Quest for the right Drug
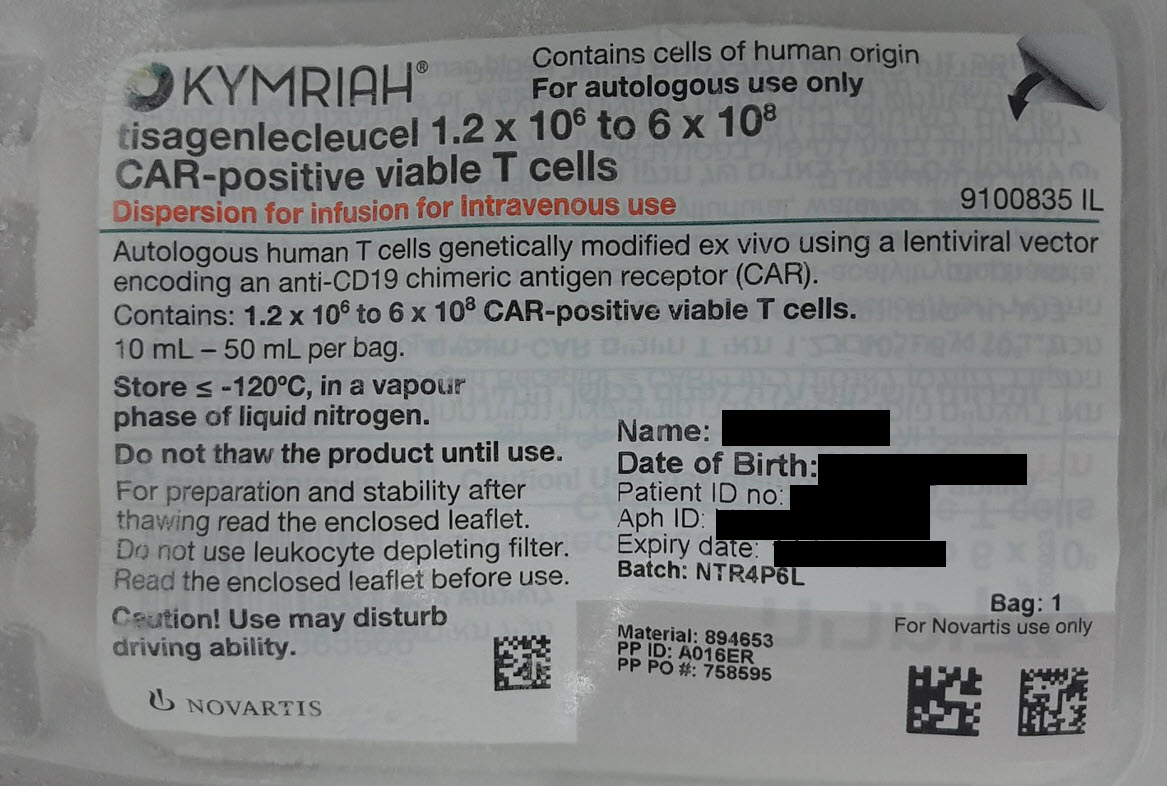
קימריה KYMRIAH (TISAGENLECLEUCEL)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אין פרטים : DISPERSION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Traceability The traceability requirements of cell-based advanced therapy medicinal products must apply. To ensure traceability the name of the medicinal product, the batch number and the name of the treated patient must be kept for a period of 30 years after expiry date of the medicinal product. Autologous use Kymriah is intended solely for autologous use and must not, under any circumstances, be administered to other patients. Kymriah must not be administered if the information on the product labels and batch specific documentation do not match the patient’s identity Reasons to delay treatment Due to the risks associated with tisagenlecleucel treatment, infusion should be delayed if a patient has any of the following conditions: - Unresolved serious adverse reactions (especially pulmonary reactions, cardiac reactions or hypotension) from preceding chemotherapies. - Active uncontrolled infection. - Active graft-versus-host disease (GVHD). - Significant clinical worsening of leukaemia burden or rapid progression of lymphoma following lymphodepleting chemotherapy. Transmission of an infectious agent Although Kymriah is tested for sterility and mycoplasma, a risk of transmission of infectious agents exists. Healthcare professionals administering Kymriah must, therefore, monitor patients for signs and symptoms of infections after treatment and treat appropriately, if needed. Blood, organ, tissue and cell donation Patients treated with Kymriah must not donate blood, organs, tissues or cells for transplantation. This information is provided in the Patient Alert Card which should be given to the patient after treatment. Active central nervous system (CNS) leukaemia or lymphoma There is limited experience of use of Kymriah in patients with active CNS leukaemia and active CNS lymphoma. Therefore, the risk/benefit of Kymriah has not been established in these populations. Kymriah is not indicated for treatment of patients with primary or secondary central nervous system lymphoma. Cytokine release syndrome Cytokine release syndrome, including fatal or life-threatening events, has been frequently observed after Kymriah infusion (see section 4.8). In almost all cases, development of cytokine release syndrome occurred between 1 to 10 days (median onset 3 days) after Kymriah infusion in paediatric and young adult B-cell ALL patients, between 1 and 9 days (median onset 3 days) after Kymriah infusion in adult DLBCL patients and between 1 to 14 days (median onset 4 days) after Kymriah infusion in adult FL patients. The median time to resolution of cytokine release syndrome was 8 days in B-cell ALL patients, 7 days in DLBCL patients and 4 days in FL patients. Symptoms of cytokine release syndrome may include high fever, rigors, myalgia, arthralgia, nausea, vomiting, diarrhoea, diaphoresis, rash, anorexia, fatigue, headache, hypotension, dyspnoea, tachypnoea, hypoxia, and tachycardia. Organ dysfunction, including cardiac insufficiency, renal insufficiency and liver injury with accompanying elevated aspartate aminotransferase (AST), elevated alanine aminotransferase (ALT) or elevated total bilirubin may also be observed. In some cases, disseminated intravascular coagulation (DIC) with low fibrinogen levels, capillary leak syndrome (CLS), macrophage activation syndrome (MAS) and haemophagocytic lymphohistiocytosis (HLH) may occur in the setting of cytokine release syndrome. Patients should be closely monitored for signs or symptoms of these events, including fever. Risk factors for severe cytokine release syndrome in paediatric and young