Quest for the right Drug
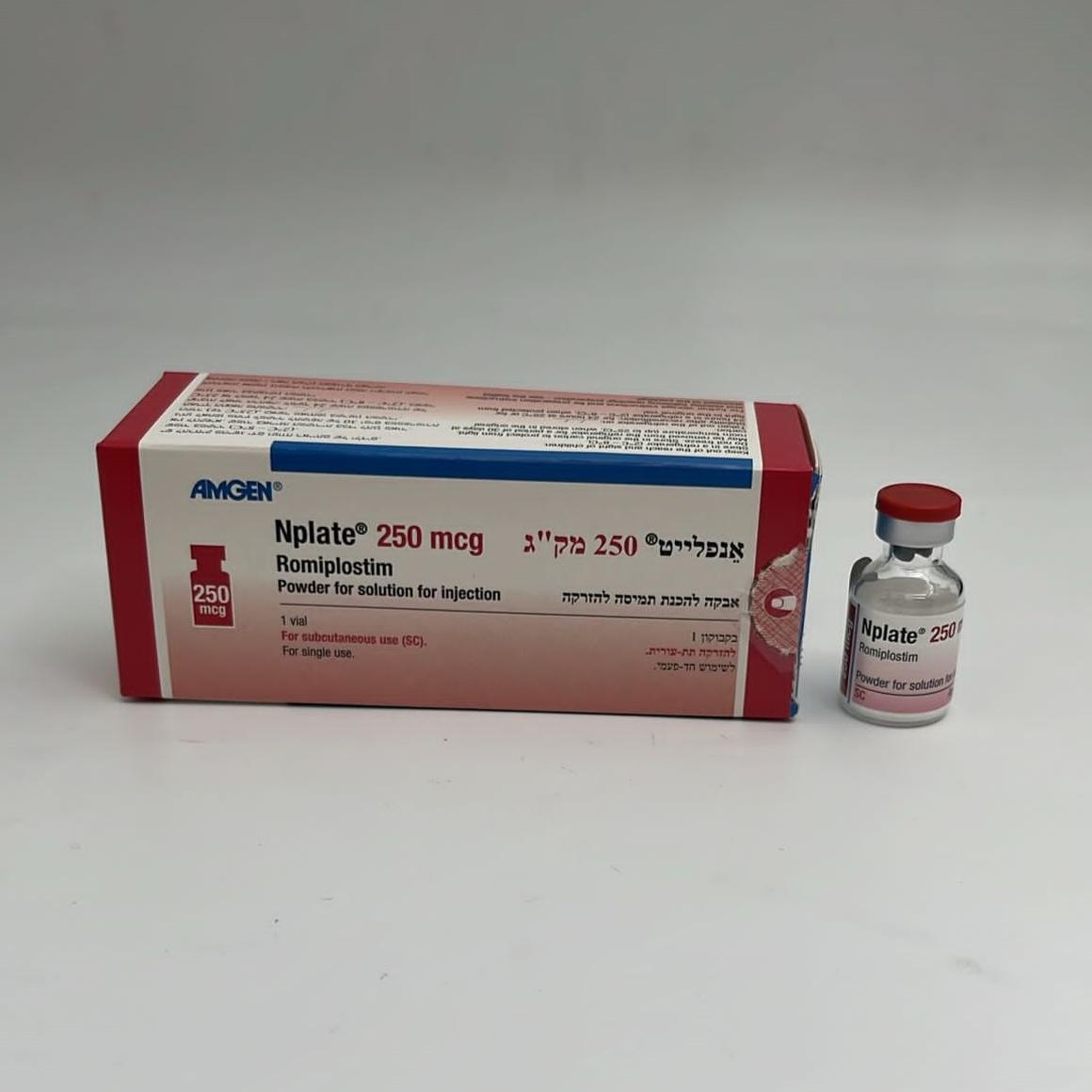
אנפלייט 250 מק"ג NPLATE 250 MCG (ROMIPLOSTIM)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תת-עורי : S.C
צורת מינון:
אבקה להכנת תמיסה לזריקה : POWDER FOR SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antihemorrhagics, other systemic hemostatics, ATC code: B02BX04 Mechanism of action Romiplostim is an Fc-peptide fusion protein (peptibody) that signals and activates intracellular transcriptional pathways via the TPO receptor (also known as cMpl) to increase platelet production. The peptibody molecule is comprised of a human immunoglobulin IgG1 Fc domain, with each single-chain subunit covalently linked at the C-terminus to a peptide chain containing 2 TPO receptor-binding domains. Romiplostim has no amino acid sequence homology to endogenous TPO. In pre-clinical and clinical trials no anti-romiplostim antibodies cross reacted with endogenous TPO. Clinical efficacy and safety The safety and efficacy of romiplostim have been evaluated for up to 3 years of continuous treatment. In clinical trials, treatment with romiplostim resulted in dose-dependent increases in platelet count. Time to reach the maximum effect on platelet count is approximately 10-14 days, and is independent of the dose. After a single subcutaneous dose of 1 to 10 mcg/kg romiplostim in ITP patients, the peak platelet count was 1.3 to 14.9 times greater than the baseline platelet count over a 2 to 3 weeks period and the response was variable among patients. The platelet counts of ITP patients who received 6 weekly doses of 1 or 3 mcg/kg of romiplostim were within the range of 50 to 450 × 109/L for most patients. Of the 271 patients who received romiplostim in ITP clinical trials, 55 (20%) were age 65 and over, and 27 (10%) were 75 and over. No overall differences in safety or efficacy have been observed between older and younger patients in the placebo-controlled studies. Results from pivotal placebo-controlled studies The safety and efficacy of romiplostim was evaluated in two placebo-controlled, double-blind studies in adults with ITP who had completed at least one treatment prior to study entry and are representative of the entire spectrum of such ITP patients. Study S1 (20030212) evaluated patients who were non-splenectomized and had an inadequate response or were intolerant to prior therapies. Patients had been diagnosed with ITP for a median of 2.1 years (range 0.1 to 31.6) at the time of study entry. Patients had received a median of 3 (range 1 to 7) treatments for ITP prior to study entry. Prior treatments included corticosteroids (90% of all patients), immunoglobulins (76%), rituximab (29%), cytotoxic therapies (21%), danazol (11%), and azathioprine (5%). Patients had a median platelet count of 19 × 109/L at study entry. Study S2 (20030105) evaluated patients who were splenectomized and continued to have thrombocytopenia. Patients had been diagnosed with ITP for a median of 8 years (range 0.6 to 44.8) at the time of study entry. In addition to a splenectomy, patients had received a median of 6 (range 3 to 10) treatments for ITP prior to study entry. Prior treatments included corticosteroids (98% of all patients), immunoglobulins (97%), rituximab (71%), danazol (37%), cytotoxic therapies (68%), and azathioprine (24%). Patients had a median platelet count of 14 × 109/L at study entry. Both studies were similarly designed. Patients (≥ 18 years) were randomized in a 2:1 ratio to receive a starting dose of romiplostim 1 mcg/kg or placebo. Patients received single subcutaneous weekly injections for 24 weeks. Doses were adjusted to maintain (50 to 200 × 109/L) platelet counts. In both studies, efficacy was determined by an increase