Quest for the right Drug
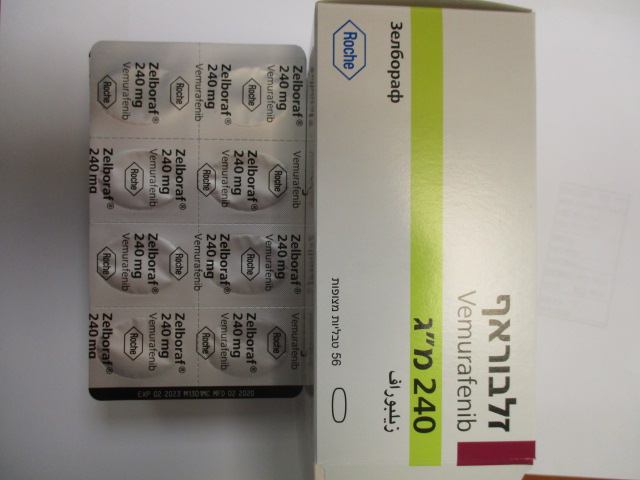
זלבוראף ZELBORAF (VEMURAFENIB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Summary of the safety profile The most common adverse drug reactions (ADR) of any grade (> 30%) reported with vemurafenib include arthralgia, fatigue, rash, photosensitivity reaction, alopecia, nausea diarrhea, headache, pruritus, vomiting, skin papilloma and hyperkeratosis. The most common (≥ 5%) Grade 3 ADRs were cuSCC, keratoacanthoma, rash, arthralgia and gamma-glutamyltransferase (GGT) increased. CuSCC was most commonly treated by local excision. Tabulated summary of adverse reactions ADRs which were reported in melanoma patients are listed below by MedDRA body system organ class, frequency and grade of severity. The following convention has been used for the classification of frequency: Very common ≥ 1/10 Common ≥ 1/100 to < 1/10 Uncommon ≥ 1/1,000 to < 1/100 Rare ≥ 1/10,000 to < 1/1,000 Very rare < 1/10,000 In this section, ADRs are based on results in 468 patients from a phase III randomised open label study in adult patients with BRAF V600 mutation-positive unresectable or stage IV melanoma, as well as a phase II single-arm study in patients with BRAF V600 mutation-positive stage IV melanoma who had previously failed at least one prior systemic therapy (see section 5.1). In addition ADRs originating from safety reports across all clinical trials and post-marketing sources are reported. All terms included are based on the highest percentage observed among phase II and phase III clinical trials. Within each frequency grouping, ADRs are presented in order of decreasing severity and were reported using NCI-CTCAE v 4.0 (common toxicity criteria) for assessment of toxicity. Table 3: ADRs occurring in patients treated with vemurafenib in the phase II or phase III study and events originating from safety reports across all trials(1) and post-marketing sources(2). System organ class Very Common Common Uncommon Rare Infections and Folliculitis infestations Neoplasms benign, SCC of the skin (d), Basal cell carcinoma, Non-cuSCC(1)(3) Chronic malignant and keratoacanthoma, new primary myelomonocytic unspecified seborrhoeic keratosis, melanoma(3) leukaemia(2)(4), (including cysts and skin papilloma pancreatic polyps) adenocarcinoma(5) Blood and lymphatic Neutropenia system disorders thrombocytopenia(6) Immune System Sarcoidosis (1)(2)(j) Disorders Metabolism and Decreased appetite nutrition disorders Nervous system Headache, dysgeusia, 7th nerve paralysis, disorders dizziness neuropathy peripheral Eye disorders Uveitis, Retinal vein occlusion, iridocyclitis Vascular disorders Vasculitis Respiratory, thoracic Cough and mediastinal disorders Gastrointestinal Diarrhoea, vomiting, Stomatitis Pancreatitis(2) disorders nausea, constipation Hepatobiliary Liver injury(1)(2) (g) disorders Skin and Photosensitivity Rash papular, Toxic epidermal Drug reaction with subcutaneous tissue reaction, actinic panniculitis necrolysis (e), Stevens- eosinophilia and disorders keratosis, rash, rash (including erythema Johnson syndrome (f) systemic maculo-papular, nodosum), keratosis symptoms(1)(2) pruritus, pilaris hyperkeratosis, erythema, palmar- plantar erythrodysaesthesia syndrome, alopecia, dry skin, sunburn Musculoskeletal and Arthralgia, myalgia, Arthritis, Plantar fascial connective tissue pain in extremity, fibromatosis(1)(2) disorders musculoskeletal pain, Dupuytren’s back pain contracture(1)(2) System organ class Very Common Common Uncommon Rare Renal and urinary Acute interstitial disorders nephritis(1)(2) (h), acute tubular necrosis(1)(2) (h) General disorders Fatigue, pyrexia, and administration oedema peripheral, site conditions asthenia Investigations ALT increased (c), alkaline phosphatase increased (c), AST increased (c),bilirubin increased (c) GGT increased (c, weight decreased, electrocardiogram QT prolonged, blood creatinine increased(1)(2) (h) Injury, Poisoning, Potentiation of and Procedural