Quest for the right Drug
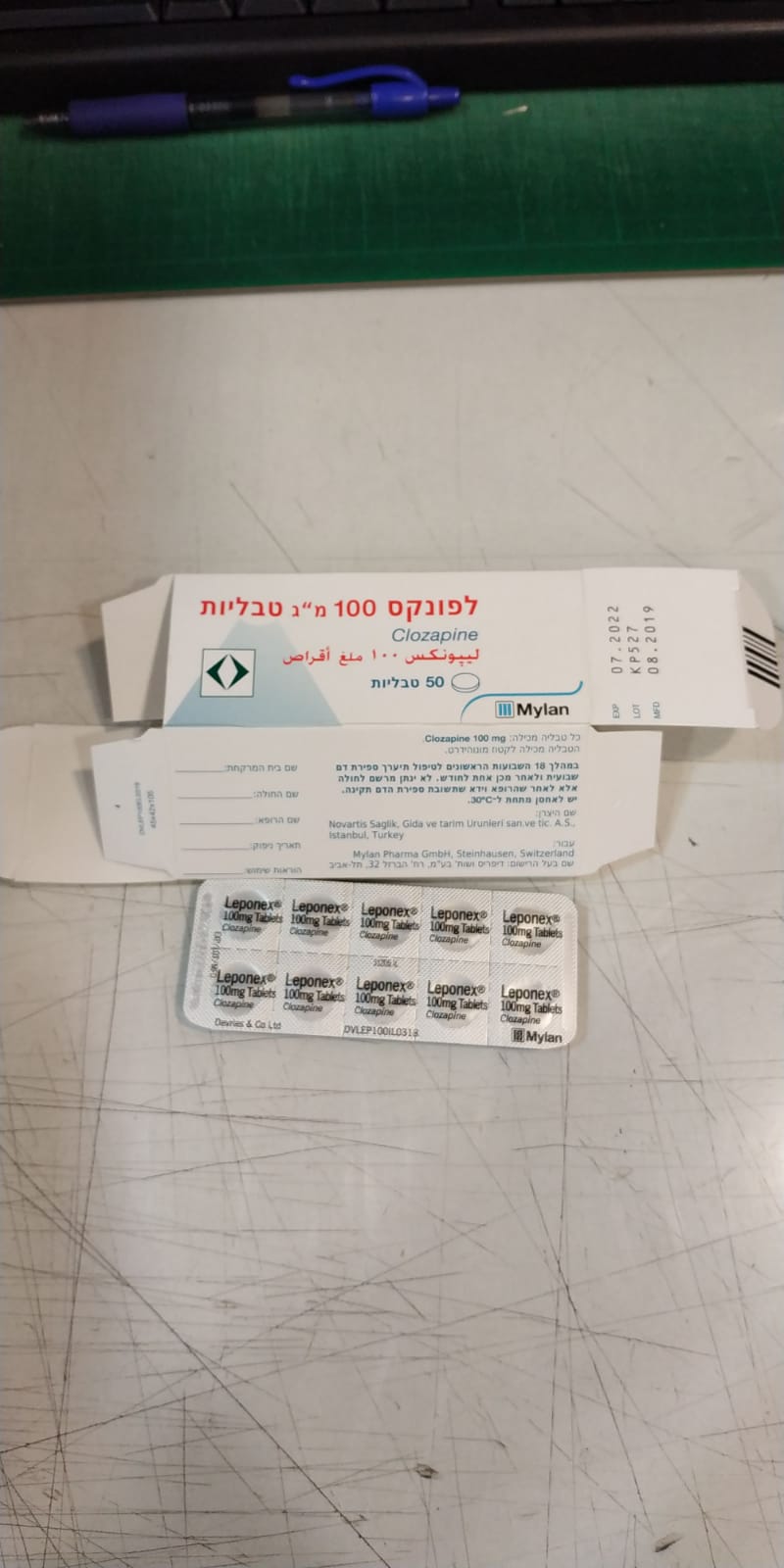
לפונקס 100 מ"ג טבליות LEPONEX 100 MG TABLETS (CLOZAPINE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Summary of the safety profile The most serious adverse reactions with clozapine are agranulocytosis, seizures, cardiovascular events and fever (see “Warnings and precautions”). The most common adverse effects are drowsiness/sedation, dizziness, tachycardia, constipation, nocturnal enuresis, hypersalivation (day and night) and sometimes also the appearance or exacerbation of obsessive symptoms. The data from clinical studies showed that a varying number of patients treated with clozapine (7.1 to 15.6%) discontinued treatment due to adverse effects. The most common adverse effects leading to treatment discontinuation were leukopenia, somnolence, dizziness (excluding vertigo) and psychotic disorders. The adverse reactions should be arranged according to MedDRA system organ classes and the conventional frequencies as follows: “very common” (≥ 1/10); “common” (≥ 1/100 to < 1/10); “uncommon” (≥ 1/1,000 to < 1/100); “rare” (≥ 1/10,000 to < 1/1,000); “very rare” (< 1/10,000), “not known” (frequency cannot be estimated from the available data). Blood and lymphatic system disorders Common: Leukopenia, decreased white blood cell (WBC), neutropenia. Uncommon: Agranulocytosis. Rare: Lymphopenia. Very rare: Thrombocytopenia, thrombocytosis, anaemia. There is a risk of granulocytopenia and/or agranulocytosis during Leponex therapy. Although generally reversible upon stopping treatment, agranulocytosis may result in sepsis and prove fatal. The majority of cases of agranulocytosis (approx. 70%) occur during the first 18 weeks of therapy. Prompt discontinuation of Leponex treatment is required to prevent the development of life- threatening agranulocytosis. Regular monitoring of the white blood cell (WBC) count is therefore mandatory (see “Special precautions”). Unexplained leukocytosis and/or eosinophilia may occur, particularly during the first few weeks of Leponex treatment. Metabolism and nutrition disorders Common to very common: Weight gain (4 to 31%), which may be substantial. Rare: Impaired glucose tolerance and diabetes mellitus, even in patients with no prior history of hyperglycaemia or diabetes mellitus. Very rare: Severe hyperglycaemia, sometimes leading to ketoacidosis or hyperosmolar coma, even in patients with no prior history of hyperglycaemia or diabetes mellitus; hypertriglyceridaemia, hypercholesterolaemia. Psychiatric disorders Common: Dysarthria. Uncommon: Stuttering (dysphemia). Rare: Restlessness, agitation. Very rare: Obsessive-compulsive disorders. Nervous system disorders Very common: Drowsiness and sedation (39 to 46%), dizziness (19 to 27%, with or without light-headedness). Common: Headache, tremor, rigor, akathisia, extrapyramidal symptoms, seizures, convulsions, myoclonic jerks. Rare: Confusion, delirium. Leponex may cause EEG changes, including spike and wave complexes. It lowers the seizure threshold in a dose-dependent manner and may induce myoclonic jerks or generalised seizures. These symptoms are more likely to occur with rapid dose increase and in patients with pre-existing epilepsy. In such cases, the dose should be reduced and, if necessary, anticonvulsant therapy initiated. Carbamazepine should be avoided because of its potential to suppress bone