Quest for the right Drug
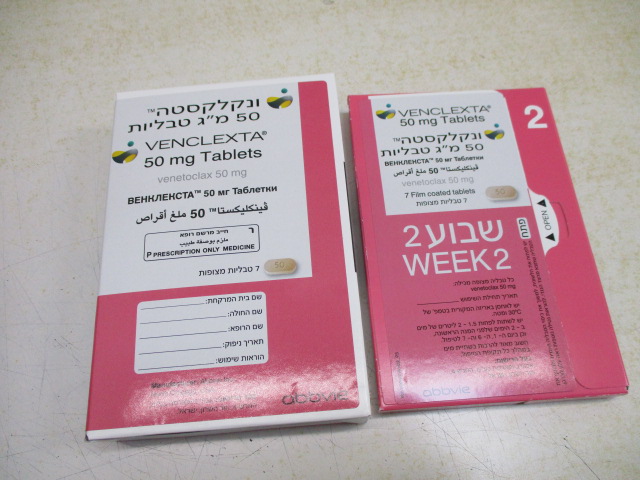
ונקלקסטה 50 מ"ג טבליות VENCLEXTA 50 MG TABLETS (VENETOCLAX)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Posology : מינונים
2 DOSAGE AND ADMINISTRATION 2.1 Important Safety Information Assess patient-specific factors for level of risk of tumor lysis syndrome (TLS) and provide prophylactic hydration and anti-hyperuricemics to patients prior to first dose of VENCLEXTA to reduce risk of TLS [see Dosage and Administration (2.4) and Warnings and Precautions (5.1)]. 2.2 Recommended Dosage for Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma VENCLEXTA dosing begins with a 5-week ramp-up. The 5-week ramp-up dosing schedule is designed to gradually reduce tumor burden (debulk) and decrease the risk of TLS. VENCLEXTA 5-week Dose Ramp-Up Schedule Administer VENCLEXTA according to the 5-week ramp-up dosing schedule to the recommended dosage of 400 mg orally once daily as shown in Table 1. Table 1. Dosing Schedule for 5-Week Ramp-up Phase for Patients with CLL/SLL VENCLEXTA Oral Daily Dose Week 1 20 mg Week 2 50 mg Week 3 100 mg Week 4 200 mg Week 5 and beyond 400 mg The CLL/SLL Starting Pack provides the first 4 weeks of VENCLEXTA according to the ramp-up schedule. [see How Supplied/Storage and Handling (16)]. In Combination with Obinutuzumab Start obinutuzumab administration at 100 mg on Cycle 1 Day 1, followed by 900 mg on Cycle 1 Day 2. Administer 1000 mg on Days 8 and 15 of Cycle 1 and on Day 1 of each subsequent 28-day cycle, for a total of 6 cycles. Refer to the obinutuzumab prescribing information for additional dosing information. On Cycle 1 Day 22, start VENCLEXTA according to the 5-week ramp-up dosing schedule (see Table 1). After completing the ramp-up phase on Cycle 2 Day 28, continue VENCLEXTA at a dose of 400 mg orally once daily from Cycle 3 Day 1 until the last day of Cycle 12. In Combination with Rituximab Start rituximab administration after the patient has completed the 5-week ramp-up dosing schedule for VENCLEXTA (see Table 1) and has received VENCLEXTA at the recommended dosage of 400 mg orally once daily for 7 days. Administer rituximab on Day 1 of each 28-day cycle for 6 cycles, at a dose of 375 mg/m2 intravenously for Cycle 1 and 500 mg/m2 intravenously for Cycles 2-6. Continue VENCLEXTA 400 mg orally once daily for 24 months from Cycle 1 Day 1 of rituximab. Refer to the rituximab prescribing information for additional dosing information. Monotherapy The recommended dosage of VENCLEXTA is 400 mg once daily after completion of the 5- week ramp-up dosing schedule (see Table 1). Continue VENCLEXTA until disease progression or unacceptable toxicity. 2.3 Recommended Dosage for Acute Myeloid Leukemia The recommended dosage and ramp-up of VENCLEXTA depends upon the combination agent. Follow the dosing schedule, including the 3-day or 4-day dose ramp-up, as shown in Table 2. Start VENCLEXTA administration on Cycle 1 Day 1 in combination with: Azacitidine 75 mg/m2 intravenously or subcutaneously once daily on Days 1-7 of each 28-day cycle; OR Decitabine 20 mg/m2 intravenously once daily on Days 1-5 of each 28-day cycle; OR Cytarabine 20 mg/m2 subcutaneously once daily on Days 1-10 of each 28-day cycle. Table 2. Dosing Schedule for 3- or 4-Day Ramp-up Phase in Patients with AML VENCLEXTA Oral Daily Dose Day 1 100 mg Day 2 200 mg Day 3 400 mg 400 mg 600 mg orally once daily of each 28-day orally once daily of each 28-day Days 4 and cycle cycle beyond in combination with in combination with azacitidine or decitabine low-dose cytarabine Continue VENCLEXTA, in combination with azacitidine or decitabine or low-dose cytarabine, until disease progression or unacceptable toxicity. Refer to Clinical Studies (14.2) and Prescribing Information for azacitidine, decitabine, or cytarabine for additional dosing information. 