Quest for the right Drug
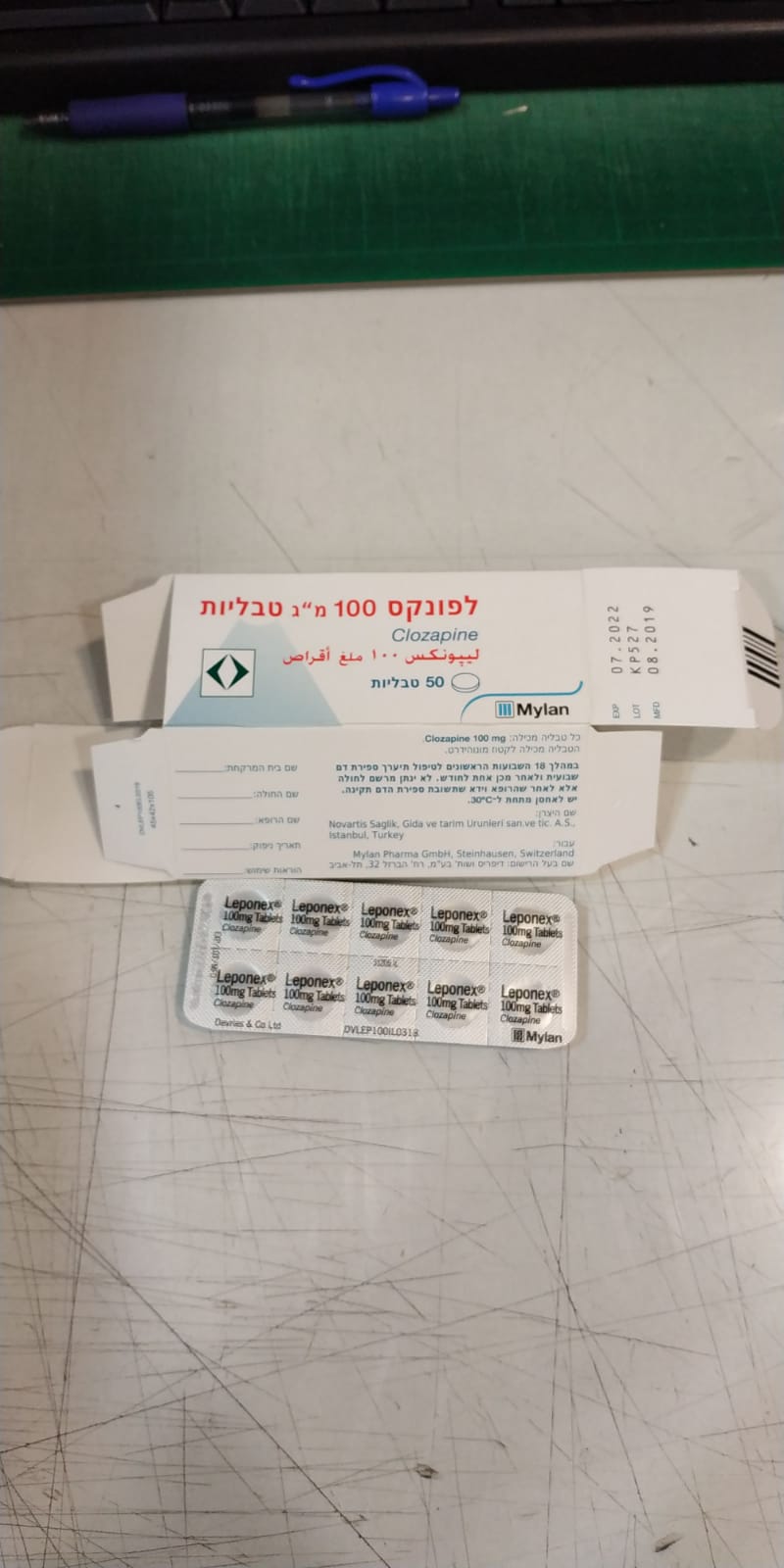
לפונקס 100 מ"ג טבליות LEPONEX 100 MG TABLETS (CLOZAPINE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Interactions : אינטראקציות
4.5 Interactions with other medicinal products and other forms of interaction Pharmacokinetic interactions Clozapine is a substrate for many CYP450 isoenzymes, in particular 3A4, 1A2 and 2D6. This should minimise the risk of metabolic interactions caused by an effect on an individual isoform. Nonetheless, plasma clozapine levels should be closely monitored in patients receiving concomitant treatment with other drugs having an affinity for one or more of these enzymes. Co-administration of substances that affect these isoenzymes may lead to a rise or fall in plasma levels of clozapine and/or the co-administered substances. Theoretically, clozapine may cause an increase in plasma levels of tricyclic antidepressants, phenothiazines and type-1c antiarrhythmic agents known to bind to cytochrome P450 2D6. It may be necessary to prescribe lower doses. However, no clinically-relevant interactions have been reported so far. The combination of Leponex with substances known to affect the activity of CYP450 isoenzymes may lead to a rise or fall in plasma levels of clozapine. Inhibitors: • The co-administration of enzyme inhibitors such as cimetidine (CYP1A2, 3A4 and 2D6 inhibitor) or erythromycin (CYP3A4 inhibitor), clarithromycin, azithromycin, fluvoxamine (1A2), perazine (1A2), ciprofloxacin (1A2) or oral contraceptives (1A2, 3A4, 2C19) with high doses of Leponex has been associated with elevated plasma clozapine levels and the occurrence of adverse effects. • There have been reports of increased plasma clozapine levels in patients who received the drug in combination with fluvoxamine (CYP3A4 and CYP1A2 inhibitor; up to ten- fold increase) or other selective serotonin reuptake inhibitors (SSRIs) such as paroxetine (CYP1A2, 2D6 inhibitor), sertraline (CYP2C8/9, 2D6 inhibitor), fluoxetine (CYP2D6 inhibitor, up to two-fold increase) or citalopram (possibly a weak CYP1A2 inhibitor with what is probably the lowest potential of all SSRIs for clinically-significant interactions). However, there have been reports of clinically-relevant interactions following co-administration of citalopram and clozapine. Increased concentrations of clozapine have also been observed in patients who received the drug in combination with venlafaxine. • Azole antimycotics and protease inhibitors are potent inhibitors/inducers of CYP3A4. They, too, may be expected to cause clinically-relevant interactions with clozapine. However, no interactions have been reported to date. Substrates: • Caffeine (substrate of CYP1A2) may raise plasma levels of clozapine. Plasma levels of clozapine fall by approx. 50% following a 5-day caffeine-free period. This should be kept in mind if there are changes in the consumption of tea or coffee. A significant increase in clozapine and N-desmethylclozapine was observed when concomitant treatment was given with 2 × 250 mg ciprofloxacin. There have also been reports of interactions with norfloxacin and enoxacin. Inducers: • Drugs that induce P450 CYP3A4 (e.g. carbamazepine and rifampicin) may reduce plasma clozapine levels. Withdrawal of concomitantly administered carbamazepine resulted in an increase in plasma clozapine levels. • Concomitant use of phenytoin has been found to decrease plasma clozapine levels, resulting in reduced efficacy of a previously effective Leponex dose. • Tobacco smoke induces CYP1A2. Sudden tobacco abstinence in heavy smokers may