Radiation toxicity (1) (2) (i) Complications (1) Events originating from safety reports across all trials (2) Events originating from post-marketing sources. (3) A causal relationship between the medicinal product and the adverse event is at least a reasonable possibility. (4) Progression of pre-existing chronic myelomonocytic leukaemia with NRAS mutation. (5) Progression of pre-existing pancreatic adenocarcinoma with KRAS mutation. (6) Calculated based on phase II and phase III studies. Description of selected adverse reactions Hepatic enzyme increase (c) Liver enzyme abnormalities reported in the phase III clinical study are expressed below as the proportion of patients who experienced a shift from baseline to a grade 3 or 4 liver enzyme abnormalities: • Very common: GGT • Common: ALT, alkaline phosphatase, bilirubin • Uncommon: AST There were no increases to Grade 4 ALT, alkaline phosphatase or bilirubin. Liver injury (g) Based on the criteria for drug induced liver injury developed by an international expert working group of clinicians and scientists, liver injury was defined as any one of the following laboratory abnormalities: • ≥ 5x ULN ALT • ≥ 2x ULN ALP (without other cause for ALP elevation) • ≥ 3x ULN ALT with simultaneous elevation of bilirubin concentration > 2x ULN Cutaneous squamous cell carcinoma (d) (cuSCC) Cases of cuSCC have been reported in patients treated with vemurafenib. The incidence of cuSCC in vemurafenib-treated patients across studies was approximately 20%. The majority of the excised lesions reviewed by an independent central dermatopathology laboratory were classified as SCC- keratoacanthoma subtype or with mixed-keratoacanthoma features (52%). Most lesions classified as “other” (43%) were benign skin lesions (e.g. verruca vulgaris, actinic keratosis, benign keratosis, cyst/benign cyst). CuSCC usually occurred early in the course of treatment with a median time to the first appearance of 7 to 8 weeks. Of the patients who experienced cuSCC, approximately 33% experienced > 1 occurrence with median time between occurrences of 6 weeks. Cases of cuSCC were typically managed with simple excision, and patients generally continued on treatment without dose modification (see sections 4.2 and 4.4). Non-cutaneous squamous cell carcinoma (non-cuSCC) Cases of non-cuSCC have been reported in patients receiving vemurafenib while enrolled in clinical trials. Surveillance for non-cuSCC should occur as outlined in section 4.4. New primary melanoma New primary melanomas have been reported in clinical trials. These cases were managed with excision, and patients continued treatment without dose adjustment. Monitoring for skin lesions should occur as outlined in section 4.4. Potentiation of radiation toxicity(i) Cases reported include recall phenomenon, radiation skin injury, radiation pneumonitis, radiation esophagitis, radiation proctitis, radiation hepatitis, cystitis radiation, and radiation necrosis. In a phase III clinical trial (MO25515, N= 3219), a higher incidence of potentiation of radiation toxicity was reported when vemurafenib patients received radiation prior to and during vemurafenib therapy (9.1%) compared to those patients who received radiation and vemurafenib concomitantly (5.2 %) or to those whose radiation treatment was prior to vemurafenib (1.5%). Hypersensitivity reactions (e) Serious hypersensitivity reactions, including anaphylaxis have been reported in association with vemurafenib. Severe hypersensitivity reactions may include Stevens-Johnson syndrome, generalised rash, erythema or hypotension. In patients who experience severe hypersensitivity reactions, vemurafenib treatment should be permanently discontinued (see section 4.4). Dermatologic reactions (f) Severe dermatologic reactions have been reported in patients receiving vemurafenib, including rare cases of Stevens-Johnson syndrome and toxic epidermal necrolysis in the pivotal clinical trial. In patients who experience a severe dermatologic