Quest for the right Drug
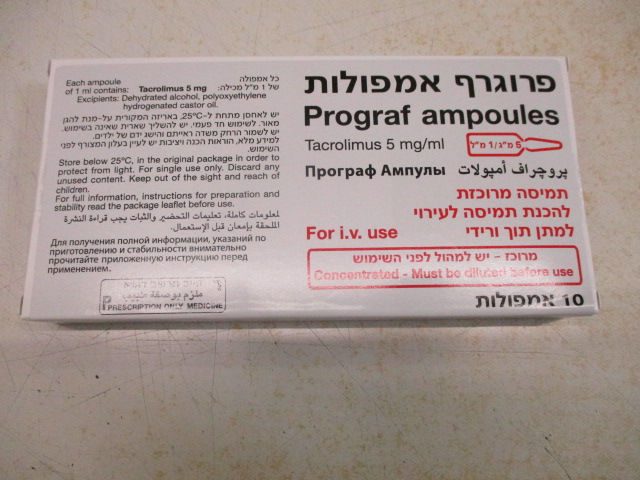
פרוגרף אמפולות PROGRAF AMPOULES (TACROLIMUS)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תרכיז להכנת תמיסה לאינפוזיה : CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use During the initial post-transplant period, monitoring of the following parameters should be undertaken on a routine basis: blood pressure, ECG, neurological and visual status, fasting blood glucose levels, electrolytes (particularly potassium), liver and renal function tests, haematology parameters, coagulation values, and plasma protein determinations. If clinically relevant changes are seen, adjustments of the immunosuppressive regimen should be considered. Substances with potential for interaction Inhibitors or inducers of CYP3A4 should only be co-administered with tacrolimus after consulting a transplant specialist, due to the potential for drug interactions resulting in serious adverse reactions including rejection or toxicity (see section 4.5). CYP3A4 inhibitors Concomitant use with CYP3A4 inhibitors may increase tacrolimus blood levels, which could lead to serious adverse reactions, including nephrotoxicity, neurotoxicity and QT prolongation. It is recommended that concomitant use of strong CYP3A4 inhibitors (such as ritonavir, cobicistat, ketoconazole, itraconazole, posaconazole, voriconazole, telithromycin, clarithromycin or josamycin) with tacrolimus should be avoided. If unavoidable, tacrolimus blood levels should be monitored frequently, starting within the first few days of co-administration, under the supervision of a transplant specialist, to adjust the tacrolimus dose if appropriate in order to maintain similar tacrolimus exposure. Renal function, ECG including the QT interval, and the clinical condition of the patient should also be closely monitored. Dose adjustment needs to be based upon the individual situation of each patient. An immediate dose reduction at the time of treatment initiation may be required (see section 4.5). Similarly, discontinuation of CYP3A4 inhibitors may affect the rate of metabolism of tacrolimus, thereby leading to subtherapeutic blood levels of tacrolimus, and therefore requires close monitoring and supervision of a transplant specialist. CYP3A4 inducers Concomitant use with CYP3A4 inducers may decrease tacrolimus blood levels potentially increasing the risk of transplant rejection. It is recommended that concomitant use of strong CYP3A4 inducers (such as rifampicin, phenytoin, carbamazepine), with tacrolimus should be avoided. If unavoidable, tacrolimus blood levels should be monitored frequently, starting within the first few days of co-administration, under the supervision of a transplant specialist, to adjust the tacrolimus dose if appropriate, in order to maintain similar tacrolimus exposure. Graft function should also be closely monitored (see section 4.5). Similarly, discontinuation of CYP3A4 inducers may affect the rate of metabolism of tacrolimus, thereby leading to supratherapeutic blood levels of tacrolimus, and therefore requires close monitoring and supervision of a transplant specialist. P-glycoprotein Caution should be observed when co-administering tacrolimus with drugs that inhibit P-glycoprotein, as an increase in tacrolimus levels may occur. Tacrolimus whole blood levels and the clinical condition of the patient should be monitored closely. An adjustment of the tacrolimus dose may be required (see section 4.5). Herbal preparations Herbal preparations containing St. John's wort (Hypericum perforatum) or other herbal preparations should be avoided when taking Prograf due to the risk of interactions that lead to either a decrease in blood concentrations of tacrolimus and reduced clinical effect of tacrolimus, or an increase in blood concentrations of tacrolimus and risk of tacrolimus toxicity (see section 4.5). Other interactions The combined administration of ciclosporin and tacrolimus should be avoided and care should be taken when administering tacrolimus to patients who have previously received ciclosporin (see sections 4.2 and 4.5). High potassium intake or potassium-sparing diuretics should be avoided (see section 4.5). Certain combinations of tacrolimus with drugs known to have nephrotoxic or neurotoxic effects may increase the risk of these effects (see section 4.5). Vaccination