marrow function; in the case of other anticonvulsant drugs, the possibility of a pharmacokinetic interaction should be considered. Fatal convulsions have been reported. Extrapyramidal symptoms are milder and less frequent than those that occur with conventional antipsychotic agents. Acute dystonia has not been confirmed as an adverse effect of Leponex therapy. Very rarely, tardive dyskinesia has been reported in Leponex-treated patients who had been treated with other antipsychotic agents; a causal connection therefore cannot be established. Patients in whom tardive dyskinesia developed with other antipsychotic agents have improved on Leponex. There have been uncommon reports of neuroleptic malignant syndrome (NMS) in patients taking Leponex either alone or in combination with lithium or other centrally-acting agents. In such cases, the drug must be discontinued immediately and intensive care instituted. The main symptoms of NMS are: rigor, hyperthermia, mental changes and autonomic lability. Eye disorders Common: Blurred vision. Cardiac disorders Very common: Tachycardia (particularly in the first weeks of treatment with Leponex; 25%). Very rare: Cardiac arrest. ECG changes (ST segment depression, flattening and inversion of the T wave, conduction disturbances) may frequently occur. There have also been isolated reports of cases of arrhythmia, pericarditis (with or without pericardial effusion), cardiomyopathies and myocarditis (with or without eosinophilia), some of which proved fatal. The clinical symptoms may resemble those of myocardial infarction or influenza. The diagnosis of myocarditis should therefore be considered in patients on Leponex who develop resting tachycardia accompanied by arrhythmias, dyspnoea or symptoms of heart failure. The treatment should be discontinued if this diagnosis is confirmed. There have been very rare reports of cardiomyopathy. Leponex must be discontinued if cardiomyopathy is diagnosed. Vascular disorders Common: Hypertension, orthostatic hypotension, syncope. Rare: Thromboembolism, including fatal cases and cases occurring in combination with organ necrosis (e.g. intestine); circulatory collapse as a result of severe hypotension, especially in association with aggressive dose titration, with the potentially severe consequence of cardiac or respiratory arrest. The prevalence and severity of hypotension are affected by the rate and extent of dose increases. Respiratory, thoracic and mediastinal disorders Rare: Aspiration of ingested food (as a result of dysphagia). Very rare: Respiratory depression, respiratory arrest. Pneumonia and lower respiratory tract infections, which may be fatal, have been reported during treatment with Leponex. Gastrointestinal disorders Very common: Constipation (14 to 25%), hypersalivation (31 to 48%). Common: Nausea, vomiting, loss of appetite, dry mouth. Rare: Dysphagia. Very rare: Enlargement of the parotid gland, intestinal obstruction, paralytic ileus, faecal impaction. Hepatobiliary disorders Common: Elevated liver enzymes. Rare: Hepatitis, jaundice, acute pancreatitis. Very rare: Fulminant hepatic necrosis. If jaundice develops, Leponex must be discontinued immediately (see “Other precautions” under “Warnings and precautions”). Skin and subcutaneous tissue disorders Very rare: Skin reactions. Renal and urinary disorders Common: Urinary incontinence, urinary retention. Very