adult B-cell ALL patients are: high pre-infusion tumour burden, uncontrolled or accelerating tumour burden following lymphodepleting chemotherapy, active infection and early onset of fever or cytokine release syndrome following Kymriah infusion. High tumour burden prior to Kymriah infusion was identified as a risk factor for developing severe cytokine release syndrome in adult DLBCL patients. Prior to administration of Kymriah in paediatric and young adult B-cell ALL patients, efforts should be made to lower and control the patient’s tumour burden. In all indications, appropriate prophylactic and therapeutic treatment for infections should be provided, and complete resolution of any existing infections should be ensured. Infections may also occur during cytokine release syndrome and may increase the risk of a fatal event. Management of cytokine release syndrome associated with Kymriah Cytokine release syndrome should be managed solely based on the patient’s clinical presentation and according to the cytokine release syndrome management algorithm provided in Table 1. Anti-IL-6 based therapy such as tocilizumab has been administered for moderate or severe cytokine release syndrome associated with Kymriah. One dose of tocilizumab per patient must be on site and available for administration prior to Kymriah infusion. The treatment centre should have access to additional doses of tocilizumab within 8 hours. In the exceptional case where tocilizumab is not available due to a shortage that is listed in the Ministry of Health website, the treatment centre must have access to suitable alternative measures instead of tocilizumab to treat CRS. Corticosteroids may be administered in cases of life-threatening emergencies. Tisagenlecleucel continues to expand and persist following administration of tocilizumab and corticosteroids. Patients with medically significant cardiac dysfunction should be managed by standards of critical care and measures such as echocardiography should be considered. Tumour necrosis factor (TNF) antagonists are not recommended for management of Kymriah-associated cytokine release syndrome. Table 1 Cytokine release syndrome management algorithm Cytokine release Symptomatic Tocilizumab Corticosteroids syndrome severity treatment Mild symptoms requiring Exclude other causes Not applicable Not applicable symptomatic treatment (e.g. infection) and only, e.g. treat specific symptoms - low fever with, for example, - fatigue antipyretics, anti- - anorexia emetics, analgesics, etc. If neutropenic, administer antibiotics per local guidelines Symptoms requiring Antipyretics, oxygen, moderate intervention: intravenous fluids - high fever and/or low-dose - hypoxia vasopressors as needed. - mild hypotension Treat other organ toxicities as per local guidance Symptom requiring High-flow oxygen If no improvement after If no improvement aggressive intervention: Intravenous fluids and symptomatic treatment, within 12-18 hours of - hypoxia requiring high-dose administer tocilizumab tocilizumab, administer high-flow oxygen vasopressor(s) intravenously over 1 hour: a daily dose of 2 mg/kg supplementation or Treat other organ - 8 mg/kg (max. 800 mg) intravenously - hypotension requiring toxicities as per local if body weight ≥30 kg methylprednisolone (or high-dose or multiple guidelines - 12 mg/kg if body weight equivalent) until vasopressors <30 kg vasopressor and Life-threatening Mechanical ventilation If no improvement, repeat oxygen no longer symptoms: Intravenous fluids and every 8 hours (max total of needed, then taper* - haemodynamic high-dose 4 doses)* instability despite vasopressor(s) intravenous fluids Treat other organ and vasopressors toxicities as per local - worsening guidelines respiratory distress - rapid clinical deterioration * If no improvement after tocilizumab and steroids, consider other anti-cytokine and anti-T-cell therapies following institutional policy and published guidelines. Alternative cytokine release syndrome management strategies may be implemented based on appropriate institutional or academic guidelines. Neurological adverse reactions Neurological events, in particular encephalopathy, confusional state or delirium, occur frequently with Kymriah and can be severe or life-threatening (see section 4.8). Other manifestations included depressed level of consciousness, seizures, aphasia and speech disorder. The majority of neurological events occurred within 8 weeks following Kymriah infusion and were transient. The median time to onset of the first neurological events occurring at any time following Kymriah infusion was 9 days in B-cell ALL, 6 days in DLBCL, and 9 days in FL. The median time to resolution was 7 days for B-cell ALL, 13 days for DLBCL, and 2 days for FL. Neurological events can be concurrent with cytokine release syndrome, following resolution of cytokine release syndrome or in the absence of cytokine release syndrome. Patients should be monitored for neurological events. In case of neurological events, patients should be diagnostically worked up and managed depending on the underlying pathophysiology and in accordance with local standard of care. Infections and febrile neutropenia Patients with active, uncontrolled infection should not start Kymriah treatment until the infection is resolved. Prior to Kymriah infusion, infection prophylaxis should follow standard guidelines based on the degree of preceding immunosuppression. Serious infections, including life-threatening or fatal infections, in some cases with late onset, occurred frequently in patients after Kymriah infusion (see section 4.8). Patients should be monitored for signs and symptoms of infection and treated appropriately. As appropriate, prophylactic antibiotics should be administered and surveillance testing should be employed prior to and during treatment with Kymriah. Infections are known to complicate the course and management of concurrent cytokine release syndrome. The possibility of opportunistic infections of the central nervous system should be considered in patients with neurological adverse events and appropriate diagnostic evaluations should be performed. Febrile neutropenia was frequently observed in patients after Kymriah infusion (see section 4.8) and may be concurrent with cytokine release syndrome. In the event of febrile neutropenia, infection should be evaluated and managed appropriately with broad-spectrum antibiotics, fluids and other supportive care, as medically indicated. In patients achieving complete remission following Kymriah, resulting low immunoglobulin levels can increase the risk for infections. Attention to signs and symptoms of infection should be implemented according to age and standard specific guidelines. Prolonged cytopenias Patients may continue to exhibit cytopenias for several weeks following lymphodepleting chemotherapy and Kymriah infusion and should be managed according to standard guidelines. The majority of patients who had cytopenias at day 28 following Kymriah treatment resolved to Grade 2 or below within three months after treatment for paediatric ALL and DLBCL patients, and within six months for FL patients. Prolonged neutropenia has been associated with increased risk of infection. Myeloid growth factors, particularly granulocyte macrophage-colony stimulating factor (GM-CSF), have the potential to worsen cytokine release syndrome symptoms and are not recommended during the first 3 weeks after Kymriah infusion or until cytokine release syndrome has resolved. Secondary malignancies including of T-cell origin Patients