Quest for the right Drug
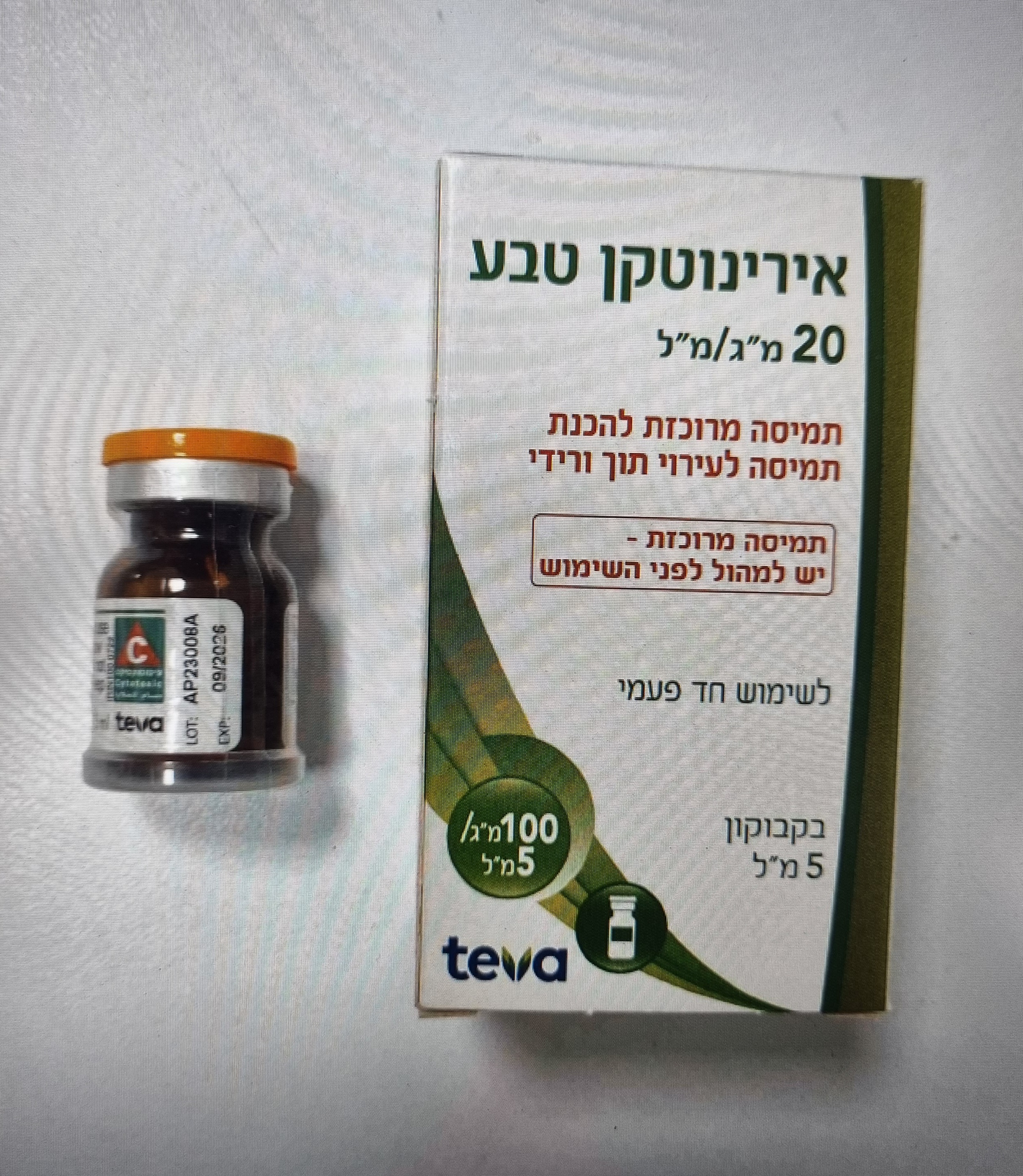
אירינוטקן טבע IRINOTECAN TEVA (IRINOTECAN HYDROCHLORIDE TRIHYDRATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תרכיז להכנת תמיסה לאינפוזיה : CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Cytostatic topoisomerase I inhibitor. ATC Code: L01CE02. Mechanism of action Experimental data Irinotecan is a semi-synthetic derivative of camptothecin. It is an antineoplastic agent which acts as a specific inhibitor of DNA topoisomerase I. It is metabolised by carboxylesterase in most tissues to SN-38, which was found to be more active than irinotecan in purified topoisomerase I and more cytotoxic than irinotecan against several murine and human tumour cell lines. The inhibition of DNA topoisomerase I by irinotecan or SN-38 induces single- strand DNA lesions which blocks the DNA replication fork and are responsible for the cytotoxicity. This cytotoxic activity was found time-dependent and was specific to the S phase. In vitro, irinotecan and SN-38 were not found to be significantly recognised by the P- glycoprotein MDR, and display cytotoxic activities against doxorubicin and vinblastine resistant cell lines. Furthermore, irinotecan has a broad antitumor activity in vivo against murine tumour models (P03 pancreatic ductal adenocarcinoma, MA16/C mammary adenocarcinoma, C38 and C51 colon adenocarcinomas) and against human xenografts (Co-4 colon adenocarcinoma, Mx-1 mammary adenocarcinoma, ST-15 and SC-16 gastric adenocarcinomas). Irinotecan is also active against tumours expressing the P-glycoprotein MDR (vincristine- and doxorubicin- resistant P388 leukaemias). Beside the antitumor activity of irinotecan, the most relevant pharmacological effect of irinotecan is the inhibition of acetylcholinesterase. Clinical data In combination therapy for the first-line treatment of metastatic colorectal carcinoma In combination therapy with Folinic Acid and 5-Fluorouracil A phase III study was performed in 385 previously untreated metastatic colorectal cancer patients treated with either every 2 weeks schedule (see section 4.2) or weekly schedule regimens. In the every 2 weeks schedule, on day 1, the administration of irinotecan at 180 mg/m² once every 2 weeks is followed by infusion with folinic acid (200 mg/m² over a 2- hour intravenous infusion) and 5-fluorouracil (400 mg/m² as an intravenous bolus, followed by 600 mg/m² over a 22-hour intravenous infusion). On day 2, folinic acid and 5-fluorouracil are administered at the same doses and schedules. In the weekly schedule, the administration of irinotecan at 80 mg/m² is followed by infusion with folinic acid (500 mg/m² over a 2-hour intravenous infusion) and then by 5-fluorouracil (2300 mg/m² over a 24-hour intravenous infusion) over 6 weeks. In the combination therapy trial with the 2 regimens described above, the efficacy of irinotecan was evaluated in 198 treated patients: Combined regimens