Quest for the right Drug
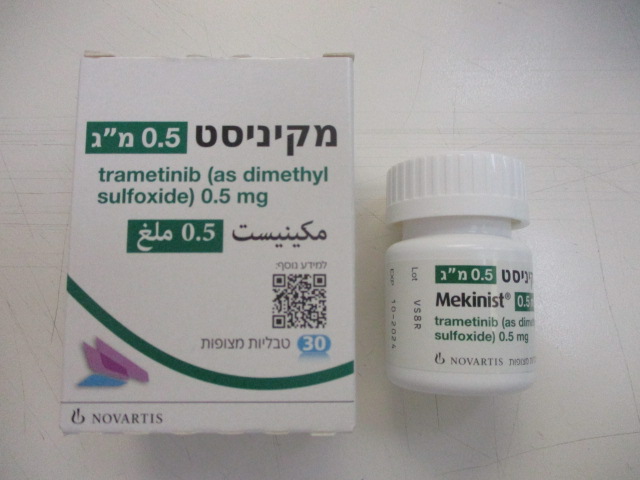
מקיניסט 0.5 מ"ג MEKINIST 0.5 MG (TRAMETINIB AS DIMETHYL SULFOXIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antineoplastic agents, protein kinase inhibitor, Mitogen-activated protein kinase (MEK) inhibitors, ATC code: L01EE01 Mechanism of action Trametinib is a reversible, highly selective, allosteric inhibitor of mitogen-activated extracellular signal regulated kinase 1 (MEK1) and MEK2 activation and kinase activity. MEK proteins are components of the extracellular signal-related kinase (ERK) pathway. In melanoma and other cancers, this pathway is often activated by mutated forms of BRAF which activates MEK. Trametinib inhibits activation of MEK by BRAF and inhibits MEK kinase activity. Trametinib inhibits growth of BRAF V600 mutant melanoma cell lines and demonstrates anti-tumour effects in BRAF V600 mutant melanoma animal models. In the setting of BRAF-mutant colorectal cancer, induction of EGFR-mediated MAPK pathway re- activation has been identified as a mechanism of intrinsic resistance to BRAF inhibitors (see section 4.1). Combination with dabrafenib Dabrafenib is an inhibitor of RAF kinases. Oncogenic mutations in BRAF lead to constitutive activation of the RAS/RAF/MEK/ERK pathway. Thus, trametinib and dabrafenib inhibit two kinases in this pathway, MEK and RAF, and therefore the combination provides concomitant inhibition of the pathway. The combination of trametinib with dabrafenib has shown anti-tumour activity in BRAF V600 mutation-positive melanoma cell lines in vitro and delays the emergence of resistance in vivo in BRAF V600 mutation-positive melanoma xenografts. Determination of BRAF mutation status Before taking trametinib or the combination with dabrafenib, patients must have BRAF V600 mutation-positive tumour status confirmed by a validated test. In clinical trials, central testing for BRAF V600 mutation using a BRAF mutation assay was conducted on the most recent tumour sample available. Primary tumour or tumour from a metastatic site was tested with a validated polymerase chain reaction (PCR) assay developed by Response Genetics Inc. The assay was specifically designed to differentiate between the V600E and V600K mutations. Only patients with BRAF V600E or V600K mutation-positive tumours were eligible for study participation. Subsequently, all patient samples were re-tested using the CE-marked bioMerieux (bMx) THxID BRAF validated assay. The bMx THxID BRAF assay is an allele-specific PCR performed on DNA extracted from FFPE tumour tissue. The assay was designed to detect the BRAF V600E and V600K mutations with high sensitivity (down to 5% V600E and V600K sequence in a background of wild- type sequence using DNA extracted from FFPE tissue). Non-clinical and clinical trials with retrospective bi-directional Sanger sequencing analyses have shown that the test also detects the less common BRAF V600D mutation and V600E/K601E mutation with lower sensitivity. Of the specimens from the non-clinical and clinical trials (n = 876) that were mutation-positive by the THxID BRAF assay and subsequently were sequenced using the reference method, the specificity of the assay was 94%. Pharmacodynamic effects Trametinib suppressed levels of phosphorylated ERK in BRAF mutant melanoma tumour cell lines and melanoma xenograft models. In patients with BRAF and NRAS mutation-positive melanoma, administration of trametinib resulted in dose-dependent changes in tumour biomarkers including inhibition of phosphorylated ERK, inhibition of Ki67 (a marker of cell proliferation) and increases in p27 (a marker of apoptosis). The mean trametinib concentrations observed following repeat dose administration of 2 mg once daily exceeds the preclinical target concentration over the 24-hr dosing interval, thereby providing