Quest for the right Drug
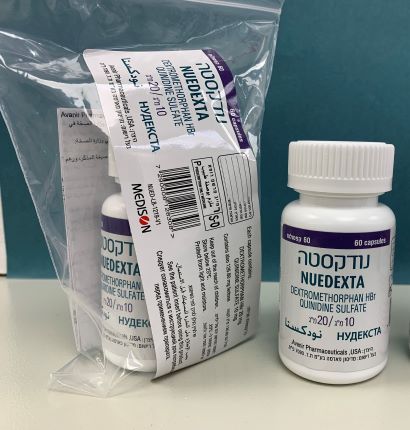
נודקסטה NUEDEXTA (DEXTROMETHORPHAN HYDROBROMIDE, QUINIDINE SULFATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
קפסולות : CAPSULES
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
5 WARNINGS AND PRECAUTIONS 5.1 Thrombocytopenia and Other Hypersensitivity Reactions Quinidine can cause immune-mediated thrombocytopenia that can be severe or fatal. Non-specific symptoms, such as lightheadedness, chills, fever, nausea, and vomiting, can precede or occur with thrombocytopenia. NUEDEXTA should be discontinued immediately if thrombocytopenia occurs, unless the thrombocytopenia is clearly not drug-related, as continued use increases the risk for fatal hemorrhage. Likewise, NUEDEXTA should not be restarted in sensitized patients, because more rapid and more severe thrombocytopenia than the original episode can occur. NUEDEXTA should not be used if immune-mediated thrombocytopenia from structurally related drugs, including quinine and mefloquine is suspected, as cross-sensitivity can occur. Quinidine-associated thrombocytopenia usually, but not always, resolves within a few days of discontinuation of the sensitizing drug. Quinidine has also been associated with a lupus-like syndrome involving polyarthritis, sometimes with a positive antinuclear antibody test. Other associations include rash, bronchospasm, lymphadenopathy, hemolytic anemia, vasculitis, uveitis, angioedema, agranulocytosis, the sicca syndrome, myalgia, elevation in serum levels of skeletal-muscle enzymes, and pneumonitis. 5.2 Hepatotoxicity Hepatitis, including granulomatous hepatitis, has been reported in patients receiving quinidine, generally during the first few weeks of therapy. Fever may be a presenting symptom, and thrombocytopenia or other signs of hypersensitivity may also occur. Most cases remit when quinidine is withdrawn. 5.3 Cardiac Effects NUEDEXTA causes dose-dependent QTc prolongation [see Clinical Pharmacology (12.2)]. QT prolongation can cause torsades de pointes-type ventricular tachycardia, with the risk increasing as the degree of prolongation increases. When initiating NUEDEXTA in patients at risk of QT prolongation and torsades de pointes, electrocardiographic (ECG) evaluation of QT interval should be conducted at baseline and 3-4 hours after the first dose. This includes patients concomitantly taking/initiating drugs that prolong the QT interval or that are strong or moderate CYP3A4 inhibitors, and patients with left ventricular hypertrophy (LVH) or left ventricular dysfunction (LVD). LVH and LVD are more likely to be present in patients with chronic hypertension, known coronary artery disease, or history of stroke. LVH and LVD can be diagnosed utilizing echocardiography or another suitable cardiac imaging modality. Strong and moderate CYP3A inhibitors include, but are not limited to, atazanavir, clarithromycin, indinavir, itraconazole, ketoconazole, nefazodone, nelfinavir, ritonavir, saquinavir, telithromycin, amprenavir, aprepitant, diltiazem, erythromycin, fluconazole, fosamprenavir, grapefruit juice, and verapamil. Reevaluate ECG if risk factors for arrhythmia change during the course of treatment with NUEDEXTA. Risk factors include concomitant use of drugs associated with QT prolongation, electrolyte abnormality (hypokalemia, hypomagnesemia), bradycardia, and family history of QT abnormality. Hypokalemia and hypomagnesemia should be corrected prior to initiation of therapy with NUEDEXTA, and should be monitored during treatment. If patients taking NUEDEXTA experience symptoms that could indicate the occurrence of cardiac arrhythmias, e.g., syncope or palpitations, NUEDEXTA should be discontinued and the patient further evaluated. 5.4 Concomitant use of CYP2D6 Substrates The quinidine in NUEDEXTA inhibits CYP2D6 in patients in whom CYP2D6 is not otherwise genetically absent or its activity otherwise pharmacologically inhibited [see Warnings and Precautions (5.8) and Clinical Pharmacology (12.3), (12.5)]. Because of this effect on CYP2D6, accumulation of parent drug and/or failure of active metabolite formation may decrease the safety and/or the efficacy of drugs used concomitantly with NUEDEXTA that are metabolized by CYP2D6 [see Drug Interactions (7.5)]. 5.5 Dizziness NUEDEXTA may cause dizziness [see Adverse Reactions (6.1)]. Precautions to reduce the risk of falls should be taken, particularly for patients with motor impairment affecting gait or a history of falls. In a controlled trial of NUEDEXTA, 10% of patients on NUEDEXTA and 5% on placebo experienced dizziness. 5.6 Serotonin Syndrome When used with SSRIs (such as fluoxetine) or tricyclic antidepressants (such as clomipramine and imipramine), NUEDEXTA may cause “serotonin syndrome”, with changes including altered mental status, hypertension, restlessness, myoclonus, hyperthermia, hyperreflexia, diaphoresis, shivering, and tremor [see Drug Interactions (7.4), Overdosage (10)]. 5.7 Anticholinergic Effects of Quinidine Monitor for worsening clinical condition in myasthenia gravis and other conditions that may be adversely affected by anticholinergic effects. 