Weekly schedule Every 2 weeks (n=198) (n=50) schedule (n=148) Irinotecan 5FU/FA Irinotecan 5FU/FA Irinotecan 5FU/FA +5FU/FA +5FU/FA +5FU/FA Response rate (%) 40.8* 23.1* 51.2* 28.6* 37.5* 21.6* p value p<0.001 p=0.045 p=0.005 Median time to progression 6.7 4.4 7.2 6.5 6.5 3.7 (months) p value p<0.001 NS p=0.001 Median duration of 9.3 8.8 8.9 6.7 9.3 9.5 response (months) p value NS p=0.043 NS Median duration of 8.6 6.2 8.3 6.7 8.5 5.6 response and stabilisation (months) p value p<0.001 NS p=0.003 Median time to treatment 5.3 3.8 5.4 5.0 5.1 3.0 failure (months) p value p=0.0014 NS P<0.001 Median survival 16.8 14.0 19.2 14.1 15.6 13.0 (months) p value p=0.028 NS p=0.041 5FU: 5-fluorouracil FA: folinic acid NS: Non Significant *As per protocol population analysis In the weekly schedule, the incidence of severe diarrhoea was 44.4 % in patients treated by irinotecan in combination with 5FU/FA and 25.6 % in patients treated by 5FU/FA alone. The incidence of severe neutropenia (neutrophil count < 500 cells/mm3) was 5.8 % in patients treated by irinotecan in combination with 5FU/FA and in 2.4 % in patients treated by 5FU/FA alone. Additionally, median time to definitive performance status deterioration was significantly longer in irinotecan combination group than in 5FU/FA alone group (p=0.046). Quality of life was assessed in this phase III study using the EORTC QLQ-C30 questionnaire. Time to definitive deterioration constantly occurred later in the irinotecan groups. The evolution of the Global Health Status/Quality of life was slightly better in irinotecan combination group although not significant, showing that efficacy of irinotecan in combination could be reached without affecting the quality of life. In monotherapy for the second-line treatment of metastatic colorectal carcinoma Clinical phase II/III studies were performed in more than 980 patients in the every-3-week dosage schedule with metastatic colorectal cancer who failed a previous 5FU regimen. The efficacy of irinotecan was evaluated in 765 patients with documented progression on 5FU at study entry. Phase III Irinotecan versus supportive care Irinotecan versus 5FU Irinotecan Supportive p values Irinotecan 5FU p values care n=183 n=127 n=90 n=129 Progression Free NA NA 33.5* 26.7 p=0.03 Survival at 6 months (%) Survival at 12 months 36.2* 13.8 p=0.0001 44.8* 32.4 p=0.0351 (%) Median survival 9.2* 6.5 p=0.0001 10.8* 8.5 p=0.0351 (months) NA: Non Applicable * Statistically significant difference In phase II studies, performed on 455 patients in the every-3-week dosage schedule, the progression free survival at 6 months was 30 % and the median survival was 9 months. The median time to progression was 18 weeks. Additionally, non-comparative phase II studies were performed in 304 patients treated with a weekly schedule regimen, at a dose of 125 mg/m² administered as an intravenous infusion over 90 minutes for 4 consecutive weeks followed by 2 weeks rest. In these studies, the median time to progression was 17 weeks and median survival was 10 months. A similar safety profile has been observed in the weekly-dosage schedule in 193 patients at the starting dose of 125 mg/m², compared to the every-3-week-dosage schedule. The median time of onset of the first liquid stool was on day 11.