Quest for the right Drug
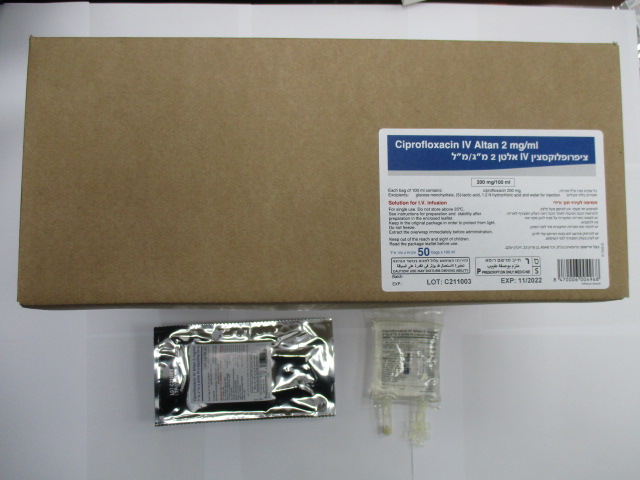
ציפרופלוקסצין I.V אלטן2 מ"ג/מ"ל CIPROFLOXACIN I.V ALTAN 2 MG/ML (CIPROFLOXACIN)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תמיסה לאינפוזיה : SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1. Pharmacodynamic properties Pharmacotherapeutic category: fluoroquinolones ATC code: J01MA02 Mechanism of action: As a fluoroquinolone antibacterial agent, the bactericidal action of ciprofloxacin results from the inhibition of both type II topoisomerase (DNA-gyrase) and topoisomerase IV, required for bacterial DNA replication, transcription, repair and recombination. Pharmacokinetic/pharmacodynamic relationship Efficacy mainly depends on the relation between the maximum concentration in serum (Cmax) and the minimum inhibitory concentration (MIC) of ciprofloxacin for a bacterial pathogen and the relation between the area under the curve (AUC) and the MIC. Mechanism of resistance: In-vitro resistance to ciprofloxacin can be acquired through a stepwise process by target site mutations in both DNA gyrase and topoisomerase IV. The degree of cross-resistance between ciprofloxacin and other fluoroquinolones that results is variable. Single mutations may not result in clinical resistance, but multiple mutations generally result in clinical resistance to many or all active substances within the class. Impermeability and/or active substance efflux pump mechanisms of resistance may have a variable effect on susceptibility to fluoroquinolones, which depends on the physiochemical properties of the various active substances within the class and the affinity of transport systems for each active substance. All in-vitro mechanisms of resistance are commonly observed in clinical isolates. Resistance mechanisms that inactivate other antibiotics such as permeation barriers (common in Pseudomonas aeruginosa) and efflux mechanisms may affect susceptibility to ciprofloxacin. Plasmid-mediated resistance encoded by qnr-genes has been reported. Spectrum of antibacterial activity: Breakpoints separate susceptible strains from strains with intermediate susceptibility and the latter from resistant strains: EUCAST recommendations Microorganisms Susceptible Resistant Enterobacteriaceae S ≤ 0.25 mg/L R > 0.5 mg/L Salmonella spp. S ≤ 0.06 mg/L R > 0.06 mg/L Pseudomonas spp. S ≤ 0.5 mg/L R > 0.5 mg/L Acinetobacter spp. S ≤ 1 mg/L R > 1 mg/L Staphylococcus spp.1 S ≤ 1 mg/L R > 1 mg/L Haemophilus influenzae S ≤ 0.06 mg/L R > 0.06 mg/L Moraxella catarrhalis S ≤ 0.125 mg/L R > 0.125 mg/L Neisseria gonorrhoeae S ≤ 0.03 mg/L R > 0.06 mg/L Neisseria meningitidis S ≤0.03 mg/L R > 0.03 mg/L Non-species related S ≤ 0.25 mg/L R > 0.5 mg/L breakpoints* 1 Staphylococcus spp. – breakpoints for ciprofloxacin related to high dose therapy. * Non-species related breakpoints have been determined mainly on the basis of PK/PD data and are independent of MIC distributions of specific species. They are for use only for species that have not been given a species-specific breakpoint and not for those species where susceptibility testing is not recommended. The prevalence of acquired resistance may vary geographically and with time for selected species and local information on resistance is desirable, particularly when treating severe infections. As necessary, expert advice should be sought when the local prevalence of resistance is such that the utility of the agent in at least some types of infections is questionable. Grouping of relevant species according to ciprofloxacin susceptibility (for Streptococcus species see section 4.4) COMMONLY SUSCEPTIBLE SPECIES Aerobic Gram-positive micro-organisms Bacillus anthracis (1) Aerobic Gram-negative micro-organisms Aeromonas spp. Brucella spp. Citrobacter koseri Francisella tularensis Haemophilus ducreyi Haemophilus influenzae* Legionella spp. Moraxella catarrhalis* Neisseria meningitidis Pasteurella spp. Salmonella spp. * Shigella spp. * Vibrio spp. Yersinia pestis Anaerobic micro-organisms Mobiluncus Other micro-organisms Chlamydia trachomatis ($) Chlamydia pneumoniae ($) Mycoplasma hominis ($) Mycoplasma pneumoniae ($) SPECIES FOR WHICH ACQUIRED RESISTANCE MAY BE A PROBLEM Aerobic Gram-positive micro-organisms Enterococcous faecalis ($) Staphylococcus spp. (2) Aerobic Gram-negative micro-organisms Acinetobacter baumannii+ Burkholderia cepacia +* Campylobacter spp.