2 4.2 0.46 (0.34, 0.62) <0.0000001 Response rate N = 290 N = 145 % (95% CI) 30 (25.1,35.6) 3 (0.5, 6.4) – <0.001 HR = hazard ratio; ITT = intent to treat; PFS = progression-free survival. * -treatment-naïve and cytokine pre-treated populations. Figure 1 Kaplan-Meier curve for progression-free survival by independent assessment for the VOT SPI Jan22 V3 EU SmPC 12-Nov-2021 overall population (treatment-naïve and cytokine pre-treated populations) (VEG105192) x axis; Months, y axis; Proportion Progression Free, Pazopanib —―— (N = 290) Median 9.2 months; Placebo -------- (N = 145) Median 4.2 months; Hazard Ratio = 0.46, 95% CI (0.34, 0.62), P <0.0000001 VOT SPI Jan22 V3 EU SmPC 12-Nov-2021 Figure 2 Kaplan-Meier curve for progression-free survival by independent assessment for the treatment-naïve population (VEG105192) x axis; Months, y axis; Proportion Progression Free, Pazopanib —―— (N = 155) Median 11.1 months; Placebo -------- (N = 78) Median 2.8 months; Hazard Ratio = 0.40, 95% CI (0.27, 0.60), P <0.0000001 Figure 3 Kaplan-Meier Curve for progression-free survival by independent assessment for the cytokine pre-treated population (VEG105192) x axis; Months, y axis; Proportion Progression Free, Pazopanib —―— (N = 135) Median 7.4 months; Placebo -------- (N = 67) Median 4.2 months; Hazard Ratio = 0.54, 95% CI (0.35, 0.84), P <0.001 For patients who responded to treatment, the median time to response was 11.9 weeks and the median duration of response was 58.7 weeks as per independent review (VEG105192). The median overall survival (OS) data at the protocol-specified final survival analysis were 22.9 months and 20.5 months [HR = 0.91 (95% CI: 0.71, 1.16; p = 0.224)] for patients randomised to the pazopanib and placebo arms, respectively. The OS results are subject to potential bias as 54% of patients in the placebo arm also received pazopanib in the extension part of this study following disease progression. Sixty-six percent of placebo patients received post-study therapy compared to 30% of pazopanib patients. No statistical differences were observed between treatment groups for Global Quality of Life using EORTC QLQ-C30 and EuroQoL EQ-5D. In a Phase II study of 225 patients with locally recurrent or metastatic clear cell renal cell carcinoma, objective response rate was 35 % and median duration of response was 68 weeks, as per independent review. Median PFS was 11.9 months. VOT SPI Jan22 V3 EU SmPC 12-Nov-2021 The safety, efficacy and quality of life of pazopanib versus sunitinib was evaluated in a randomised, open- label, parallel group Phase III non-inferiority study (VEG108844). In VEG108844, patients (N = 1110) with locally advanced and/or metastatic RCC who had not received prior systemic therapy, were randomised to receive either pazopanib 800 mg once daily continuously or sunitinib 50 mg once daily in 6-week cycles of dosing with 4 weeks on treatment followed by 2 weeks without treatment. The primary objective of this study was to evaluate and compare PFS in patients treated with pazopanib to those treated with sunitinib. Demographic characteristics were similar between the treatment arms. Disease characteristics at initial diagnosis and at screening were balanced between the treatment arms with the majority of patients having clear cell histology and Stage IV disease. VEG108844 achieved its primary endpoint of PFS and demonstrated that pazopanib was non-inferior to sunitinib, as the upper bound of the 95% CI for the hazard ratio was less than the protocol-specified non- inferiority margin of 1.25. Overall efficacy results are summarised in Table 5. Table 5 Overall efficacy results (VEG108844) Pazopanib Sunitinib HR Endpoint N = 557 N = 553 (95% CI) PFS Overall Median (months) 8.4 9.5 1.047 (95% CI) (8.3, 10.9) (8.3, 11.0) (0.898, 1.220) Overall Survival Median (months) 28.3 29.1 0.915a (95% CI) (26.0, 35.5) (25.4, 33.1) (0.786, 1.065) HR = hazard ratio; PFS = progression-free survival; a P value = 0.245 (2-sided) VOT SPI Jan22 V3 EU SmPC 12-Nov-2021 Figure 4 Kaplan-Meier Curve for progression-free survival by independent assessment for the overall population (VEG108844) Subgroup analyses of PFS were performed for 20 demographic and prognostic factors. The 95% confidence intervals for all subgroups include a hazard ratio of 1. In the three smallest of these 20 subgroups, the point estimate of the hazard ratio exceeded 1.25; i.e. in subjects with no prior nephrectomy (n=186, HR=1.403, 95% CI (0.955, 2.061)), baseline LDH >1.5 x ULN (n=68, HR=1.72, 95% CI (0.943, 3.139)), and MSKCC: poor risk (n=119, HR=1.472, 95% CI (0.937, 2.313)). Soft-tissue sarcoma (STS) The efficacy and safety of pazopanib in STS were evaluated in a pivotal Phase III randomised, double-blind, placebo-controlled multicentre study (VEG110727). A total of 369 patients with advanced STS were randomised to receive pazopanib 800 mg once daily or placebo. Importantly, only patients with selective histological subtypes of STS were allowed to participate to the