sustained inhibition of the MEK pathway. Clinical efficacy and safety Unresectable or metastatic melanoma In the clinical trials only patients with cutaneous melanoma were studied. Efficacy in patients with ocular or mucosal melanoma has not been assessed. • Trametinib in combination with dabrafenib Treatment naïve patients The efficacy and safety of the recommended dose of trametinib (2 mg once daily) in combination with dabrafenib (150 mg twice daily) for the treatment of adult patients with unresectable or metastatic melanoma with a BRAF V600 mutation was studied in two Phase III studies and one supportive Phase I/II study. MEK115306 (COMBI-d): MEK115306 was a Phase III, randomised, double-blinded study comparing the combination of dabrafenib and trametinib to dabrafenib and placebo in first-line therapy for subjects with unresectable (Stage IIIC) or metastatic (Stage IV) BRAF V600E/K mutation-positive cutaneous melanoma. The primary endpoint of the study was progression-free survival (PFS), with a key secondary endpoint of overall survival (OS). Subjects were stratified by lactate dehydrogenase (LDH) level (> the upper limit of normal (ULN) versus ≤ULN) and BRAF mutation (V600E versus V600K). A total of 423 subjects were randomised 1:1 to either combination (N = 211) or dabrafenib (N = 212). Most subjects were Caucasian (>99%) and male (53%), with a median age of 56 years (28% were ≥65 years). The majority of subjects had Stage IVM1c disease (67%). Most subjects had LDH ≤ULN (65%), Eastern Cooperative Oncology Group (ECOG) performance status of 0 (72%), and visceral disease (73%) at baseline. The majority of subjects had a BRAF V600E mutation (85%). Subjects with brain metastases were not included in the trial. Median OS and estimated 1-year, 2-year, 3-year, 4-year and 5-year survival rates are presented in Table 12. From an OS analysis at 5 years, the median OS for the combination arm was approximately 7 months longer than for dabrafenib monotherapy (25.8 months versus 18.7 months) with 5-year survival rates of 32% for the combination versus 27% for dabrafenib monotherapy (Table 12, Figure 1). The Kaplan-Meier OS curve appears to stabilise from 3 to 5 years (see Figure 1). The 5-year overall survival rate was 40% (95% CI: 31.2, 48.4) in the combination arm versus 33% (95% CI: 25.0, 41.0) in the dabrafenib monotherapy arm for patients who had a normal lactate dehydrogenase level at baseline, and 16% (95% CI: 8.4, 26.0) in the combination arm versus 14% (95% CI: 6.8, 23.1) in the dabrafenib monotherapy arm for patients with an elevated lactate dehydrogenase level at baseline. Table 12. Overall Survival results for Study MEK115306 (COMBI-d) OS analysis 5-year OS analysis (data cut-off: 12-Jan-2015) (data cut-off: 10-Dec-2018) Dabrafenib + Dabrafenib + Dabrafenib + Dabrafenib+ Trametinib Placebo Trametinib Placebo (n=211) (n=212) (n=211) (n=212) Number of patients Died (event), n 99 (47) 123 (58) 135 (64) 151 (71) (%) Estimates of OS (months) 25.1 18.7 25.8 18.7 Median (95% CI) (19.2, NR) (15.2, 23.7) (19.2, 38.2) (15.2, 23.1) Hazard ratio 0.71 0.80 (95% CI) (0.55, 0.92) (0.63, 1.01) p-value 0.011 NA Overall survival Dabrafenib + Trametinib Dabrafenib + Placebo estimate, % (95% (n=211) (n=212) CI) At 1 year 74 (66.8, 79.0) 68 (60.8, 73.5) At 2 years 52 (44.7, 58.6) 42 (35.4, 48.9) At 3 years 43 (36.2, 50.1) 31 (25.1, 37.9) At 4 years 35 (28.2, 41.8) 29 (22.7, 35.2) At 5 years 32 (25.1, 38.3) 27 (20.7, 33.0) NR = Not reached, NA = Not applicable Figure 1 Kaplan-Meier overall survival curves for Study MEK115306 (ITT population) 1.0 Dabrafenib + Trametinib Dabrafenib + Placebo Estimated Survival Function 0.8 0.6 0.4 0.2 0.0 0 6 12 18 24 30 36 42 48 54 60 66 72 78 Time since Randomisation (Months) Subjects at Risk: Dabrafenib + Trametinib 211 188 145 113 98 86 79 71 63 60 57 54 12 