in the proportion of patients who achieved a durable platelet response. The median average weekly dose for splenectomized patients was 3 mcg/kg and for non-splenectomized patients was 2 mcg/kg. A significantly higher proportion of patients receiving romiplostim achieved a durable platelet response compared to patients receiving placebo in both studies. Following the first 4 weeks of study romiplostim maintained platelet counts ≥ 50 × 109/L in between 50% to 70% of patients during the 6 months treatment period in the placebo-controlled studies. In the placebo group, 0% to 7% of patients were able to achieve a platelet count response during the 6 months of treatment. A summary of the key efficacy endpoints is presented below. Summary of key efficacy results from placebo-controlled studies Study 1 Combined Study 2 non-splenectomized studies 1 & 2 splenectomized patients patients Romiplostim Placebo Romiplostim Placebo Romiplostim Placebo (n = 41) (n = 21) (n = 42) (n = 21) (n = 83) (n = 42) No. (%) patients with 25 (61%) 1 (5%) 16 (38%) 0 (0%) 41 (50%) 1 (2%) durable platelet responsea (95% (0%, (0%, (45%, 76%) (24%, 54%) (38%, 61%) (0%, 13%) CI) 24%) 16%) p-value < 0.0001 0.0013 < 0.0001 No. (%) patients with 36 (88%) 3 (14%) 33 (79%) 0 (0%) 69 (83%) 3 (7%) overall platelet responseb (95% (3%, (0%, (74%, 96%) (63%, 90%) (73%, 91%) (2%, 20%) CI) 36%) 16%) p-value < 0.0001 < 0.0001 < 0.0001 Mean no. weeks with 15 1 12 0 14 1 platelet responsec (SD) 3.5 7.5 7.9 0.5 7.8 2.5 p-value < 0.0001 < 0.0001 < 0.0001 No. (%) patients requiring 8 (20%) 13 (62%) 11 (26%) 12 (57%) 19 (23%) 25 (60%) rescue therapies d (95% (38%, (34%, (43%, (9%, 35%) (14%, 42%) (14%, 33%) CI) 82%) 78%) 74%) p-value 0.001 0.0175 < 0.0001 No. (%) patients with durable platelet 21 (51%) 0 (0%) 13 (31%) 0 (0%) 34 (41%) 0 (0%) response with stable dosee (95% (0%, (0%, (35%, 67%) (18%, 47%) (30%, 52%) (0%, 8%) CI) 16%) 16%) p-value 0.0001 0.0046 < 0.0001 Study 1 Combined Study 2 non-splenectomized studies 1 & 2 splenectomized patients patients Romiplostim Placebo Romiplostim Placebo Romiplostim Placebo (n = 41) (n = 21) (n = 42) (n = 21) (n = 83) (n = 42) a Durable platelet response was defined as weekly platelet count ≥ 50 × 109/L for 6 or more times for study weeks 18-25 in the absence of rescue therapies any time during the treatment period. b Overall platelet response is defined as achieving durable or transient platelet responses. Transient platelet response was defined as weekly platelet count ≥ 50 × 109/L for 4 or more times during study weeks 2-25 but without durable platelet response. Patient may not have a weekly response within 8 weeks after receiving any rescue medicinal products. c Number of weeks with platelet response is defined as number of weeks with platelet counts ≥ 50 × 109/L during study weeks 2-25. Patient may not have a weekly response within 8 weeks after receiving any rescue medicinal products. d Rescue therapies defined as any therapy administered to raise platelet counts. Patients requiring rescue medicinal products were not considered for durable platelet response. Rescue therapies allowed in the study were IVIG, platelet transfusions, anti-D immunoglobulin, and corticosteroids. e Stable dose defined as dose maintained within ± 1 mcg/kg during the last 8 weeks of treatment. Results of studies in adult patients with newly diagnosed and persistent ITP Study S3 (20080435) was a single-arm, open-label study in adult patients who had an insufficient response (platelet count ≤ 30 × 109/L) to first line therapy. The study enrolled 75 patients of whom the median age was 39 years (range 19 to 85) and 59% were female. The median time from ITP diagnosis to study enrolment was 2.2 months (range 0.1 to 