Immunosuppressants may affect the response to vaccination and vaccination during treatment with tacrolimus may be less effective. The use of live attenuated vaccines should be avoided. Nephrotoxicity Tacrolimus can result in renal function impairment in post-transplant patients. Acute renal impairment without active intervention may progress to chronic renal impairment. Patients with impaired renal function should be monitored closely as the dosage of tacrolimus may need to be reduced. The risk for nephrotoxicity may increase when tacrolimus is concomitantly administered with drugs associated with nephrotoxicity (see section 4.5). Concurrent use of tacrolimus with drugs known to have nephrotoxic effects should be avoided. When co-administration cannot be avoided, tacrolimus trough blood level and renal function should be monitored closely and dosage reduction should be considered if nephrotoxicity occurs. Gastrointestinal disorders Gastrointestinal perforation has been reported in patients treated with tacrolimus. As gastrointestinal perforation is a medically important event that may lead to a life-threatening or serious condition, adequate treatments should be considered immediately after suspected symptoms or signs occur. Since levels of tacrolimus in blood may significantly change during diarrhoea episodes, extra monitoring of tacrolimus concentrations is recommended during episodes of diarrhoea. Cardiac disorders Ventricular hypertrophy or hypertrophy of the septum, reported as cardiomyopathies, have been observed on rare occasions. Most cases have been reversible, occurring primarily in children with tacrolimus blood trough concentrations much higher than the recommended maximum levels. Other factors observed to increase the risk of these clinical conditions included pre- existing heart disease, corticosteroid usage, hypertension, renal or hepatic dysfunction, infections, fluid overload, and oedema. Accordingly, high-risk patients, particularly young children and those receiving substantial immunosuppression should be monitored, using such procedures as echocardiography or ECG pre- and post-transplant (e.g., initially at three months and then at 9 - 12 months). If abnormalities develop, dose reduction of Prograf therapy, or change of treatment to another immunosuppressive agent should be considered. Tacrolimus may prolong the QT interval and may cause Torsades de pointes. Caution should be exercised in patients with risk factors for QT prolongation, including patients with a personal or family history of QT prolongation, congestive heart failure, bradyarrhythmias and electrolyte abnormalities. Caution should also be exercised in patients diagnosed or suspected to have Congenital Long QT Syndrome or acquired QT prolongation or patients on concomitant medications known to prolong the QT interval, induce electrolyte abnormalities or known to increase tacrolimus exposure (see section 4.5). Lymphoproliferative disorders and malignancies Patients treated with Prograf have been reported to develop Epstein-Barr virus (EBV)-associated lymphoproliferative disorders (see section 4.8). Patients switched to Prograf therapy should not receive anti-lymphocyte treatment concomitantly. Very young (< 2 years), EBV-VCA-negative children have been reported to have an increased risk of developing lymphoproliferative disorders. Therefore, in this patient group, EBV-VCA serology should be ascertained before starting treatment with Prograf. During treatment, careful monitoring with EBV-PCR is recommended. Positive EBV-PCR may persist for months and is per se not indicative of lymphoproliferative disease or lymphoma. As with other immunosuppressive agents, owing to the potential risk of malignant skin changes, exposure to sunlight and UV light should be limited by wearing protective clothing and using a sunscreen with a high protection factor. As with other potent immunosuppressive compounds, the risk of secondary cancer is unknown (see section 4.8). Posterior reversible encephalopathy syndrome (PRES) Patients treated with tacrolimus have been reported to develop posterior reversible encephalopathy syndrome (PRES). If patients taking tacrolimus present with symptoms indicating PRES such as headache, altered mental status, seizures, and visual disturbances, a radiological procedure (e.g., MRI) should be performed. If PRES is