treated with Kymriah may develop secondary malignancies or recurrence of their cancer. T- cell malignancies have been reported following treatment of haematological malignancies with a BCMA- or CD19-directed CAR T-cell therapy, including Kymriah. T-cell malignancies, including CAR-positive malignancies, have been reported within weeks and up to several years following administration of a CD19- or BCMA-directed CAR T-cell therapy. There have been fatal outcomes. Patiens should be monitored life-long for secondary malignancies. In the event that a secondary malignancy occurs, the company should be contacted to obtain instructions on patient samples to collect for testing. Hypogammaglobulinaemia Hypogammaglobulinaemia and agammaglobulinaemia can occur in patients after Kymriah infusion. Immunoglobulin levels should be monitored after treatment with Kymriah. In patients with low immunoglobulin levels pre-emptive measures such as infection precautions, antibiotic prophylaxis and immunoglobulin replacement should be taken according to age and standard guidelines. Tumour lysis syndrome (TLS) TLS, which may be severe, has occasionally been observed. To minimise risk of TLS, patients with elevated uric acid or high tumour burden should receive allopurinol, or an alternative prophylaxis, prior to Kymriah infusion. Signs and symptoms of TLS should be monitored and events managed according to standard guidelines. Concomitant disease Patients with a history of active CNS disorder or inadequate renal, hepatic, pulmonary or cardiac function were excluded from the studies. These patient are likely to be more vulnerable to the consequences of the adverse reactions described below and require special attention. Prior stem cell transplantation It is not recommended that patients receive Kymriah within 4 months of undergoing an allogeneic stem cell transplant (SCT) because of the potential risk of Kymriah worsening GVHD. Leukapheresis for Kymriah manufacturing should be performed at least 12 weeks after allogeneic SCT. Serological testing There is currently no experience with manufacturing Kymriah for patients testing positive for HBV, HCV and HIV. Screening for HBV, HCV and HIV must be performed in accordance with clinical guidelines before collection of cells for manufacturing. Hepatitis B virus (HBV) reactivation, can occur in patients treated with medicinal products directed against B cells and could result in fulminant hepatitis, hepatic failure and death. Prior treatment with anti-CD19 therapy There is limited experience with Kymriah in patients exposed to prior CD19-directed therapy. While activity of tisagenlecleucel has been observed, data are currently too limited to make an adequate assessment of the benefit-risk profile in these patients. Kymriah is not recommended if the patient has relapsed with CD19-negative leukaemia after prior anti-CD19 therapy. Interference with virological testing Due to limited and short spans of identical genetic information between the lentiviral vector used to create Kymriah and HIV, some commercial HIV nucleic acid tests (NAT) may give a false positive result. Hypersensitivity reactions Serious hypersensitivity reactions, including anaphylaxis, may be due to dimethyl sulfoxide (DMSO) and dextran 40 in Kymriah. All patients should be observed closely during the infusion period. Long-term follow-up Patients are expected to be enrolled in a registry in order to better understand the long-term safety and efficacy of Kymriah. Sodium and potassium content This medicinal product contains 24.3 to 121.5 mg sodium per dose, equivalent to 1 to 6% of the WHO recommended maximum daily intake of 2 g sodium for an adult. This medicinal product contains potassium, less than 1 mmol (39 mg) per dose, i.e. essentially “potassium-free”.