2.4 Risk Assessment and Prophylaxis for Tumor Lysis Syndrome Patients treated with VENCLEXTA may develop tumor lysis syndrome (TLS). Refer to the appropriate section below for specific details on management. Assess patient-specific factors for level of risk of TLS and provide prophylactic hydration and anti-hyperuricemics to patients prior to first dose of VENCLEXTA to reduce risk of TLS. Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma VENCLEXTA can cause rapid reduction in tumor and thus poses a risk for TLS in the initial 5- week ramp-up phase. Changes in blood chemistries consistent with TLS that require prompt management can occur as early as 6 to 8 hours following the first dose of VENCLEXTA and at each dose increase. TLS can also occur upon resumption of VENCLEXTA following a dosage interruption. See Table 4 and Table 5 for dose modifications of VENCLEXTA after interruption. The risk of TLS is a continuum based on multiple factors, particularly reduced renal function (creatinine clearance [CLcr] <80 mL/min) and tumor burden; splenomegaly may also increase the risk of TLS. Perform tumor burden assessments, including radiographic evaluation (e.g., CT scan), assess blood chemistry (potassium, uric acid, phosphorus, calcium, and creatinine) in all patients and correct pre-existing abnormalities prior to initiation of treatment with VENCLEXTA. The risk may decrease as tumor burden decreases [see Warnings and Precautions (5.1) and Use in Specific Populations (8.6)]. Table 3 below describes the recommended TLS prophylaxis and monitoring during VENCLEXTA treatment based on tumor burden determination from clinical trial data. Consider all patient comorbidities before final determination of prophylaxis and monitoring schedule. Reassess the risk of TLS when reinitiating VENCLEXTA after a dosage interruption lasting more than 1 week during the ramp-up phase, or more than 2 weeks after completion of ramp-up. Institute prophylaxis and monitoring as needed. Table 3. Recommended TLS Prophylaxis Based on Tumor Burden in Patients with CLL/SLL Blood Chemistry Tumor Burden Prophylaxis Monitoringc,d Hydrationa Anti- Setting and hyperuricemicsb Frequency of Assessments Low All LN <5 cm Oral Allopurinol Outpatient AND (1.5 to • For first dose of 20 ALC <25 x109/L 2 L) mg and 50 mg: Pre- dose, 6 to 8 hours, 24 hours • For subsequent ramp-up doses: Pre- dose Medium Any LN 5 to Oral Allopurinol Outpatient <10 cm (1.5 to • For first dose of OR 2 L) 20 mg and 50 mg: ALC ≥25 x109/L and consider Pre-dose, 6 to 8 additional hours, 24 hours intravenous • For subsequent ramp-up doses: Pre- dose • For first dose of 20 mg and 50 mg: Consider hospitalization for patients with CLcr<80ml/min ; see below for monitoring in hospital High Any LN ≥10 cm Oral (1.5 to Allopurinol; In hospital OR 2L) consider rasburicase • For first dose of ALC ≥25 x109/L and if baseline uric acid 20 mg and 50 mg: AND intravenous is elevated Pre-dose, 4, 8, 12 any LN ≥5 cm (150 to 200 and 24 hours mL/hr as Outpatient tolerated) • For subsequent ramp-up doses: Pre-dose, 6 to 8 hours, 24 hours ALC = absolute lymphocyte count; CLcr = creatinine clearance; LN = lymph node. a Administer intravenous hydration for any patient who cannot tolerate oral hydration. b Start