diagnosed, adequate blood pressure and seizure control and immediate discontinuation of systemic tacrolimus is advised. Most patients completely recover after appropriate measures are taken. Eye disorders Eye disorders, sometimes progressing to loss of vision, have been reported in patients treated with tacrolimus. Some cases have reported resolution on switching to alternative immunosuppression. Patients should be advised to report changes in visual acuity, changes in colour vision, blurred vision, or visual field defect, and in such cases, prompt evaluation is recommended with referral to an ophthalmologist as appropriate. Infections including opportunistic infections Patients treated with immunosuppressants, including Prograf are at increased risk for infections including opportunistic infections (bacterial, fungal, viral and protozoal) such as CMV infection, BK virus associated nephropathy and JC virus associated progressive multifocal leukoencephalopathy (PML). Patients are also at an increased risk of infections with viral hepatitis (for example, hepatitis B and C reactivation and de novo infection, as well as hepatitis E, which may become chronic). These infections are often related to a high total immunosuppressive burden and may lead to serious or fatal conditions including graft rejection that physicians should consider in the differential diagnosis in immunosuppressed patients with deteriorating hepatic or renal function or neurological symptoms. Prevention and management should be in accordance with appropriate clinical guidance. Thrombotic microangiopathy (TMA) (including haemolytic uraemic syndrome (HUS) and thrombotic thrombocytopenic purpura (TTP)) The diagnosis of TMA, including thrombotic thrombocytopaenic purpura (TTP) and haemolytic uraemic syndrome (HUS), sometimes leading to renal failure or a fatal outcome, should be considered in patients presenting with haemolytic anaemia, thrombocytopenia, fatigue, fluctuating neurological manifestation, renal impairment, and fever. If TMA is diagnosed, prompt treatment is required, and discontinuation of tacrolimus should be considered at the discretion of the treating physician. The concomitant administration of tacrolimus with a mammalian target of rapamycin (mTOR) inhibitor (e.g., sirolimus, everolimus) may increase the risk of thrombotic microangiopathy (including haemolytic uraemic syndrome and thrombotic thrombocytopenic purpura). Pure Red Cell Aplasia Cases of pure red cell aplasia (PRCA) have been reported in patients treated with tacrolimus. All patients reported risk factors for PRCA such as parvovirus B19 infection, underlying disease or concomitant medications associated with PRCA. Excipients Prograf 5 mg/ml concentrate for solution for infusion contains polyoxyethylene hydrogenated castor oil, which has been reported to cause anaphylactoid reactions. Caution is therefore necessary in patients who have previously received preparations containing polyoxyethylene castor oil derivatives either by intravenous injection or infusion, and in patients with an allergenic predisposition. The risk of anaphylaxis may be reduced by slow infusion of reconstituted Prograf 5 mg/ml concentrate for solution for infusion or by the prior administration of an antihistamine. Patients should be closely observed during the first 30 minutes of infusion for possible anaphylactoid reaction. This medicine contains 638 mg of alcohol (ethanol) in 5 mg/ml iv infusion solution which is equivalent to 16 ml beer or 7 ml wine. The small amount of alcohol in this medicine will not have any noticeable effects. If administered accidentally either arterially or perivasally, the reconstituted Prograf 5 mg/ml concentrate for solution for infusion may cause irritation at the injection site.
Effects on Driving
4.7 Effects on ability to drive and use machines Not relevant.

פרטי מסגרת הכללה בסל
1. התרופה תינתן לטיפול במקרים האלה: א. מושתלי כליה ב. מושתלי כבד. ג. מושתלי לב. ד. מושתלי ריאה. 2. מתן התרופה ייעשה לפי מרשם של רופא מומחה באימונולוגיה קלינית או רופא מומחה העוסק בתחום ההשתלות
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| התרופה תינתן לטיפול במושתלי כליה, או מושתלי כבד, או מושתלי לב, או מושתלי ריאה |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
09/03/1999
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
רישום
107 71 29160 00
מחיר
0 ₪
מידע נוסף