Effects on Driving
4.7 Effects on ability to drive and use machines Kymriah has major influence on the ability to drive and use machines. Due to the potential for neurological events, including altered mental status or seizures, patients receiving Kymriah are at risk for altered or decreased consciousness or coordination and must refrain from driving or operating heavy or potentially dangerous machines for 8 weeks following Kymriah infusion.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. ילדים ומבוגרים צעירים שמלאו להם 3 שנים וטרם מלאו להם 25 שנים החולים בלוקמיה חוזרת או עמידה (רפרקטורית) מסוג CD19+ B cell Acute Lymphoblastic Leukemia (ALL).לעניין זה מחלה חוזרת תוגדר בחולה שקיבל שני קווי טיפול קודמים או שעבר השתלה של תאי גזע המטופואטיים.במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Brexucabtagene autoleucel, Tisagenlecleucel. 2. מבוגרים החולים בלימפומה חוזרת או עמידה (רפרקטורית) מסוג Diffuse large B cell lymphoma, לאחר שני קווי טיפול ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. 3. מבוגרים החולים בלימפומה פוליקולרית חוזרת או רפרקטורית לאחר שלושה קווי טיפול קודמים ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| מבוגרים החולים בלימפומה חוזרת או עמידה (רפרקטורית) מסוג Diffuse large B cell lymphoma, לאחר שני קווי טיפול ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. | 16/01/2019 | המטולוגיה | DLBCL, Diffusa large B cell lymphoma | |
| ילדים ומבוגרים צעירים שמלאו להם 3 שנים וטרם מלאו להם 25 שנים החולים בלוקמיה חוזרת או עמידה (רפרקטורית) מסוג CD19+ B cell Acute Lymphoblastic Leukemia (ALL). לעניין זה מחלה חוזרת תוגדר בחולה שקיבל שני קווי טיפול קודמים או שעבר השתלה של תאי גזע המטופואטיים. | 16/01/2019 | המטולוגיה | ALL, Acute lymphoblastic leukemia | |
| מבוגרים החולים בלימפומה פוליקולרית חוזרת או רפרקטורית לאחר שלושה קווי טיפול קודמים ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. | 01/02/2023 | המטולוגיה | לימפומה פוליקולרית, Follicular lymphoma | |
| ילדים ומבוגרים צעירים שמלאו להם 3 שנים וטרם מלאו להם 25 שנים החולים בלוקמיה חוזרת או עמידה (רפרקטורית) מסוג CD19+ B cell Acute Lymphoblastic Leukemia (ALL). לעניין זה מחלה חוזרת תוגדר בחולה שקיבל שני קווי טיפול קודמים או שעבר השתלה של תאי גזע המטופואטיים. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Brexucabtagene autoleucel, Tisagenlecleucel. | 01/02/2023 | המטולוגיה | ALL, Acute lymphoblastic leukemia |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
16/01/2019
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
ATC
מידע נוסף
עלון מידע לצרכן
05.04.22 - עלון לצרכן אנגלית 05.04.22 - עלון לצרכן עברית 05.04.22 - עלון לצרכן ערבית 05.04.22 - עלון לצרכן 02.05.22 - עלון לצרכן אנגלית 05.04.22 - עלון לצרכן אנגלית 05.04.22 - עלון לצרכן עברית 05.04.22 - עלון לצרכן ערבית 05.04.22 - עלון לצרכן 05.04.22 - עלון לצרכן אנגלית 16.12.21 - עלון לצרכן אנגלית 07.08.22 - עלון לצרכן עברית 16.12.21 - עלון לצרכן ערבית 11.10.22 - עלון לצרכן אנגלית 11.10.22 - עלון לצרכן עברית 11.10.22 - עלון לצרכן ערבית 18.12.22 - עלון לצרכן אנגלית 18.12.22 - עלון לצרכן עברית 18.12.22 - עלון לצרכן ערבית 18.12.22 - עלון לצרכן 18.12.22 - עלון לצרכן אנגלית 18.12.22 - עלון לצרכן אנגלית 09.01.23 - עלון לצרכן עברית 28.02.23 - עלון לצרכן אנגלית 28.02.23 - עלון לצרכן עברית 28.02.23 - עלון לצרכן ערבית 04.08.23 - עלון לצרכן עברית 07.09.23 - עלון לצרכן אנגלית 07.09.23 - עלון לצרכן עברית 07.09.23 - עלון לצרכן ערבית 16.08.24 - עלון לצרכן עברית 12.09.24 - עלון לצרכן אנגלית 12.09.24 - עלון לצרכן ערבית 10.02.20 - החמרה לעלון 09.06.21 - החמרה לעלון 22.11.21 - החמרה לעלון 07.08.22 - החמרה לעלון 05.09.22 - החמרה לעלון 09.01.23 - החמרה לעלון 04.08.23 - החמרה לעלון 28.12.23 - החמרה לעלון 19.08.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
קימריה