6.6). Sixty percent of patients (n = 45) had ITP duration < 3 months and 40% (n = 30) had ITP duration ≥ 3 months. The median platelet count at screening was 20 × 109/L. Prior ITP treatments included corticosteroids, immunoglobulins and anti-D immunoglobulins. Patients already receiving ITP medical therapies at a constant dosing schedule were allowed to continue receiving these medical treatments throughout the studies. Rescue therapies (i.e., corticosteroids, IVIG, platelet transfusions, anti-D immunoglobulin, dapsone, danazol, and azathioprine) were permitted. Patients received single weekly SC injections of romiplostim over a 12-month treatment period, with individual dose adjustments to maintain platelet counts (50 × 109/L to 200 × 109/L). During the study, the median weekly romiplostim dose was 3 mcg/kg (25th-75th percentile: 2-4 mcg/kg). Of the 75 patients enrolled in study 20080435, 70 (93%) had a platelet response ≥ 50 × 109/L during the 12-month treatment period. The mean number of months with platelet response during the 12-month treatment period was 9.2 (95% CI: 8.3, 10.1) months; the median was 11 (95% CI: 10, 11) months. The Kaplan Meier estimate of the median time to first platelet response was 2.1 weeks (95% CI: 1.1, 3.0). Twenty-four (32%) patients had sustained treatment-free remission as defined by maintaining every platelet count ≥ 50 × 109/L for at least 6 months in the absence of romiplostim and any medication for ITP (concomitant or rescue); the median time to onset of maintaining every platelet count ≥ 50 × 109/L for at least 6 months was 27 weeks (range 6 to 57). In an integrated analysis of efficacy, 277 adult patients with ITP duration ≤ 12 months and who received at least one dose of romiplostim from among those patients in 9 ITP studies (inclusive of study S3) were included. Of the 277 romiplostim-treated patients, 140 patients had newly diagnosed ITP (ITP duration < 3 months) and 137 patients had persistent ITP (ITP duration ≥ 3 to ≤ 12 months). The percentage of patients achieving a durable platelet response, defined as at least 6 weekly platelet counts of ≥ 50 × 109/L during weeks 18 through 25 of treatment, was 50% (95% CI: 41.4% to 58.6%) for the 140 patients with newly diagnosed ITP and 55% (95% CI: 46.7% to 64.0%) for the 137 patients with persistent ITP. The median (Q1, Q3) percent time with a platelet response ≥ 50 × 109/L was 100.0% (70.3%, 100.0%) for patients with newly diagnosed ITP and 93.5% (72.2%, 100.0%) for patients with persistent ITP, respectively. Also, the percentage of patients requiring rescue medications was 47.4% for patients with newly diagnosed ITP and 44.9% for patients with persistent ITP. Results of studies compared to standard of care (SOC) in non-splenectomized patients Study S4 (20060131) was an open-label randomized 52 week trial in adult subjects who received romiplostim or medical standard of care (SOC) treatment. Patients had been diagnosed with ITP for a median of 2 years (range 0.01 to 44.2) at the time of study entry. This study evaluated non-splenectomized patients with ITP and platelet counts < 50 × 109/L. Romiplostim was administered to 157 subjects by subcutaneous injection once weekly starting at a dose of 3 mcg/kg, and adjusted throughout the study within a range of 1-10 mcg/kg in order to maintain platelet counts between 50 and 200 × 109/L, 77 subjects received SOC treatment according to standard institutional practice or therapeutic guidelines. The overall subject incidence rate of splenectomy was 8.9% (14 of 157 subjects) in the romiplostim group compared with 36.4% (28 of 77 subjects) in the SOC group, with an odds ratio (romiplostim vs SOC) of 0.17 (95% CI: 0.08, 0.35). The overall subject incidence