allopurinol or xanthine oxidase inhibitor 2 to 3 days prior to initiation of VENCLEXTA. c Evaluate blood chemistries (potassium, uric acid, phosphorus, calcium, and creatinine); review in real time. d For patients at risk of TLS, monitor blood chemistries at 6 to 8 hours and at 24 hours at each subsequent ramp-up dose. Acute Myeloid Leukemia • All patients should have white blood cell count less than 25 × 109/L prior to initiation of VENCLEXTA. Cytoreduction prior to treatment may be required. • Prior to first VENCLEXTA dose, provide all patients with prophylactic measures including adequate hydration and anti-hyperuricemic agents and continue during ramp-up phase. • Assess blood chemistry (potassium, uric acid, phosphorus, calcium, and creatinine) and correct pre-existing abnormalities prior to initiation of treatment with VENCLEXTA. • Monitor blood chemistries for TLS at pre-dose, 6 to 8 hours after each new dose during ramp-up, and 24 hours after reaching final dose. • For patients with risk factors for TLS (e.g., circulating blasts, high burden of leukemia involvement in bone marrow, elevated pretreatment lactate dehydrogenase [LDH] levels, or reduced renal function), consider additional measures, including increased laboratory monitoring and reducing VENCLEXTA starting dose. 2.5 Dosage Modifications for Adverse Reactions Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma The recommended dosage modifications for VENCLEXTA for adverse reactions are provided in Table 4 and the recommended dose reductions for VENCLEXTA for adverse reactions are provided in Table 5. For patients having a dosage interruption lasting more than 1 week during the ramp-up phase, or more than 2 weeks after completion of ramp-up, reassess for risk of TLS to determine if reinitiation with a reduced dose is necessary (e.g., all or some levels of the dose ramp-up schedule) [see Dosage and Administration (2.2, 2.4)]. Table 4. Recommended VENCLEXTA Dosage Modifications for Adverse Reactionsa in CLL/SLL Adverse Reaction Occurrence Dosage Modification Tumor Lysis Syndrome Blood chemistry Any Withhold the next day’s dose. If changes or symptoms resolved within 24 to 48 hours of last suggestive of TLS [see dose, resume at same dose. Warnings and Precautions For any blood chemistry changes (5.1)] requiring more than 48 hours to resolve, resume at reduced dose (see Table 5). For any events of clinical TLS,b resume at reduced dose following resolution (see Table 5) . Non-Hematologic Adverse Reactions Grade 3 or 4 non- 1st occurrence Interrupt VENCLEXTA. hematologic toxicities Upon resolution to Grade 1 or baseline [see Adverse Reactions level, resume VENCLEXTA at the (6.1)] same dose. 2nd and subsequent Interrupt VENCLEXTA. occurrences Follow dose reduction guidelines in Table 5 when resuming treatment with VENCLEXTA after resolution. A larger dose reduction may occur at the discretion of the physician. Hematologic Adverse Reactions st Grade 3 neutropenia with 1 occurrence Interrupt VENCLEXTA. infection or fever; or Grade Upon resolution to Grade 1 or baseline 4 hematologic toxicities level, resume VENCLEXTA at the (except lymphopenia) [see same dose. Warnings and Precautions 2 and subsequent nd Interrupt VENCLEXTA. (5.2)] occurrences Follow dose reduction guidelines in Table 5 when resuming treatment with VENCLEXTA after resolution. A larger dose reduction may occur at the discretion of the physician. Consider discontinuing VENCLEXTA for patients who require dose reductions to less than 100 mg for more than 2 weeks. a Adverse reactions