5.8 CYP2D6 Poor Metabolizers The quinidine component of NUEDEXTA is intended to inhibit CYP2D6 so that higher exposure to dextromethorphan can be achieved compared to when dextromethorphan is given alone [see Warnings and Precautions (5.4) and Clinical Pharmacology (12.3), (12.5)]. Approximately 7-10% of Caucasians and 3-8% of African Americans lack the capacity to metabolize CYP2D6 substrates and are classified as poor metabolizers (PMs). The quinidine component of NUEDEXTA is not expected to contribute to the effectiveness of NUEDEXTA in PMs, but adverse events of the quinidine are still possible. In those patients who may be at risk of significant toxicity due to quinidine, genotyping to determine if they are PMs should be considered prior to making the decision to treat with NUEDEXTA. 6 ADVERSE REACTIONS A total of 946 patients participated in four Phase 3 controlled and uncontrolled PBA studies and received at least one dose of the combination product of dextromethorphan/quinidine in various strengths at the recommended or higher than the recommended dose. Of those patients, 393 patients were exposed for at least 180 days and 294 patients were exposed for at least one year. Median exposure was 168 days. Controlled trials enrolled only patients with either ALS or MS. Uncontrolled studies enrolled 136 patients with PBA secondary to a wide variety of underlying neurological conditions including stroke (45 patients) and traumatic brain injury (23 patients). Consequently, patients with other underlying neurologic diseases may experience other adverse reactions not described below. 6.1 Clinical Trials Experience A 12-week, placebo-controlled study evaluated NUEDEXTA (dextromethorphan 20 mg/quinidine 10 mg) (N=107) and a 30 mg dextromethorphan/10 mg quinidine combination (N=110) compared to placebo (N=109). Approximately 60% of patients had ALS and 40% had MS. Patients were 25 to 80 years of age, with a mean age of approximately 51 years. Three (3) ALS patients in each drug treatment arm and 1 ALS patient in the placebo arm died during the 12-week placebo-control period. All deaths were consistent with the natural progression of ALS. Adverse Reactions Leading to Discontinuation The most commonly reported adverse reactions (incidence ≥ 2% and greater than placebo) that led to discontinuation with the 20 mg dextromethorphan/10 mg quinidine twice daily dose were muscle spasticity (3%), respiratory failure (1%), abdominal pain (2%), asthenia (2%), dizziness (2%), fall (1%), and muscle spasms (2%). Most Common Adverse Reactions Adverse drug reactions that occurred in ≥ 3% of patients receiving the 20 mg dextromethorphan/10 mg quinidine twice daily dose, and at an incidence of ≥ 2 times placebo in short-term clinical trials in ALS and MS are provided in Table 1. Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to the rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice. Table 1: Adverse Drug Reactions with an Incidence of ≥ 3% of Patients and ≥ 2x Placebo in NUEDEXTA-treated Patients by System-Organ Class and Preferred Term NUEDEXTA Placebo N=107 N=109 % % Diarrhea 13 6 Dizziness 10 5 Cough 5 2 Vomiting 5 1 Asthenia 5 2 Peripheral edema 5 1 Urinary tract infection 4 1 Influenza 4 1 Increased gamma- glutamyltransferase 3 0 Flatulence 3 1 6.2 Long-Term Exposure with NUEDEXTA The experience in open-label clinical trials is consistent with the safety profile observed in the placebo-controlled clinical trials. 6.3 Safety Experience of Individual Components The following adverse reactions have been reported with the use of the individual components of NUEDEXTA, dextromethorphan and quinidine, from post-marketing experience. Because these reactions are reported voluntarily from a population of unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Dextromethorphan Drowsiness, dizziness, nervousness or restlessness, nausea, vomiting, and stomach pain. Quinidine Cinchonism is most often a sign of chronic quinidine toxicity, but it may appear in sensitive patients after a single moderate dose of several hundred milligrams. Cinchonism is characterized by nausea, vomiting, diarrhea, headache tinnitus, hearing loss, vertigo, blurred vision, diplopia, photophobia, confusion, and delirium. Convulsions, apprehension, and ataxia have been reported with quinidine therapy, but it is not clear that these were not simply the results of hypotension and consequent cerebral hypoperfusion in patients being treated for cardiovascular indications. Acute psychotic reactions have been reported to follow the first dose of quinidine, but these reactions appear to be extremely rare. Other adverse reactions occasionally reported with quinidine therapy include depression, mydriasis, disturbed color perception, night blindness, scotomata, optic neuritis, visual field loss, photosensitivity, keratopathy, and abnormalities of skin pigmentation. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorization of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il/
Effects on Driving

פרטי מסגרת הכללה בסל
התרופה תינתן לטיפול ב-pseudobulbar affect.התרופה תינתן בהתאם למרשם של רופא מומחה בנוירולוגיה או בפסיכיאטריה או בשיקום.
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
15/01/2015
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