study, therefore efficacy and safety of pazopanib can only be considered established for those subgroups of STS and treatment with pazopanib should be restricted to such STS subtypes. The following tumour types were eligible: Fibroblastic (adult fibrosarcoma, myxofibrosarcoma, sclerosing epithelioid fibrosarcoma, malignant solitary fibrous tumours), so-called fibrohistiocytic (pleomorphic malignant fibrous histiocytoma [MFH], giant cell MFH, inflammatory MFH), leiomyosarcoma, malignant glomus tumours, skeletal muscles (pleomorphic and alveolar rhabdomyosarcoma), vascular (epithelioid hemangioendothelioma, angiosarcoma), uncertain differentiation (synovial, epithelioid, alveolar soft part, clear cell, desmoplastic small round cell, extra-renal rhabdoid, malignant mesenchymoma, PEComa, intimal sarcoma), malignant peripheral nerve sheath tumours, undifferentiated soft tissue sarcomas not otherwise specified (NOS) and other types of sarcoma (not listed as ineligible). The following tumour types were not eligible: Adipocytic sarcoma (all subtypes), all rhabdomyosarcoma that were not alveolar or pleomorphic, chondrosarcoma, osteosarcoma, Ewing tumours/primitive neuroectodermal tumours (PNET), GIST, dermofibromatosis sarcoma protuberans, inflammatory myofibroblastic sarcoma, malignant mesothelioma and mixed mesodermal tumours of the uterus. Of note, patients with adipocytic sarcoma were excluded from the pivotal Phase III study as in a preliminary Phase II study (VEG20002) activity (PFS at week 12) observed with pazopanib in adipocytic did not meet the prerequisite rate to allow further clinical testing. VOT SPI Jan22 V3 EU SmPC 12-Nov-2021 Other key eligibility criteria of the VEG110727 study were: histological evidence of high or intermediate grade malignant STS and disease progression within 6 months of therapy for metastatic disease, or recurrence within 12 months of (neo) -/adjuvant therapy. Ninety-eight percent (98%) of subjects received prior doxorubicin, 70% prior ifosfamide, and 65% of subjects had received at least three or more chemotherapeutic agents prior to study enrolment. Patients were stratified by the factors of WHO performance status (WHO PS) (0 or 1) at baseline and the number of lines of prior systemic therapy for advanced disease (0 or 1 vs. 2+). In each treatment group, there was a slightly greater percentage of subjects in the 2+ lines of prior systemic therapy for advanced disease (58% and 55%, respectively, for placebo and pazopanib treatment arms) compared with 0 or 1 lines of prior systemic therapy (42% and 45%, respectively, for placebo and pazopanib treatment arms). The median duration of follow-up of subjects (defined as date of randomisation to date of last contact or death) was similar for both treatment arms (9.36 months for placebo [range 0.69 to 23.0 months] and 10.04 months for pazopanib [range 0.2 to 24.3 months]. The primary objective of the study was progression-free survival (PFS assessed by independent radiological review); the secondary endpoints included overall survival (OS), overall response rate and duration of response. VOT SPI Jan22 V3 EU SmPC 12-Nov-2021 Table 6 Overall efficacy results in STS by independent assessment (VEG110727) Endpoints/ study population Pazopanib Placebo HR (95% CI) P value (two-sided) PFS Overall ITT N = 246 N = 123 Median (weeks) 20.0 7.0 0.35 (0.26, 0.48) <0.001 Leiomyosarcoma N = 109 N = 49 Median (weeks) 20.1 8.1 0.37 (0.23, 0.60) <0.001 Synovial sarcoma subgroups N = 25 N = 13 Median (weeks) 17.9 4.1 0.43 (0.19, 0.98) 0.005 ‘Other STS’ subgroups N = 112 N = 61 Median (weeks) 20.1 4.3 0.39 (0.25, 0.60) <0.001 OS Overall ITT N = 246 N = 123 Median (months) 12.6 10.7 0.87 (0.67,1.12) 0.256 Leiomyosarcoma* N = 109 N = 49 Median (months) 16.7 14.1 0.84 (0.56, 1.26 0.363 Synovial sarcoma subgroups* N = 25 N = 13 Median (months) 8.7 21.6 1.62 (0.79, 3.33) 0.115 "Other STS" subgroups* N = 112 N = 61 Median (months) 10.3 9.5 0.84 (0.59, 1.21) 0.325 Response rate (CR+PR) % (95% CI) 4 (2.3, 7.9) 0 (0.0, 3.0) Duration of response Median (weeks) (95% CI) 38.9 (16.7, 40.0) HR = hazard ratio; ITT = intent to treat; PFS = progression-free survival; CR = complete response; PR = partial response. OS = overall survival * Overall survival for the respective STS histological subgroups (leiomyosarcoma, synovial sarcoma and “Other” STS) should be interpreted with caution due to the small number of subjects and wide confidence intervals A similar improvement in PFS based on investigator assessments was observed in the pazopanib arm compared with the placebo arm (in the overall ITT population HR: 0.39; 95% CI, 0.30 to 0.52, p <0.001). VOT SPI Jan22 V3 EU SmPC 12-Nov-2021 Figure 5 Kaplan-Meier Curve for Progression-Free Survival in STS by Independent Assessment for the Overall Population (VEG110727) No significant difference in OS was observed between the two treatment arms at the final OS analysis performed after 76% (280/369) of the events had occurred (HR 0.87, 95% CI 0.67, 1.12 p=0.256).