+* Citrobacter freundii* Enterobacter aerogenes Enterobacter cloacae* Escherichia coli* Klebsiella oxytoca Klebsiella pneumoniae* Morganella morganii* Neisseria gonorrhoeae* Proteus mirabilis* Proteus vulgaris* Providencia spp. Pseudomonas aeruginosa* Pseudomonas fluorescens Serratia marcescens* Anaerobic micro-organisms Peptostreptococcus spp. Propionibacterium acnes INHERENTLY RESISTANT ORGANISMS Aerobic Gram-positive micro-organisms Actinomyces Enterococcus faecium Listeria monocytogenes Aerobic Gram-negative micro-organisms Stenotrophomonas maltophilia Anaerobic micro-organisms Excepted as listed above Other micro-organisms Mycoplasma genitalium Ureaplasma urealitycum * Clinical efficacy has been demonstrated for susceptible isolates in approved clinical indications + Resistance rate ≥ 50% in one or more EU countries ($): Natural intermediate susceptibility in the absence of acquired mechanism of resistance (1): Studies have been conducted in experimental animal infections due to inhalations of Bacillus anthracis spores; these studies reveal that antibiotics starting early after exposition avoid the occurrence of the disease if the treatment is made up to the decrease of the number of spores in the organism under the infective dose. The recommended use in human subjects is based primarily on in-vitro susceptibility and on animal experimental data together with limited human data. Two-month treatment duration in adults with oral ciprofloxacin given at the following dose, 500 mg bid, is considered as effective to prevent anthrax infection in humans. The treating physician should refer to national and /or international consensus documents regarding treatment of anthrax. (2): Methicillin-resistant S. aureus very commonly expresses co-resistance to fluoroquinolones. The rate of resistance to methicillin is around 20 to 50% among all staphylococcal species and is usually higher in nosocomial isolates.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption: Following an intravenous infusion of ciprofloxacin the mean maximum serum concentrations were achieved at the end of infusion. Pharmacokinetics of ciprofloxacin were linear over the dose range up to 400 mg administered intravenously. Comparison of the pharmacokinetic parameters for a twice a day and three times a day intravenous dose regimen indicated no evidence of drug accumulation for ciprofloxacin and its metabolites. A 60-minute intravenous infusion of 200 mg ciprofloxacin or the oral administration of 250 mg ciprofloxacin, both given every 12 hours, produced an equivalent area under the serum concentration time curve (AUC). A 60-minute intravenous infusion of 400 mg ciprofloxacin every 12 hours was bioequivalent to a 500 mg oral dose every 12 hours with regard to AUC. The 400 mg intravenous dose administered over 60 minutes every 12 hours resulted in a C max R R similar to that observed with a 750 mg oral dose. A 60-minute infusion of 400 mg ciprofloxacin every 8 hours is equivalent with respect to AUC to 750 mg oral regimen given every 12 hours. Distribution: Protein binding of ciprofloxacin is low (20-30%). Ciprofloxacin is present in plasma largely in a nonionised form and has a large steady state distribution volume of 2-3 L/kg body weight. Ciprofloxacin reaches high concentrations in a variety of tissues such as lung (epithelial fluid, alveolar macrophages, biopsy tissue), sinuses, inflamed lesions (cantharides blister fluid), and the urogenital tract (urine, prostate, endometrium) where total concentrations exceeding those of plasma concentrations are reached. Biotransformation: Low concentrations of four metabolites have been reported, which were identified as: desethyleneciprofloxacin (M 1), sulphociprofloxacin (M 2), oxociprofloxacin (M 3) and formylciprofloxacin (M 4). The metabolites display in-vitro antimicrobial activity but to a lower degree than the parent compound. Ciprofloxacin is known to be a moderate inhibitor of the CYP 450 1A2 iso-enzymes. Elimination: Ciprofloxacin is largely excreted unchanged both renally and, to a smaller extent, faecally. Excretion of ciprofloxacin (% of dose) Intravenous Administration Urine Faeces Ciprofloxacin 61.5 15.2 Metabolites (M1-M4) 9.5 2.6 Renal clearance is between 180-300 mL/kg/h and the total body clearance is between 480-600 mL/kg/h. Ciprofloxacin undergoes both glomerular filtration and tubular secretion. Severely impaired renal function leads to increased half lives of ciprofloxacin of up to 12 h. Non-renal clearance of ciprofloxacin is mainly due to active trans-intestinal secretion and metabolism. 1% of the dose is excreted via the biliary route. Ciprofloxacin is present in the bile in high concentrations. Paediatric patients The pharmacokinetic data in paediatric patients are limited. In a study in children C max and AUC were not age-dependent (above one year of age). No notable increase in C max and AUC upon multiple dosing (10 mg/kg three times daily) was observed. In 10 children with severe sepsis C max was 6.1 mg/L (range 4.6-8.3 mg/L) after a 1-hour intravenous infusion of 10 mg/kg in children aged less than 1 year compared to 7.2 mg/L (range 4.7-11.8 mg/L) for children between 1 and 5 years of age. The AUC values were 17.4 mg*h/L (range 11.8-32.0 mg*h/L) and 16.5 mg*h/L (range 11.0-23.8 mg*h/L) in the respective age groups. These values are within the range reported for adults at therapeutic doses. Based on population pharmacokinetic analysis of paediatric patients with various infections, the predicted mean half- life in children is approx. 4-5 hours and the bioavailability of the oral suspension ranges from 50 to 80%.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