of treatment failure was 11.5% (18 of 157 subjects) in the romiplostim group compared with 29.9% (23 of 77 subjects) in the SOC group, with an odds ratio (romiplostim vs SOC) of 0.31 (95% CI: 0.15, 0.61). Of the 157 subjects randomized to the romiplostim group, three subjects did not receive romiplostim. Among the 154 subjects who received romiplostim, the total median exposure to romiplostim was 52.0 weeks and ranged from 2 to 53 weeks. The most frequently used weekly dose was between 3-5 mcg/kg (25th-75th percentile respectively; median 3 mcg/kg). Of the 77 subjects randomized to the SOC group, two subjects did not receive any SOC. Among the 75 subjects who received at least one dose of SOC, the total median exposure to SOC was 51 weeks and ranged from 0.4 to 52 weeks. Reduction in permitted concurrent ITP medical therapies In both adult placebo-controlled, double-blind studies, patients already receiving ITP medical therapies at a constant dosing schedule were allowed to continue receiving these medical treatments throughout the study (corticosteroids, danazol and/or azathioprine). Twenty-one non-splenectomized and 18 splenectomized patients received on-study ITP medical treatments (primarily corticosteroids) at the start of study. All (100%) splenectomized patients who were receiving romiplostim were able to reduce the dose by more than 25% or discontinue the concurrent ITP medical therapies by the end of the treatment period compared to 17% of placebo treated patients. Seventy-three percent of non-splenectomized patients receiving romiplostim were able to reduce the dose by more than 25% or discontinue concurrent ITP medical therapies by the end of the study compared to 50% of placebo treated patients (see section 4.5). Bleeding events Across the entire adult ITP clinical program an inverse relationship between bleeding events and platelet counts was observed. All clinically significant (≥ grade 3) bleeding events occurred at platelet counts < 30 × 109/L. All bleeding events ≥ grade 2 occurred at platelet counts < 50 × 109/L. No statistically significant differences in the overall incidence of bleeding events were observed between romiplostim and placebo treated patients. In the two adult placebo-controlled studies, 9 patients reported a bleeding event that was considered serious (5 [6.0%] romiplostim, 4 [9.8%] placebo; Odds Ratio [romiplostim/placebo] = 0.59; 95% CI = (0.15, 2.31)). Bleeding events that were grade 2 or higher were reported by 15% of patients treated with romiplostim and 34% of patients treated with placebo (Odds Ratio; [romiplostim/placebo] = 0.35; 95% CI = (0.14, 0.85)). Pediatric population The safety and efficacy of romiplostim was evaluated in two placebo-controlled, double-blind studies. Study S5 (20080279) was a phase 3 study with 24 weeks of romiplostim treatment and study S6 (20060195) was a phase 1/2 study with 12 weeks of romiplostim treatment (up to 16 weeks for eligible responders who enter a 4-week pharmacokinetic assessment period). Both studies enrolled pediatric subjects (≥ 1 year to < 18 years of age) with thrombocytopenia (defined by a mean of 2 platelet counts ≤ 30 × 109/L with neither count > 35 × 109/L in both studies) with ITP, regardless of splenectomy status. In study S5, 62 subjects were randomized in a 2:1 ratio to receive romiplostim (n = 42) or placebo (n = 20) and stratified into 1 of 3 age cohorts. The starting dose of romiplostim 1 mcg/kg and doses were adjusted to maintain (50 to 200 × 109/L) platelet counts. The most frequently used weekly dose was 3-10 mcg/kg and the maximum allowed dose on-study was 10 mcg/kg. Patients received single subcutaneous weekly injections for 24 weeks. Of those 62 subjects, 48 subjects had ITP > 12 months of duration (32 subjects received romiplostim and 16 subjects received placebo). The primary endpoint was the incidence of durable response, defined as achieving at least 6 weekly platelet counts of ≥ 50 × 109/L during weeks 18 through 25 of treatment. Overall, a significant greater proportion of subjects in the romiplostim arm achieved the primary endpoint compared with subjects in the placebo arm (p = 0.0018). A total of 22 subjects (52%) had durable platelet response in the romiplostim arm compared with 2 subjects (10%) in the placebo arm: ≥ 1 to < 6 years 38% versus 25%; ≥ 6 to < 12 years 56% versus 11%; ≥ 12 to < 18 years 56% versus 0%. In the subset of subjects with ITP > 12 months of duration, the incidence of durable response was also significantly greater in the romiplostim arm compared with the placebo arm (p = 0.0022). A total of 17 subjects (53.1%) had durable platelet response in the romiplostim arm compared with 1 subject (6.3%) in the placebo arm: ≥ 1 to < 6 years 28.6% versus 25%; ≥ 6 to < 12 years 63.6% versus 0%; ≥ 12 to < 18 years 57.1% versus 0%. The composite bleeding episode was defined as clinically significant bleeding events or the use of a rescue medication to prevent a clinically significant bleeding event during weeks 2 through 25 of the treatment period. A clinically significant bleeding event was defined as a Common Terminology Criteria for Adverse Events (CTCAE) version 3.0 grade ≥ 2 bleeding event. The mean (SD) number of composite bleeding episodes was 1.9 (4.2) for the romiplostim arm and 4.0 (6.9) for the placebo arm with a median (Q1, Q3) number of bleeding events of 0.0 (0, 2) for the romiplostim arm and 0.5 (0, 4.5) in the placebo arm. In the subset of subjects with ITP > 12 months of duration, the mean (SD) number of composite bleeding episodes was 2.1 (4.7) for the romiplostim arm and 4.2 (7.5) for the placebo arm with a median (Q1, Q3) number of bleeding events of 0.0 (0, 2) for the romiplostim arm and 0.0 (0, 4) in the placebo arm. Because the statistical testing for the incidence of rescue medication use was not significant, no statistical test was done for the number of composite bleeding episodes endpoint. In study S6, 22 subjects were randomized in a 3:1 ratio to receive romiplostim (n = 17) or placebo (n = 5). Doses were increased in increments of 2 mcg/kg every 2 weeks and the target platelet count was ≥ 50 × 109/L. Treatment with romiplostim resulted in statistically significantly greater incidence of platelet response compared with placebo (p = 0.0008). Of those 22 subjects, 17 subjects had ITP > 12 months of duration (14 subjects received romiplostim and 3 subjects received placebo). Treatment with romiplostim resulted in statistically significantly greater incidence of platelet response compared with placebo (p = 0.0147). Pediatric subjects who had completed a prior romiplostim study (including study S5) were allowed to enroll in study S7 (20090340), an open-label extension study evaluating the safety and efficacy of long-term dosing of romiplostim in thrombocytopenic pediatric subjects with ITP. A total of 66 subjects were enrolled in this study, including 54 subjects (82%) who had completed study S5. Of these, 65 subjects (98.5%) received at least 1 dose of romiplostim. The median (Q1, Q3) duration of treatment was 135.0 weeks (95.0 weeks, 184.0 weeks). The median (Q1, Q3) average weekly dose was 4.82 mcg/kg (1.88 mcg/kg, 8.79 mcg/kg). The median (Q1, Q3) of most frequent dose received by subjects during the treatment period was 5.0 mcg/kg (1.0 mcg/kg, 10.0 mcg/kg). Of the 66 subjects enrolled in the study, 63 subjects had ITP > 12 months of duration. All the 63 subjects received at least 1 dose of romiplostim. The