were graded using NCI CTCAE version 4.0. b Clinical TLS was defined as laboratory TLS with clinical consequences such as acute renal failure, cardiac arrhythmias, or sudden death and/or seizures [see Adverse Reactions (6.1)]. Table 5. Recommended Dose Reduction for Adverse Reactions for VENCLEXTA in CLL/SLL Dose at Interruption, mg Restart Dose, mga,b 400 300 300 200 200 100 100 50 50 20 20 10 a During the ramp-up phase, continue the reduced dose for 1 week before increasing the dose. b If a dosage interruption lasts more than 1 week during the ramp-up phase or more than 2 weeks after completion of ramp-up, reassess the risk of TLS and determine if reinitiation at a reduced dosage is necessary [see Dosage and Administration (2.2, 2.4)]. Acute Myeloid Leukemia Monitor blood counts frequently through resolution of cytopenias. Dose modification and interruptions for cytopenias are dependent on remission status. Dose modifications of VENCLEXTA. for adverse reactions are provided in Table 6. Table 6. Recommended VENCLEXTA Dosage Modifications for Adverse Reactions in AML Adverse Reaction Occurrence Dosage Modification Hematologic Adverse Reactions Grade 4 neutropenia Occurrence prior to In most instances, do not interrupt a with or without fever achieving remission VENCLEXTA in combination with or infection; or Grade 4 azacitidine, decitabine, or low-dose thrombocytopenia [see cytarabine due to cytopenias prior to Warnings and achieving remission. Precautions (5.2)] First occurrence after Delay subsequent cycle of VENCLEXTA achieving remission and in combination with azacitidine, lasting at least 7 days decitabine, or low-dose cytarabine and monitor blood counts. Upon resolution to Grade 1 or 2, resume VENCLEXTA at the same dose in combination with azacitidine, decitabine, or low-dose cytarabine. Subsequent occurrences in Delay subsequent cycle of VENCLEXTA cycles after achieving in combination with azacitidine, or remission and lasting 7 days decitabine, or low-dose cytarabine and or longer monitor blood counts. Upon resolution to Grade 1 or 2, resume VENCLEXTA at the same dose in combination with azacitidine, decitabine, or low-dose cytarabine, and reduce VENCLEXTA duration by 7 days during each of the subsequent cycles, such as 21 days instead of 28 days. Non-Hematologic Adverse Reactions Adverse Reaction Occurrence Dosage Modification Grade 3 or 4 non- Any occurrence Interrupt VENCLEXTA if not resolved hematologic toxicities with supportive care. [see Adverse Upon resolution to Grade 1 or baseline Reactions (6.1)] level, resume VENCLEXTA at the same dose. a Recommend bone marrow evaluation. 2.6 Dosage Modifications for Drug Interactions Strong or Moderate CYP3A Inhibitors or P-gp Inhibitors Table 7 describes VENCLEXTA contraindication or dosage modification based on concomitant use with a strong or moderate CYP3A inhibitor or a P-gp inhibitor [see Drug Interactions (7.1)] at initiation, during, or after the ramp-up phase. Resume the VENCLEXTA dosage that was used prior to concomitant use of a strong or moderate CYP3A inhibitor or a P-gp inhibitor 2 to 3 days after discontinuation of the inhibitor [see Drug Interactions (7.1)]. Table 7. Management of Potential VENCLEXTA Interactions with CYP3A and P-gp Inhibitors Initiation and Ramp- Steady Daily Dose Coadministered Drug Up Phase (After Ramp-Up Phase) a CLL/SLL Contraindicated Reduce VENCLEXTA dose to 70 Posaconazole AML Day 1 – 10 mg mg. Day 2 – 20 mg Day 3 – 50 mg Day 4 – 70 mg Other strong CYP3A inhibitor CLL/SLL Contraindicated Reduce VENCLEXTA dose to 100 mg. AML Day 1 – 10 mg Day 2 – 20 mg Day 3 – 50 mg Day 4 – 100 mg Moderate CYP3A inhibitor Reduce the VENCLEXTA dose by at least 50%. P-gp inhibitor a In patients with CLL/SLL, consider alternative medications or reduce the VENCLEXTA dose as described in Table 7. 