reaction, vemurafenib treatment should be permanently discontinued. QT prolongation Analysis of centralised ECG data from an open-label uncontrolled phase II QT sub-study in 132 patients dosed with vemurafenib 960 mg twice daily (NP22657) showed an exposure-dependent QTc prolongation. The mean QTc effect remained stable between 12-15 ms beyond the first month of treatment, with the largest mean QTc prolongation (15.1 ms; upper 95% CI: 17.7 ms) observed within the first 6 months (n=90 patients). Two patients (1.5%) developed treatment-emergent absolute QTc values >500 ms (CTC Grade 3), and only one patient (0.8%) exhibited a QTc change from baseline of >60 ms (see section 4.4). Acute kidney injury (h) Cases of renal toxicity have been reported with vemurafenib ranging from creatinine elevations to acute interstitial nephritis and acute tubular necrosis, some observed in the setting of dehydration events. Serum creatinine elevations were mostly mild (>1-1.5x ULN) to moderate (>1.5-3x ULN) and observed to be reversible in nature (see table 4). Table 4: Creatinine changes from baseline in the phase III study Vemurafenib (%) Dacarbazine (%) Change 1 grade from baseline to any grade 27.9 6.1 Change 1 grade from baseline to grade 3 or higher 1.2 1.1 • To grade 3 0.3 0.4 • To grade 4 0.9 0.8 Table 5: Acute kidney injury cases in the phase III study Vemurafenib (%) Dacarbazine (%) Acute kidney injury cases* 10.0 1.4 Acute kidney injury cases associated with 5.5 1.0 dehydration events Dose modified for acute kidney injury 2.1 0 All percentages are expressed as cases out of total patients exposed to each medicinal product. * Includes acute kidney injury, renal impairment, and laboratory changes consistent with acute kidney injury. Sarcoidosis (j) Cases of sarcoidosis have been reported in patients treated with vemurafenib, mostly involving the skin, lung and eye. In majority of the cases, vemurafenib was maintained and the event of sarcoidosis either resolved or persisted. Special populations Elderly In the phase III study, ninety-four (28%) of 336 patients with unresectable or metastatic melanoma treated with vemurafenib were ≥ 65 years. Older patients (≥ 65 years) may be more likely to experience adverse reactions, including cuSCC, decreased appetite, and cardiac disorders. Gender During clinical trials with vemurafenib, grade 3 adverse reactions reported more frequently in females than males were rash, arthralgia and photosensitivity. Paediatric population The safety of vemurafenib in children and adolescents has not been established. No new safety signals were observed in a clinical study with six adolescent patients. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form /https://sideeffects.health.gov.il

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול בחולי מלנומה מתקדמת (גרורתית או שאיננה נתיחה) המבטאים מוטציה ב-BRAF. ב. במהלך מחלתו יהיה החולה זכאי לטיפול בתרופה אחת בלבד מהתרופות המפורטות להלן – Encorafenib, Dabrafenib, Vemurafenibלעניין זה מלנומה בשלב מתקדם (לא נתיח או גרורתי) לא תוגדר כאותה מחלה כמו מלנומה בשלב בר הסרה בניתוח.ג. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| התרופה תינתן לטיפול בחולי מלנומה מתקדמת (גרורתית או שאיננה נתיחה) המבטאים מוטציה ב-BRAF. |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
10/01/2012
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
21.08.14 - עלון לצרכן 22.04.18 - עלון לצרכן 01.05.18 - עלון לצרכן 11.02.20 - עלון לצרכן אנגלית 11.02.20 - עלון לצרכן עברית 11.02.20 - עלון לצרכן ערבית 08.08.23 - עלון לצרכן עברית 11.09.23 - עלון לצרכן אנגלית 11.09.23 - עלון לצרכן ערבית 09.04.24 - עלון לצרכן עברית 23.05.24 - עלון לצרכן אנגלית 23.05.24 - עלון לצרכן ערבית 30.05.13 - החמרה לעלון 18.07.13 - החמרה לעלון 12.02.14 - החמרה לעלון 20.03.14 - החמרה לעלון 19.10.15 - החמרה לעלון 13.12.15 - החמרה לעלון 13.07.16 - החמרה לעלון 24.05.17 - החמרה לעלון 15.11.18 - החמרה לעלון 09.01.20 - החמרה לעלון 08.08.23 - החמרה לעלון 09.04.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
זלבוראף