median (Q1, Q3) duration of treatment was 138.0 weeks (91.1 weeks, 186.0 weeks). The median (Q1, Q3) average weekly dose was 4.82 mcg/kg (1.88 mcg/kg, 8.79 mcg/kg). The median (Q1, Q3) of most frequent dose received by subjects during the treatment period was 5.0 mcg/kg (1.0 mcg/kg, 10.0 mcg/kg). Across the study, the overall subject incidence of platelet response (1 or more platelet count ≥ 50 × 109/L in the absence of rescue medication) was 93.8% (n = 61) and was similar across age groups. Across all subjects, the median (Q1, Q3) number of months with platelet response was 30.0 months (13.0 months, 43.0 months) and the median (Q1, Q3) time on-study was 34.0 months (24.0 months, 46.0 months). Across all subjects, the median (Q1, Q3) percentage of months with platelet response was 93.33% (67.57%, 100.00%) and was similar across age groups. In the subset of subjects with ITP > 12 months of duration, the overall subject incidence of platelet response was 93.7% (n = 59) and was similar across age groups. Across all subjects, the median (Q1, Q3) number of months with platelet response was 30.0 months (13.0 months, 43.0 months) and the median (Q1, Q3) time on-study was 35.0 months (23.0 months, 47.0 months). Across all subjects, the median (Q1, Q3) percentage of months with platelet response was 93.33% (67.57%, 100.00%) and was similar across age groups. A total of 31 subjects (47.7%) used concurrent ITP therapy during the study including 23 subjects (35.4%) who used rescue medication and 5 subjects (7.7%) who used concurrent ITP medication at baseline. The subject prevalence of concurrent ITP medication use showed a trend towards a reduction over the course of the study: from 30.8% (weeks 1 to 12) to < 20.0% (weeks 13 to 240), and then 0% from week 240 to the end of the study. In the subset of subjects with ITP > 12 months of duration, 29 subjects (46.0%) used concurrent ITP therapy during the study including 21 subjects (33.3%) who used rescue medication and 5 subjects (7.9%) who used concurrent ITP medication at baseline. The subject prevalence of concurrent ITP medication use showed a trend towards a reduction over the course of the study: from 31.7% (weeks 1 to 12) to < 20.0% (weeks 13 to 240), and then 0% from week 240 to the end of the study. The subject prevalence of rescue medication use showed a trend towards a reduction over the course of the study: from 24.6% (weeks 1 to 12) to < 13.0% (weeks 13 to 216), then 0% after week 216 until the end of the study. Similar reduction of the subject prevalence of rescue medication over the course of the study was seen in the subset of subjects with ITP > 12 months of duration: from 25.4% (weeks 1 to 12) to ≤ 13.1% (weeks 13 to 216), then 0% after week 216 until the end of the study. Study S8 (20101221) was a phase 3, long-term, single-arm, open-label, multicenter study conducted in 203 pediatric patients with ITP diagnosed for at least 6 months and who received at least 1 prior ITP therapy (excluding romiplostim) or were ineligible for other ITP therapies. Romiplostim was administered weekly by subcutaneous injection starting at a dose of 1 mcg/kg with weekly increments to a maximum dose of 10 mcg/kg to reach a target platelet count between 50 × 109/L and 200 × 109/L. The median age of the patients was 10 years (range 1 to 17 years) and the median duration of treatment were 155.9 (range 8.0 to 163.0) weeks. The mean (SD) and median percentage of time with a platelet response (platelet count ≥ 50 × 109/L) within the first 6 months of initiation of romiplostim without rescue medication use for the past 4 weeks was 50.57% (37.01) and 50.0%, respectively. Sixty (29.6%) subjects overall received rescue medications. Rescue medications (i.e., corticosteroids, platelet transfusions, IVIG, azathioprine, anti-D immunoglobulin, and danazol) were permitted. Study S8 also evaluated bone marrows for reticulin and collagen formation as well as for abnormalities in pediatric patients with ITP receiving romiplostim treatment. The modified Bauermeister grading scale was used for reticulin and collagen assessments, whereas cytogenetics and fluorescence in situ hybridization (FISH) were used to evidence bone marrow abnormalities. Based on cohort assignment at the time of study enrolment, patients were evaluated for bone marrow reticulin and collagen at year 1 (cohort 1) or year 2 (cohort 2) in comparison to the baseline bone marrow at the start of the study. From the total of 79 patients enrolled in the 2 cohorts, 27 of 30 (90%) patients in cohort 1 and 36 of 49 (73.5%) patients in cohort 2 had evaluable on-study bone marrow biopsies. Increased reticulin fiber formation was reported for 18.5% (5 of 27) of patients in cohort 1 and 47.2% (17 of 36) of patients in cohort 2. No patients in either cohort developed collagen fibrosis or a bone marrow abnormality that was inconsistent with an underlying diagnosis of ITP.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties The pharmacokinetics of romiplostim involved target-mediated disposition, which is presumably mediated by TPO receptors on platelets and other cells of the thrombopoietic lineage such as megakaryocytes. Absorption After subcutaneous administration of 3 to 15 mcg/kg romiplostim, maximum romiplostim serum levels in ITP patients were obtained after 7-50 hours (median 14 hours). The serum concentrations varied among patients and did not correlate with the dose administered. Romiplostim serum levels appear inversely related to platelet counts. Distribution The volume of distribution of romiplostim following intravenous administration of romiplostim decreased nonlinearly from 122, 78.8, to 48.2 mL/kg for intravenous doses of 0.3, 1.0 and 10 mcg/kg, respectively in healthy subjects. This non-linear decrease in volume of distribution is in line with the (megakaryocyte and platelet) target-mediated binding of romiplostim, which may be saturated at the higher doses applied. Elimination Elimination half-life of romiplostim in ITP patients ranged from 1 to 34 days (median, 3.5 days). The elimination of serum romiplostim is in part dependent on the TPO receptor on platelets. As a result for a given dose, patients with high platelet counts are associated with low serum concentrations and vice versa. In another ITP clinical trial, no accumulation in serum concentrations was observed after 6 weekly doses of romiplostim (3 mcg/kg). Special populations Pharmacokinetics of romiplostim in patients with renal and hepatic impairment has not been investigated. Romiplostim pharmacokinetics appear not affected by age, weight and gender to a clinically significant extent. Pediatric population Pharmacokinetic data of romiplostim were collected from two studies in 21 pediatric subjects with ITP. In study S6 (20060195), romiplostim concentrations were available from 17 subjects at doses ranging from 1 to 10 mcg/kg. In Study S7 (20090340), intensive romiplostim concentrations were available from 4 subjects (2 at 7 mcg/kg and 2 at 9 mcg/kg). Serum concentrations of romiplostim in pediatrics with ITP were within the range observed in adult ITP subjects receiving the same dose range of romiplostim. Similar to adults with ITP, romiplostim pharmacokinetics are highly variable in pediatric subjects with ITP and are not reliable and predictive. However, the data are insufficient to draw any meaningful conclusion relating to the impact of dose and age on the pharmacokinetics of romiplostim.

