Quest for the right Drug
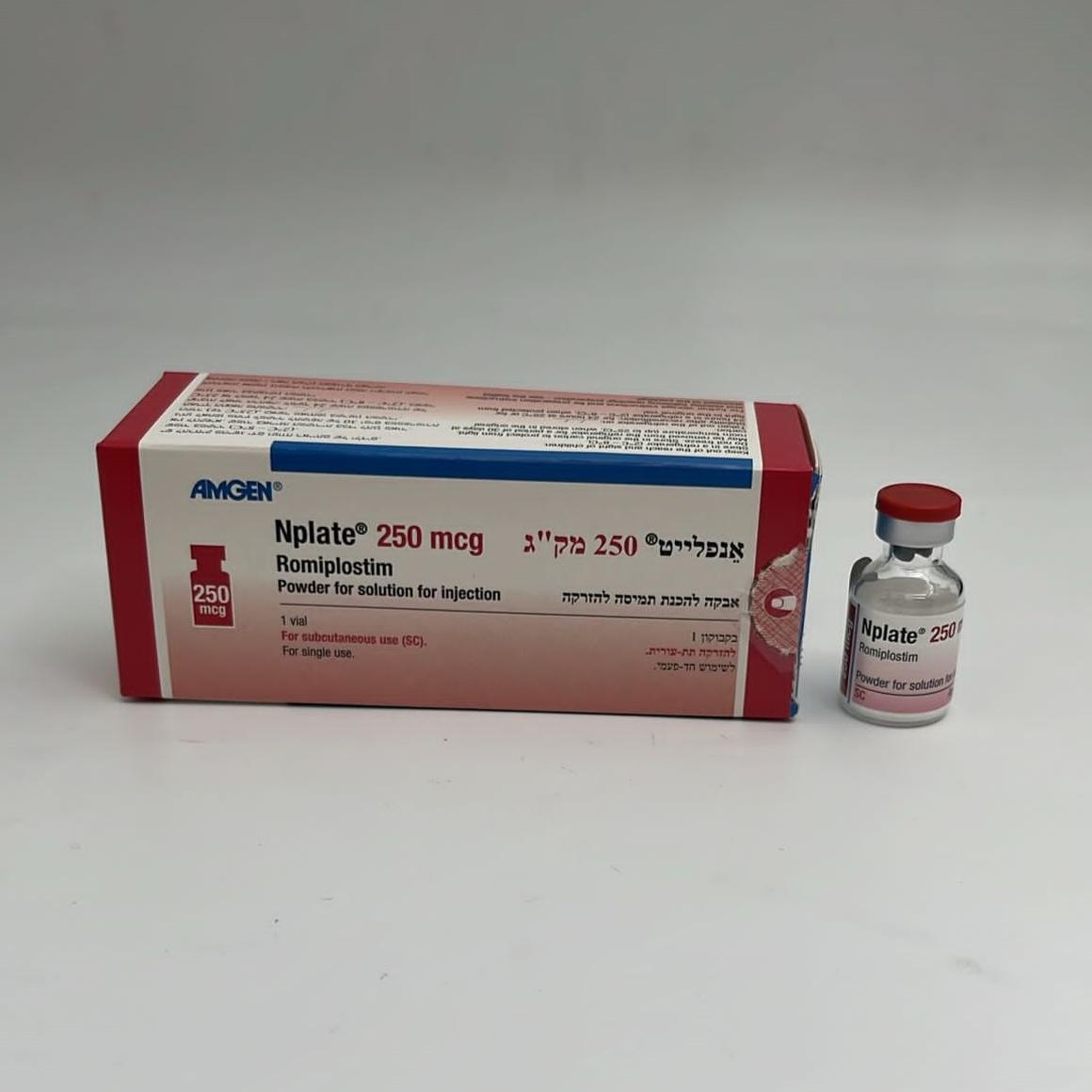
אנפלייט 250 מק"ג NPLATE 250 MCG (ROMIPLOSTIM)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תת-עורי : S.C
צורת מינון:
אבקה להכנת תמיסה לזריקה : POWDER FOR SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Summary of the safety profile Based on an analysis of all adult ITP patients receiving romiplostim in 4 controlled and 5 uncontrolled clinical trials, the overall subject incidence of all adverse reactions for romiplostim-treated subjects was 91.5% (248/271). The mean duration of exposure to romiplostim in this study population was 50 weeks. The most serious adverse reactions that may occur during Nplate treatment include: reoccurrence of thrombocytopenia and bleeding after cessation of treatment, increased bone marrow reticulin, thrombotic/thromboembolic complications, medication errors and progression of existing MDS to AML. The most common adverse reactions observed include hypersensitivity reactions (including cases of rash, urticaria and angioedema) and headache. Tabulated list of adverse reactions Frequencies are defined as: very common (≥ 1/10), common (≥ 1/100 to < 1/10), uncommon (≥ 1/1,000 to < 1/100), rare (≥ 1/10,000 to < 1/1,000), very rare (< 1/10,000) and not known (cannot be estimated from the available data). Within each MedDRA system organ class and frequency grouping, undesirable effects are presented in order of decreasing incidence. MedDRA system Very common Common Uncommon organ class Infections and Upper respiratory Gastroenteritis Influenza infestations tract infection Pharyngitis*** Localized infection Rhinitis*** Conjunctivitis*** Nasopharyngitis Ear infection*** Sinusitis***/**** Bronchitis**** MedDRA system Very common Common Uncommon organ class Neoplasms benign, Multiple myeloma malignant and Myelofibrosis unspecified (including cysts and polyps) Blood and Bone marrow Aplastic anemia lymphatic system disorder* Bone marrow failure disorders Thrombocytopenia* Leukocytosis Anemia Splenomegaly Thrombocythemia Platelet count increased Platelet count abnormal Immune system Hypersensitivity** Angioedema disorders Metabolism and Alcohol intolerance nutrition disorders Anorexia Decreased appetite Dehydration Gout Psychiatric Insomnia Depression disorders Abnormal dreams Nervous system Headache Dizziness Clonus disorders Migraine Dysgeusia Paresthesia Hypoesthesia Hypogeusia Neuropathy peripheral Transverse sinus thrombosis Eye disorders Conjunctival hemorrhage Accommodation disorder Blindness Eye disorder Eye pruritus Lacrimation increased Papilloedema Visual disturbances Ear and labyrinth Vertigo disorders Cardiac disorders Palpitations Myocardial infarction Heart rate increased MedDRA system Very common Common Uncommon organ class Vascular disorders Flushing Deep vein thrombosis Hypotension Peripheral embolism Peripheral ischemia Phlebitis Thrombophlebitis superficial Thrombosis Erythromelalgia Respiratory, Oropharyngeal Pulmonary Cough thoracic and pain*** embolism* Rhinorrhea mediastinal Dry throat disorders Dyspnea Nasal congestion Painful respiration Gastrointestinal Upper abdominal Nausea Vomiting disorders pain*** Diarrhea Rectal hemorrhage Abdominal pain Breath odor Constipation Dysphagia Dyspepsia Gastro-esophageal reflux disease Hematochezia Mouth hemorrhage Stomach discomfort Stomatitis Tooth discoloration Hepatobiliary Portal vein disorders thrombosis Increase in transaminase Skin and Pruritus Alopecia subcutaneous tissue Ecchymosis Photosensitivity disorders Rash reaction Acne Dermatitis contact Dry skin Eczema Erythema Exfoliative rash Hair growth abnormal Prurigo Purpura Rash papular Rash pruritic Skin nodule Skin odor abnormal Urticaria MedDRA system Very common Common