rare: Tubulointerstitial nephritis, renal impairment, renal failure. Reproductive system and breast disorders Very rare: Priapism, impotence, changes in ejaculation, dysmenorrhoea. General disorders and administration site conditions Common: Fatigue, fever, benign hyperthermia, disturbances in sweating and temperature regulation. Investigations Rare: Elevated creatine phosphokinase (CPK). Very rare: Hyponatraemia. There have been very rare reports of ventricular tachycardia, cardiac arrest and QT prolongation, possibly associated with torsade de pointes, but there is no conclusive causal relationship to the use of this drug. Fatalities during treatment Unexpected sudden death is known to occur in psychiatric patients receiving conventional antipsychotic medication, but also in patients receiving no medication. Such cases of sudden death have occurred with Leponex, even in younger patients. There may be a connection with the cardiovascular adverse effects of Leponex (ECG changes, arrhythmias, cardiomyopathies, myocarditis). List of adverse drug reactions from post-marketing spontaneous reports (unknown frequency (cannot be estimated from the available data)) Infections and infestations Sepsis. Immune system disorders Drug rash with eosinophilia and systemic symptoms (DRESS), angioedema, leukocytoclastic vasculitis. Endocrine disorders Pseudophaeochromocytoma. Metabolism and nutrition disorders Obesity. Nervous system disorders Cholinergic symptoms, EEG changes, pleurothotonus (Pisa syndrome), restless legs syndrome (RLS). Cardiac disorders Myocardial infarction (sometimes with fatal outcome), myocarditis (sometimes with fatal outcome) chest pain / angina pectoris, palpitations, atrial fibrillation, mitral valve incompetence associated with Leponex-related cardiomyopathy. Vascular disorders Hypotension. Respiratory, thoracic and mediastinal disorders Bronchoconstriction, pleural effusion, sleep apnoea syndrome, nasal congestion. Gastrointestinal disorders Megacolon and intestinal infarction/ischaemia (sometimes with fatal outcome), as well as intestinal necrosis, intestinal ulceration and bowel perforation with a possible fatal outcome, diarrhoea, abdominal discomfort, heartburn, dyspepsia, colitis. Hepatobiliary disorders Hepatic steatosis, hepatic necrosis, hepatotoxicity, liver fibrosis, liver cirrhosis, liver damage with associated life-threatening consequences such as liver failure, liver transplant and even death. Skin and subcutaneous tissue disorders Pigmentation disorder. Musculoskeletal and connective tissue disorders Rhabdomyolysis, muscle weakness, muscle spasms, muscle pain, systemic lupus erythematosus. Renal and urinary disorders Renal failure, nocturnal enuresis. Reproductive system and breast disorders Retrograde ejaculation. General disorders and administration site conditions Polyserositis. Injury, poisoning and procedural complications Falls (associated with Leponex-induced seizures, somnolence, postural hypertonia and motor and sensory instability). Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form: https://sideeffects.health.gov.il

שימוש לפי פנקס קופ''ח כללית 1994
Schizophrenia in patients unresponsive to or intolerant of conventional antipsychotic drugs. התרופה תימצא רק בבתי חולים ותנופק לחולים אמבולטורים רק באמצעותם
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה אשפוזית לפי החלטת משרד הבריאות
מידע נוסף