פרטי מסגרת הכללה בסל
הטיפול בתרופה יינתן לטיפול באחד מאלה:1. בגיר החולה ב-ITP (immune thrombocytopenic purpura) כרונית או עיקשת (Persistent) הסובל מתרומבוציטופניה קשה (ספירת טסיות נמוכה מ-30,000) לאחר מיצוי טיפול בסטרואידים או אימונוגלובולינים.2. ילד עד גיל 18 שנים החולה ב- ITP (immune thrombocytopenic purpura) כרונית או עיקשת (Persistent) הסובל מתרומבוציטופניה קשה (ספירת טסיות נמוכה מ-30,000) לאחר מיצוי טיפול בסטרואידים או אימונוגלובולינים. תחילת הטיפול בתרופה ייעשה לפי מרשם של רופא מומחה בהמטולוגיה או המטולוגיה ילדים.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| בגיר החולה ב-ITP (immune thrombocytopenic purpura) כרונית הסובל תרומבוציטופניה קשה (ספירת טסיות נמוכה מ-30,000) לאחר מיצוי טיפול בסטרואידים ואימונוגלובולינים. | 30/01/2020 | המטולוגיה | Immune thrombocytopenic purpura, ITP | |
| ילד עד גיל 18 שנים החולה ב-ITP (immune thrombocytopenic purpura) כרונית הסובל תרומבוציטופניה קשה (ספירת טסיות נמוכה מ-30,000) לאחר מיצוי הטיפולים המקובלים. | 11/01/2018 | המטולוגיה | Immune thrombocytopenic purpura, ITP | |
| לחולה ITP (immune thrombocytopenic purpura) כרונית הסובל תרומבוציטופניה קשה (ספירת טסיות נמוכה מ-30,000) לאחר מיצוי הטיפולים המקובלים, כולל בין היתר RITUXIMAB וכריתת טחול, למעט חולים בהם קיימת הורית נגד לכריתת טחול | 23/01/2011 | המטולוגיה | Immune thrombocytopenic purpura, ITP | |
| הטיפול בתרופה יינתן לטיפול באחד מאלה: 1. בגיר החולה ב-ITP (immune thrombocytopenic purpura) כרונית או עיקשת (Persistent) הסובל מתרומבוציטופניה קשה (ספירת טסיות נמוכה מ-30,000) לאחר מיצוי טיפול בסטרואידים או אימונוגלובולינים. 2. ילד עד גיל 18 שנים החולה ב- ITP (immune thrombocytopenic purpura) כרונית או עיקשת (Persistent) הסובל מתרומבוציטופניה קשה (ספירת טסיות נמוכה מ-30,000) לאחר מיצוי טיפול בסטרואידים או אימונוגלובולינים. תחילת הטיפול בתרופה ייעשה לפי מרשם של רופא מומחה בהמטולוגיה או המטולוגיה ילדים. | 03/02/2022 | המטולוגיה | Immune thrombocytopenic purpura, ITP |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
23/01/2011
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