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption At the end of the infusion, at the recommended dose of 350 mg/m², the mean peak plasma concentrations of irinotecan and SN-38 were 7.7 µg/ml and 56 ng/ml, respectively, and the mean area under the curve (AUC) values were 34 µg.h/ml and 451 ng.h/ml, respectively. A large interindividual variability in pharmacokinetic parameters is generally observed for SN- 38. Distribution The phase I study in 60 patients with a dosage regimen of a 30-minute intravenous infusion of 100 to 750 mg/m² every three weeks, the volume of distribution at steady state (Vss): 157 L/m². In vitro, plasma protein binding for irinotecan and SN-38 was approximately 65% and 95%, respectively. Biotransformation Mass balance and metabolism studies with 14C-labelled drug have shown that more than 50% of an intravenously administered dose of irinotecan is excreted as unchanged drug, with 33% in the faeces mainly via the bile and 22% in urine. Two metabolic pathways account each for at least 12% of the dose: • Hydrolysis by carboxylesterase into active metabolite SN-38, SN-38 is mainly eliminated by glucuronidation, and further by biliary and renal excretion (less than 0.5% of the irinotecan dose) The SN-38 glucuronite is subsequently probably hydrolysed in the intestine. • Cytochrome P450 3A enzymes-dependent oxidations resulting in opening of the outer piperidine ring with formation of APC (aminopentanoic acid derivate) and NPC (primary amine derivate) (see section 4.5). Unchanged irinotecan is the major entity in plasma, followed by APC, SN-38 glucuronide and SN-38. Only SN-38 has significant cytotoxic activity. Elimination In a phase I study in 60 patients with a dosage regimen of a 30-minute intravenous infusion of 100 to 750 mg/m² every three weeks, irinotecan showed a biphasic or triphasic elimination profile. The mean plasma clearance was 15 L/h/m². The mean plasma half-life of the first phase of the triphasic model was 12 minutes, of the second phase 2.5 hours, and the terminal phase half-life was 14.2 hours. SN-38 showed a biphasic elimination profile with a mean terminal elimination half-life of 13.8 hours. Irinotecan clearance is decreased by about 40% in patients with bilirubinemia between 1.5 and 3 times the upper normal limit. In these patients a 200 mg/m² irinotecan dose leads to plasma drug exposure comparable to that observed at 350 mg/m² in cancer patients with normal liver parameters. Linearity/non-linearity A population pharmacokinetic analysis of irinotecan has been performed in 148 patients with metastatic colorectal