Uncommon organ class Musculoskeletal and Arthralgia Muscle tightness connective tissue Myalgia Muscular weakness disorders Muscle spasms Shoulder pain Pain in extremity Muscle twitching Back pain Bone pain Renal and urinary Protein urine present disorders Reproductive Vaginal hemorrhage system and breast disorders General disorders Fatigue Injection site and administration Edema peripheral hemorrhage site conditions Influenza like illness Chest pain Pain Irritability Asthenia Malaise Pyrexia Face edema Chills Feeling hot Injection site Feeling jittery reaction Peripheral swelling*** Investigations Blood pressure increased Blood lactate dehydrogenase increased Body temperature increased Weight decreased Weight increased Injury, poisoning Contusion and procedural complications * see section 4.4 ** Hypersensitivity reactions including cases of rash, urticaria, and angioedema *** Additional adverse reactions observed in pediatric studies **** Additional adverse reactions observed in adult patients with ITP duration up to 12 months Adult population with ITP duration up to 12 months The safety profile of romiplostim was similar across adult patients, regardless of ITP duration. Specifically in the integrated analysis of ITP ≤ 12 months duration (n = 311), 277 adult patients with ITP ≤ 12 months duration and who received at least one dose of romiplostim from among those patients in 9 ITP studies were included (see section 5.1). In this integrated analysis, the following adverse reactions (at least 5% incidence and at least 5% more frequent with Nplate compared with placebo or standard of care) occurred in romiplostim patients with ITP duration up to 12 months, but were not observed in those adult patients with ITP duration > 12 months: bronchitis, sinusitis (reported commonly (≥ 1/100 to < 1/10)). Pediatric population In the pediatric studies, 282 pediatric ITP subjects were treated with romiplostim in 2 controlled and 3 uncontrolled clinical trials. The median duration of exposure was 65.4 weeks. The overall safety profile was similar to that seen in adults. The pediatric adverse reactions are derived from each of the pediatric ITP randomized safety set (2 controlled clinical trials) and pediatric ITP safety set (2 controlled and 3 uncontrolled clinical trials) where the subject incidence was at least 5% higher in the romiplostim arm compared to placebo and at least a 5% subject incidence in romiplostim-treated subjects. The most common adverse reactions in pediatric ITP patients 1 year and older were upper respiratory tract infection, rhinitis, cough, oropharyngeal pain, upper abdominal pain, diarrhea, rash, pyrexia, contusion (reported very commonly (≥ 1/10)), and pharyngitis, conjunctivitis, ear infection, gastroenteritis, sinusitis, purpura, urticaria and peripheral swelling (reported commonly (≥ 1/100 to < 1/10)). Oropharyngeal pain, upper abdominal pain, rhinitis, pharyngitis, conjunctivitis, ear infection, sinusitis and peripheral swelling were additional adverse reactions observed in pediatric studies compared to those seen in adult studies. Some of the adverse reactions seen in adults were reported more frequently in pediatric subjects such as cough, diarrhea, rash, pyrexia and contusion reported very commonly (≥ 1/10) in pediatric subjects and purpura and urticaria were reported commonly (≥ 1/100 to < 1/10) in pediatric subjects. Description of selected adverse reactions In addition, the reactions listed below have been deemed to be related to romiplostim treatment. Bleeding events Across the entire adult ITP clinical program an inverse relationship between bleeding events and platelet counts was observed. All clinically significant (≥ grade 3) bleeding events occurred at platelet