therefore lead to elevated plasma levels of clozapine and thus to increased adverse effects. • Omeprazole is an inducer of CYP1A2 and CYP3A4 and an inhibitor of CYP2C19. There have been isolated reports of interactions with proton pump inhibitors (decreased concentrations of clozapine when given with omeprazole and pantoprazole or with combinations of lansoprazole and paroxetine). Pharmacodynamic interactions Drugs with substantial myelosuppressive potential should not be used concomitantly with Leponex. Long-acting depot antipsychotics (which have myelosuppressive potential) should not be used concomitantly with Leponex because these substances cannot be rapidly removed from the body if required, e.g. in the event of neutropenia (see “Special precautions” under “Warnings and precautions”). Leponex may enhance the CNS effects of alcohol and MAO inhibitors as well as the CNS- depressant effects of narcotics, antihistamines and benzodiazepines. Fatalities have been reported for combinations of clozapine with such substances (including methadone). Particular caution is advised when giving Leponex concomitantly with benzodiazepines or other psychotropic agents as well as in patients who were using such drugs until only a few days before initiation of Leponex therapy. In such cases, there is an increased risk of circulatory collapse, which, on rare occasions, can be profound and may lead to cardiac or respiratory arrest. It is not clear whether cardiac or respiratory collapse can be prevented by dose adjustment. It is advisable to avoid administering benzodiazepines. If necessary – preferably short-term. Concomitant use of lithium or other CNS-acting drugs may increase the risk of neuroleptic malignant syndrome (NMS). Due to the possibility of additive effects, particular caution is required when concomitantly administering drugs possessing anticholinergic, antihypertensive or respiratory-depressant properties. Owing to its anti-alpha-adrenergic properties, Leponex may reduce the pressor effect of noradrenaline or other predominantly alpha-adrenergic agents and may reverse the pressor effect of adrenaline. Leponex may lower the seizure threshold and adjustment of the antiepileptic dosage may therefore be necessary. There have been rare reports of severe epileptic seizures, including first occurrence of seizures and isolated cases of delirium when Leponex was co- administered with valproic acid. These effects are possibly due to a pharmacodynamic interaction, the mechanism of which has not been determined. Due to the risk of epileptic convulsions and hematologic disorders, avoid administering medicines that lower the seizure threshold, such as maprotiline or buproprion concomitantly with clozapine. Leponex may increase plasma concentrations of highly protein-bound substances (e.g. warfarin and digoxin) due to their displacement from plasma proteins. If necessary, the dose of the protein-bound substance should be adjusted. As with other antipsychotic agents, caution is advised when prescribing Leponex in conjunction with medicinal products known to increase the QTc interval or cause an electrolyte imbalance. It is recommended to avoid administering medicines to lower blood pressure that are ACE inhibitors, antihistamines and barbiturates concomitantly with clozapine.

שימוש לפי פנקס קופ''ח כללית 1994
Schizophrenia in patients unresponsive to or intolerant of conventional antipsychotic drugs. התרופה תימצא רק בבתי חולים ותנופק לחולים אמבולטורים רק באמצעותם
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה אשפוזית לפי החלטת משרד הבריאות
מידע נוסף