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption Upon oral administration of a single pazopanib 800 mg dose to patients with solid tumours, maximum plasma concentration (Cmax) of approximately 19 ± 13 µg/ml was obtained after median 3.5 hours (range 1.0- 11.9 hours) and an AUC0-∞ of approximately 650 ± 500 µg.h/ml was obtained. Daily dosing results in 1.23- to 4-fold increase in AUC0-T. There was no consistent increase in AUC or Cmax at pazopanib doses above 800 mg. Systemic exposure to pazopanib is increased when administered with food. Administration of pazopanib with a high-fat or low-fat meal results in an approximately 2-fold increase in AUC and Cmax. Therefore, pazopanib should be administered at least two hours after food or at least one hour before food (see section 4.2). Administration of a pazopanib 400 mg crushed tablet increased AUC(0-72) by 46% and Cmax by approximately 2 fold and decreased tmax by approximately 2 hours compared to administration of the whole tablet. These results indicate that the bioavailability and the rate of pazopanib oral absorption are increased after administration of the crushed tablet relative to administration of the whole tablet (see section 4.2). Distribution Binding of pazopanib to human plasma protein in vivo was greater than 99% with no concentration dependence over the range of 10-100 µg/ml. In vitro studies suggest that pazopanib is a substrate for P-gp and BCRP. Biotransformation Results from in vitro studies demonstrated that metabolism of pazopanib is mediated primarily by CYP3A4, with minor contributions from CYP1A2 and CYP2C8. The four principle pazopanib metabolites account for only 6% of the exposure in plasma. One of these metabolites inhibits the proliferation of VEGF-stimulated human umbilical vein endothelial cells with a similar potency to that of pazopanib, the others are 10- to 20- VOT SPI Jan22 V3 EU SmPC 12-Nov-2021 fold less active. Therefore, activity of pazopanib is mainly dependent on parent pazopanib exposure. Elimination Pazopanib is eliminated slowly with a mean half-life of 30.9 hours after administration of the recommended dose of 800 mg. Elimination is primarily via faeces with renal elimination accounting for <4% of the administered dose. Special populations Renal impairment Results indicate that less than 4% of an orally administered pazopanib dose is excreted in the urine as pazopanib and metabolites. Results from population pharmacokinetic modelling (data from subjects with baseline CLCR values ranging from 30.8 ml/min to 150 ml/min) indicated that renal impairment is unlikely to have clinically relevant effect on pazopanib pharmacokinetics. No dose adjustment is required in patients with creatinine clearance above 30 ml/min. Caution is advised in patients with creatinine clearance below 30 ml/min as there is no experience of pazopanib in this patient population (see section 4.2). Hepatic impairment Mild The median steady-state pazopanib Cmax and AUC(0-24) in patients with mild abnormalities in hepatic parameters (defined as either normal bilirubin and any degree of ALT elevation or as an elevation of bilirubin up to 1.5 x ULN regardless of the ALT value) after administration of 800 mg once daily are similar to the median in patients with normal hepatic function (see Table 7). 