counts < 30 × 109/L. All bleeding events ≥ grade 2 occurred at platelet counts < 50 × 109/L. No statistically significant differences in the overall incidence of bleeding events were observed between Nplate and placebo treated patients. In the two adult placebo-controlled studies, 9 patients reported a bleeding event that was considered serious (5 [6.0%] romiplostim, 4 [9.8%] placebo; Odds Ratio [romiplostim/placebo] = 0.59; 95% CI = (0.15, 2.31)). Bleeding events that were grade 2 or higher were reported by 15% of patients treated with romiplostim and 34% of patients treated with placebo (Odds Ratio; [romiplostim/placebo] = 0.35; 95% CI = (0.14, 0.85)). In the phase 3 pediatric study, the mean (SD) number of composite bleeding episodes (see section 5.1) was 1.9 (4.2) for the romiplostim arm and 4.0 (6.9) for the placebo arm. Thrombocytosis Based on an analysis of all adult ITP patients receiving romiplostim in 4 controlled and 5 uncontrolled clinical trials, 3 events of thrombocytosis were reported, n = 271. No clinical sequelae were reported in association with the elevated platelet counts in any of the 3 subjects. Thrombocytosis in pediatric subjects occurred uncommonly (≥ 1/1,000 to < 1/100), with a subject incidence of 1 (0.4%). Subject incidence was 1 (0.4%) for either grade ≥ 3 or serious thrombocytosis. Thrombocytopenia after cessation of treatment Based on an analysis of all adult ITP patients receiving romiplostim in 4 controlled and 5 uncontrolled clinical trials, 4 events of thrombocytopenia after cessation of treatment were reported, n = 271 (see section 4.4). Progression of existing Myelodysplastic Syndromes (MDS) In a randomized placebo-controlled trial in MDS adult subjects treatment with romiplostim was prematurely stopped due to a numerical increase in cases of MDS disease progression to AML and transient increases in blast cell counts in patients treated with romiplostim compared to placebo. Of the cases of MDS disease progression to AML that were observed, patients with RAEB-1 classification of MDS at baseline were more likely to have disease progression to AML (see section 4.4). Overall survival was similar to placebo. Increased bone marrow reticulin In adult clinical trials, romiplostim treatment was discontinued in 4 of the 271 patients because of bone marrow reticulin deposition. In 6 additional patients reticulin was observed upon bone marrow biopsy (see section 4.4). In a pediatric clinical trial (see section 5.1), of the subjects with an evaluable on-study bone marrow biopsy, 5 out of 27 subjects (18.5%) developed increased reticulin at year 1 after exposure to romiplostim (cohort 1) and 17 out of 36 subjects (47.2%) developed increased reticulin at year 2 after exposure to romiplostim (cohort 2). However, no subject showed any bone marrow abnormalities that were inconsistent with an underlying diagnosis of ITP at baseline or on-treatment. Immunogenicity Clinical trials in adult ITP patients examined antibodies to romiplostim and TPO. While 5.7% (60/1,046) and 3.2% (33/1,046) of the subjects were positive for developing binding antibodies to romiplostim and TPO respectively, only 4 subjects were positive for neutralizing antibodies to romiplostim but these antibodies did not cross react with endogenous TPO. Of the 4 subjects, 2 subjects tested negative for neutralizing antibodies to romiplostim at the subject’s last timepoint (transient positive) and 2 subjects remained positive at the subject’s last timepoint (persistent antibodies). The incidence of pre-existing antibodies to romiplostim and TPO was 3.3% (35/1,046) and 3.0% (31/1,046), respectively. In pediatric studies, the incidence of binding antibodies to romiplostim at any time was 9.6% (27/282). Of the 