cancer, treated with various schedules and at different doses in phase II trials. Pharmacokinetic parameters estimated with a three compartment model were similar to those observed in phase I studies. All studies have shown that irinotecan (CPT-11) and SN- 38 exposure increase proportionally with CPT-11 administered dose; their pharmacokinetics are independent of the number of previous cycles and of the administration schedule. Pharmacokinetic/Pharmacodynamic relationship(s) The intensity of the major toxicities encountered with irinotecan (e.g. leukoneutropenia and diarrhoea) are related to the exposure (AUC) to parent drug and metabolite SN-38. Significant correlations were observed between haematological toxicity (decrease in white blood cells and neutrophils at nadir) or diarrhoea intensity and both irinotecan and metabolite SN-38 AUC values in monotherapy. Patients with reduced UGT1A1 activity Uridine diphosphate-glucuronosyl transferase 1A1 (UGT1A1) is involved in the metabolic deactivation of SN-38, the active metabolite of irinotecan to inactive SN-38 glucuronide (SN- 38G). The UGT1A1 gene is highly polymorphic, resulting in variable metabolic capacities among individuals. The most well-characterised UGT1A1 genetic variants are UGT1A1*28 and UGT1A1*6. These variants and other congenital deficiencies in UGT1A1 expression (such as Gilbert's syndrome and Crigler-Najjar) are associated with reduced activity of this enzyme. Patients that are UGT1A1 poor metabolisers (e.g. homozygous for UGT1A1*28 or *6 variants) are at increased risk of severe adverse reactions such as neutropenia and diarrhoea following administration of irinotecan, as a consequence of SN-38 accumulation. According to data from several meta- analyses, the risk is higher for patients receiving irinotecan doses > 180 mg/m2 (see section 4.4). In order to identify patients at increased risk of experiencing severe neutropenia and diarrhoea, UGT1A1 genotyping can be used. Homozygous UGT1A1*28 occurs with a frequency of 8-20% in the European, African, Near Eastern and Latino population. The *6 variant is nearly absent in these populations. In the East Asian population the frequency of *28/*28 is about 1-4%, 3-8% for *6/*28 and 2-6% for *6/*6. In the Central and South Asian population the frequency of *28/*28 is around 17%, 4% for *6/*28 and 0.2% for *6/*6.

פרטי מסגרת הכללה בסל
1. התרופה תינתן לטיפול במקרים האלה: א. סרטן מעי גס מתקדם (גם כטיפול ראשון). ב. סרטן החלחולת לטיפול בחזרה מקומית של המחלה. ג. סרטן לבלב גרורתי כקו טיפול ראשון.2. מתן התרופה האמורה ייעשה לפי מרשם של רופא מומחה באונקולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| סרטן מעי גס מתקדם (גם כטיפול ראשון). | 16/12/1997 | |||
| סרטן לבלב גרורתי כקו טיפול ראשון. | 16/12/1997 | |||
| סרטן החלחולת לטיפול בחזרה מקומית של המחלה. | 16/12/1997 |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
16/12/1997
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