800 mg pazopanib once daily is the recommended dose in patients with mild abnormalities of serum liver tests (see section 4.2). Moderate The maximally tolerated pazopanib dose (MTD) in patients with moderate hepatic impairment (defined as an elevation of bilirubin >1.5 x to 3 x ULN regardless of the ALT values) was 200 mg once daily. The median steady-state Cmax and AUC(0-24) values after administration of 200 mg pazopanib once daily in patients with moderate hepatic impairment were approximately 44% and 39%, of the corresponding median values after administration of 800 mg once daily in patients with normal hepatic function, respectively (see Table 7). Based on safety and tolerability data, the dose of pazopanib should be reduced to 200 mg once daily in subjects with moderate hepatic impairment (see section 4.2). Severe The median steady-state Cmax and AUC(0-24) values after administration of 200 mg pazopanib once daily in patients with severe hepatic impairment were approximately 18% and 15%, of the corresponding median values after administration of 800 mg once daily in patients with normal hepatic function. Based on the diminished exposure and limited hepatic reserve pazopanib is not recommended in patients with severe hepatic impairment (defined as total bilirubin >3 X ULN regardless of any level of ALT) (see section 4.2). Table 7 Median steady-state pazopanib pharmacokinetics measured in subjects with hepatic impairment. Group Investigated Cmax (µg/ml) AUC (0-24) Recommended dose (µg x hr/ml) dose Normal hepatic 800 mg OD 52.0 888.2 800 mg OD function (17.1-85.7) (345.5-1482) Mild HI 800 mg OD 33.5 774.2 800 mg OD (11.3-104.2) (214.7-2034.4) Moderate HI 200 mg OD 22.2 256.8 200 mg OD (4.2-32.9) (65.7-487.7) Severe HI 200 mg OD 9.4 130.6 Not recommended (2.4-24.3) (46.9-473.2) OD – once daily VOT SPI Jan22 V3 EU SmPC 12-Nov-2021

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. סרטן כליה מתקדם או גרורתי (גם כקו טיפול ראשון). 2. קו טיפול מתקדם (שני והלאה) בסרקומה מתקדמת של הרקמות הרכות מסוג סרקומה פיברובלסטית, סרקומה פיברוהיסטיוציטית, ליומיוסרקומה, סרקומה סינוביאלית, MPNST, NOS, סרקומה וסקולארית, malignant glomus tumors ב. מתן התרופה האמורה ייעשה לפי מרשם של רופא מומחה באונקולוגיה או מומחה באורולוגיה המטפל באורולוגיה אונקולוגית.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| קו טיפול מתקדם (שני והלאה) בסרקומה מתקדמת של הרקמות הרכות מסוג סרקומה פיברובלסטית, סרקומה פיברוהיסטיוציטית, ליומיוסרקומה, סרקומה סינוביאלית, MPNST, NOS, סרקומה וסקולארית, malignant glomus tumors | 09/01/2013 | אונקולוגיה | Soft tissue sarcoma | |
| לטיפול בסרטן כליה מתקדם או גרורתי (גם כקו טיפול ראשון). במהלך מחלתו יהיה החולה זכאי לטיפול בשתי תרופות בלבד מהתרופות המפורטות להלן - Sunitinib, Sorafenib, Everolimus, Temsirolimus, Pazopanib | 23/01/2011 | אונקולוגיה | Renal cell carcinoma | |
| סרטן כליה מתקדם או גרורתי (גם כקו טיפול ראשון). | 30/01/2020 | אונקולוגיה | Renal cell carcinoma | |
| סרטן כליה מתקדם או גרורתי (גם כקו טיפול ראשון). במהלך מחלתו יהיה החולה זכאי לטיפול בשלוש תרופות בלבד מהתרופות המפורטות להלן - Sunitinib, Sorafenib, Everolimus, Temsirolimus, Pazopanib, Axitinib, Nivolumab. הטיפול בתכשיר לא יינתן בשילוב עם Nivolumab או עם תרופה ממשפחת מעכבי mTOR. | 12/01/2017 | אונקולוגיה | Renal cell carcinoma |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
23/01/2011
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לרופא
15.03.22 - עלון לרופאעלון מידע לצרכן
08.05.16 - עלון לצרכן 20.04.22 - עלון לצרכן אנגלית 20.04.22 - עלון לצרכן עברית 20.04.22 - עלון לצרכן ערבית 18.07.23 - עלון לצרכן עברית 07.09.23 - עלון לצרכן אנגלית 07.09.23 - עלון לצרכן ערבית 27.09.24 - עלון לצרכן אנגלית 27.09.24 - עלון לצרכן עברית 27.09.24 - עלון לצרכן ערבית 18.11.12 - החמרה לעלון 21.08.13 - החמרה לעלון 26.03.14 - החמרה לעלון 29.03.15 - החמרה לעלון 06.07.15 - החמרה לעלון 02.03.16 - החמרה לעלון 15.03.17 - החמרה לעלון 27.02.20 - החמרה לעלון 20.08.20 - החמרה לעלון 01.11.21 - החמרה לעלון 16.12.21 - החמרה לעלון 15.03.22 - החמרה לעלון 18.07.23 - החמרה לעלון 27.09.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
ווטריינט 200 מ"ג