27 subjects, 2 subjects had pre-existing binding non-neutralizing romiplostim antibodies at baseline. Additionally, 2.8% (8/282) developed neutralizing antibodies to romiplostim. A total of 3.9% (11/282) subjects had binding antibodies to TPO at any time during romiplostim treatment. Of these 11 subjects, 2 subjects had pre-existing binding non-neutralizing antibodies to TPO. One subject (0.35%) had a weakly positive postbaseline result for neutralizing antibodies against TPO while on-study (consistently negative for anti-romiplostim antibodies) with a negative result at baseline. The subject showed a transient antibody response for neutralizing antibodies against TPO, with a negative result at the subject’s last timepoint tested within the study period. In the post-marketing registry study, 19 confirmed pediatric patients were included. The incidence of binding antibody post-treatment was 16% (3/19) to romiplostim, of which 5.3% (1/19) were positive for neutralizing antibodies to romiplostim. There were no antibodies detected to TPO. A total of 184 confirmed adult patients were included in this study; for these patients, the incidence of binding antibody post-treatment was 3.8% (7/184) to romiplostim, of which 0.5% (1/184) was positive for neutralizing antibodies to romiplostim. A total of 2.2% (4/184) adult patients developed binding, non-neutralizing antibody against TPO. As with all therapeutic proteins, there is a potential for immunogenicity. If formation of neutralizing antibodies is suspected, contact the local representative of the Marketing Authorization Holder for antibody testing. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorization of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il

פרטי מסגרת הכללה בסל
הטיפול בתרופה יינתן לטיפול באחד מאלה:1. בגיר החולה ב-ITP (immune thrombocytopenic purpura) כרונית או עיקשת (Persistent) הסובל מתרומבוציטופניה קשה (ספירת טסיות נמוכה מ-30,000) לאחר מיצוי טיפול בסטרואידים או אימונוגלובולינים.2. ילד עד גיל 18 שנים החולה ב- ITP (immune thrombocytopenic purpura) כרונית או עיקשת (Persistent) הסובל מתרומבוציטופניה קשה (ספירת טסיות נמוכה מ-30,000) לאחר מיצוי טיפול בסטרואידים או אימונוגלובולינים. תחילת הטיפול בתרופה ייעשה לפי מרשם של רופא מומחה בהמטולוגיה או המטולוגיה ילדים.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| בגיר החולה ב-ITP (immune thrombocytopenic purpura) כרונית הסובל תרומבוציטופניה קשה (ספירת טסיות נמוכה מ-30,000) לאחר מיצוי טיפול בסטרואידים ואימונוגלובולינים. | 30/01/2020 | המטולוגיה | Immune thrombocytopenic purpura, ITP | |
| ילד עד גיל 18 שנים החולה ב-ITP (immune thrombocytopenic purpura) כרונית הסובל תרומבוציטופניה קשה (ספירת טסיות נמוכה מ-30,000) לאחר מיצוי הטיפולים המקובלים. | 11/01/2018 | המטולוגיה | Immune thrombocytopenic purpura, ITP | |
| לחולה ITP (immune thrombocytopenic purpura) כרונית הסובל תרומבוציטופניה קשה (ספירת טסיות נמוכה מ-30,000) לאחר מיצוי הטיפולים המקובלים, כולל בין היתר RITUXIMAB וכריתת טחול, למעט חולים בהם קיימת הורית נגד לכריתת טחול | 23/01/2011 | המטולוגיה | Immune thrombocytopenic purpura, ITP | |
| הטיפול בתרופה יינתן לטיפול באחד מאלה: 1. בגיר החולה ב-ITP (immune thrombocytopenic purpura) כרונית או עיקשת (Persistent) הסובל מתרומבוציטופניה קשה (ספירת טסיות נמוכה מ-30,000) לאחר מיצוי טיפול בסטרואידים או אימונוגלובולינים. 2. ילד עד גיל 18 שנים החולה ב- ITP (immune thrombocytopenic purpura) כרונית או עיקשת (Persistent) הסובל מתרומבוציטופניה קשה (ספירת טסיות נמוכה מ-30,000) לאחר מיצוי טיפול בסטרואידים או אימונוגלובולינים. תחילת הטיפול בתרופה ייעשה לפי מרשם של רופא מומחה בהמטולוגיה או המטולוגיה ילדים. | 03/02/2022 | המטולוגיה | Immune thrombocytopenic purpura, ITP |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
23/01/2011
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