2.7 Dosage Modifications for Patients with Severe Hepatic Impairment Reduce the VENCLEXTA once daily dose by 50% for patients with severe hepatic impairment (Child-Pugh C); monitor these patients more closely for adverse reactions [see Use in Specific Populations (8.7)]. 2.8 Administration Instruct patients of the following: • Take VENCLEXTA with a meal and water. • Take VENCLEXTA at approximately the same time each day. • Swallow VENCLEXTA tablets whole. Do not chew, crush, or break tablets prior to swallowing. The recommended dosage of VENCLEXTA may be delivered using any of the approved tablet strengths (e.g., patients can take 2 x 50 mg tablets or 10 x 10 mg tablets instead of 1 x 100 mg tablet as needed). If the patient misses a dose of VENCLEXTA within 8 hours of the time it is usually taken, instruct the patient to take the missed dose as soon as possible and resume the normal daily dosing schedule. If a patient misses a dose by more than 8 hours, instruct the patient not to take the missed dose and resume the usual dosing schedule the next day. If the patient vomits following dosing, instruct the patient to not take an additional dose that day and to take the next prescribed dose at the usual time.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1 .בשילוב עם Obinutuzumab לטיפול בלוקמיה מסוג CLL בחולה שטרם קיבל טיפול סיסטמי למחלתו.משך הטיפול בתכשיר להתוויה זו לא יעלה על שנה.הטיפול לא יינתן בשילוב עם Ibrutinib.2. לוקמיה מסוג CLL בחולה שמחלתו חזרה (relapsed) לאחר או הייתה עמידה (refractory) לטיפול קודם. הטיפול יינתן כמונותרפיה או בשילוב עם Rituximab. הטיפול לא יינתן בשילוב עם Ibrutinib.הטיפול בתרופה יינתן לחולה שטרם טופל ב-Venetoclax למחלתו. 3. לוקמיה מסוג AML בחולה שטרם קיבל טיפול סיסטמי למחלתו ואינו מתאים לטיפול בכימותרפיה אינטנסיבית. הטיפול יינתן בשילוב עם Cytarabine במינון נמוך (LDAC) או בשילוב עם תרופות ממשפחת ה-Hypomethylating agents (HMAs) – Azacitidine או Decitabine. ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה או מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| לוקמיה מסוג AML בחולה שטרם קיבל טיפול סיסטמי למחלתו ואינו מתאים לטיפול בכימותרפיה אינטנסיבית | ||||
| לוקמיה מסוג CLL בחולה שמחלתו חזרה (relapsed) לאחר או הייתה עמידה (refractory) לטיפול קודם | ||||
| טיפול בלוקמיה מסוג CLL - חולים עם מחלה עמידה או רפרקטורית ל-Ibrutinib, שאינם בעלי מוטציה מסוג del17p | ||||
| טיפול ב-CLL חוזרת בחולים עם מוטציה מסוג del 17p |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
12/01/2017
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
17.04.18 - עלון לצרכן 27.03.17 - עלון לצרכן 28.08.17 - עלון לצרכן עברית 27.03.17 - עלון לצרכן 03.09.19 - עלון לצרכן 18.04.21 - עלון לצרכן אנגלית 02.05.22 - עלון לצרכן אנגלית 02.05.22 - עלון לצרכן עברית 18.04.21 - עלון לצרכן ערבית 02.05.22 - עלון לצרכן ערבית 16.03.23 - עלון לצרכן אנגלית 04.04.23 - עלון לצרכן עברית 16.03.23 - עלון לצרכן ערבית 31.01.24 - עלון לצרכן עברית 15.03.24 - עלון לצרכן אנגלית 15.03.24 - עלון לצרכן ערבית 11.04.19 - החמרה לעלון 03.09.19 - החמרה לעלון 26.04.20 - החמרה לעלון 04.06.20 - החמרה לעלון 04.06.20 - החמרה לעלון 18.08.20 - החמרה לעלון 12.01.21 - החמרה לעלון 29.03.21 - החמרה לעלון 13.04.21 - החמרה לעלון 27.02.22 - החמרה לעלון 02.05.22 - החמרה לעלון 04.04.23 - החמרה לעלון 01.02.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
ונקלקסטה 50 מ"ג טבליות