0 Dabrafenib + Placebo 212 175 137 104 84 69 60 56 54 51 50 46 10 0 Improvements for the primary endpoint of PFS were sustained over a 5 year timeframe in the combination arm compared to dabrafenib monotherapy. Improvements were also observed for overall response rate (ORR) and a longer duration of response (DoR) was observed in the combination arm compared to dabrafenib monotherapy (Table 13). Table 13. Efficacy results for Study MEK115306 (COMBI-d) Primary analysis (data Updated analysis (data 5-year analysis (data cut-off: 26-Aug-2013) cut-off: 12-Jan-2015) cut-off: 10-Dec-2018) Endpoint Dabrafeni Dabrafeni Dabrafeni Dabrafenib Dabrafeni Dabrafeni b b b + b b + + + Placebo + + Trametini Placebo Trametini (n=212) Trametini Placebo b (n=211) (n=212) b (n=211) b (n=211) (n=212) PFSa Progressive disease or 102 (48) 109 (51) 139 (66) 162 (76) 160 (76) 166 (78) death, n (%) Median PFS (months) 9.3 8.8 11.0 8.8 10.2 8.8 (95% CI) (7.7, 11.1) (5.9, 10.9) (8.0, 13.9) (5.9, 9.3) (8.1, 12.8) (5.9, 9.3) Hazard Ratio 0.75 0.67 0.73 (95% CI) (0.57, 0.99) (0.53, 0.84) (0.59, 0.91) f P value 0.035 <0.001 NA ORRb 67 51 69 53 69 54 % (95% CI) (59.9, 73.0) (44.5, 58.4) (61.8, 74.8) (46.3, 60.2) (62.5, 75.4) (46.8, 60.6) ORR difference 15e 15e NA (95% CI) (5.9, 24.5) (6.0, 24.5) P value 0.0015 0.0014f NA DoR (months) c Median 9.2d 10.2d 12.9 10.6 12.9 10.2 (95% CI) (7.4, NR) (7.5, NR) (9.4,19.5) (9.1, 13.8) (9.3, 18.4) (8.3, 13.8) a – Progression-free survival (investigator assessed) b – Overall Response Rate = Complete Response + Partial Response c – Duration of response d – At the time of the reporting the majority (≥59%) of investigator-assessed responses were still ongoing. e – ORR difference calculated based on the ORR result not rounded f – Updated analysis was not pre-planned and the p-value was not adjusted for multiple testing NR = Not reached NA = Not applicable MEK116513 (COMBI-v): Study MEK116513 was a 2-arm, randomised, open-label, Phase III study comparing dabrafenib and trametinib combination therapy with vemurafenib monotherapy in BRAF V600 mutation-positive unresectable or metastatic melanoma. The primary endpoint of the study was OS with a key secondary endpoint of PFS. Subjects were stratified by lactate dehydrogenase (LDH) level (> the upper limit of normal (ULN) versus ≤ULN) and BRAF mutation (V600E versus V600K). A total of 704 subjects were randomised 1:1 to either combination or vemurafenib. Most subjects were Caucasian (>96%) and male (55%), with a median age of 55 years (24% were ≥65 years). The majority of subjects had Stage IV M1c disease (61% overall). Most subjects had LDH ≤ULN (67%), ECOG performance status of 0 (70%), and visceral disease (78%) at baseline. Overall, 54% of subjects had <3 disease sites at baseline. The majority of subjects had BRAF V600E mutation-positive melanoma (89%). Subjects with brain metastases were not included in the trial. Median OS and estimated 1-year, 2-year, 3-year, 4-year and 5-year survival rates are presented in Table 14. From an OS analysis at 5 years, the median OS for the combination arm was approximately 8 months longer than the median OS for vemurafenib monotherapy (26.0 months versus 17.8 months) with 5-year survival rates of 36% for the combination versus 23% for vemurafenib monotherapy (Table 14, Figure 2). The Kaplan-Meier OS curve appears to stabilise from 3 to 5 years (see Figure 2). The 5-year overall survival rate was 46% (95% CI: 38.8, 52.0) in the combination arm versus 28% (95% CI: 22.5, 34.6) in the vemurafenib monotherapy arm for patients who had a normal lactate dehydrogenase level at baseline, and 16% (95% CI: 9.3, 23.3) in the combination arm versus 10% (95% CI: 5.1, 17.4) in the vemurafenib monotherapy arm for patients with an elevated lactate dehydrogenase level at baseline. Table 14. Overall Survival results for Study MEK116513 (COMBI-v) OS analysis 5-year OS analysis data cut-off: 13-Mar-2015) (data cut-off: 08-Oct-2018) Dabrafenib + Dabrafenib + Vemurafenib Vemurafenib Trametinib Trametinib (n=352) (n=352) (n=352) (n=352) Number of patients Died (event), n 155 (44) 194 (55) 216 (61) 246 (70) (%) Estimates of OS (months) Median (95% CI) 25.6 18.0 26.0 17.8 (22.6, NR) (15.6, 20.7) (22.1, 33.8) (15.6, 20.7) Adjusted hazard 0.66 0.70 ratio (95% CI) (0.53, 0.81) (0.58, 0.84) p-value <0.001 NA Overall survival Dabrafenib + Trametinib Vemurafenib estimate, % (95% (n=352) (n=352) CI) At 1 year 72 (67, 77) 65 (59, 70) At 2 years 53 (47.1, 57.8) 39 (33.8, 44.5) At 3 years 44 (38.8, 49.4) 31 (25.9, 36.2) At 4 years 39 (33.4, 44.0) 26 (21.3, 31.0) At 5 years 36 (30.5, 40.9) 23 (18.1, 27.4) NR = Not reached, NA = Not applicable Figure 2 Kaplan-Meier curves Updated OS analysis for Study MEK116513 1.0 Dabrafenib + Trametinib Estimated Survival Function Vemurafenib 0.8 0.6 0.4 0.2 0.0 0 6 12 18 24 30 36 42 48 54 60 66 72 78 Time since Randomisation (Months) Subjects at Risk: Dabrafenib + Trametinib 352 311 246 201 171 151 140 130 118 109 104 49 4 0 Vemurafenib 352 287 201 154 120 104 94 86 78 72 65 30 1 0 Improvements for the secondary endpoint of PFS were sustained over a 5 year timeframe in the combination arm compared to vemurafenib monotherapy. Improvements were also observed for ORR and a longer DoR was observed in the combination arm compared to vemurafenib monotherapy (Table 15). Table 15. Efficacy results for Study MEK116513 (COMBI-v) Primary analysis (Data cut-off: 17- 5-year analysis (Data cut-off: 08- Apr-2014) Oct-2018) Endpoint Dabrafenib + Vemurafenib Dabrafenib + Vemurafenib Trametinib (n=352) Trametinib (n=352) (n=352) (n=352) PFSa Progressive 166 (47) 217 (62) 257 (73) 259 (74) disease or death, n (%) Median PFS 11.4 7.3 12.1 7.3 (months) (9.9, 14.9) (5.8, 7.8) (9.7, 14.7) (6.0, 8.1) (95% CI) Hazard Ratio 0.56 0.62 (95% CI) (0.46, 0.69) (0.52, 0.74) P value <0.001 NA ORRb % 64 51 67 53 (95% CI) (59.1, 69.4) (46.1, 56.8) (62.2, 72.2) (47.2, 57.9) ORR difference 13 NA (95% CI) (5.7, 20.2) P value 0.0005 NA DoRc (months) Median 13.8d 7.5d 13.8 8.5 (95% CI) (11.0, NR) (7.3, 9.3) (11.3, 18.6) (7.4, 9.3) a – Progression-free survival (investigator assessed) b – Overall Response Rate = Complete Response + Partial Response c – Duration of response d – At the time of the reporting the majority (59% of dabrafenib+trametinib and 42% of vemurafenib) of investigator-assessed responses were still ongoing NR = Not reached NA = Not applicable Prior BRAF inhibitor therapy There are limited data in patients taking the combination of trametinib with dabrafenib who have progressed on a prior BRAF inhibitor. Part B of study BRF113220 included a cohort of 26 patients that had progressed on a BRAF inhibitor. The trametinib 2 mg once daily and dabrafenib 150 mg twice daily combination demonstrated limited clinical activity in patients who had progressed on a BRAF inhibitor (see section 4.4). The investigator-assessed confirmed response rate was 15% (95% CI: 4.4, 34.9) and the median PFS was 3.6 months (95% CI: 1.9, 5.2). Similar results were seen in the 45 patients who crossed over from dabrafenib monotherapy to the trametinib 2 mg once daily and dabrafenib 150 mg twice daily combination in Part C of this study. In these patients a 13% (95% CI: 5.0, 27.0) confirmed response rate was observed with a median PFS of 3.6 months (95% CI: 2, 4). Patients with brain metastases The efficacy and safety of trametinib in combination with dabrafenib in patients with BRAF mutation-positive melanoma that has metastasised to the brain was studied in a non-randomised, open-label, multicentre, Phase II study (COMBI-MB study). A total of 125 patients were enrolled into four cohorts: • Cohort A: patients with BRAF V600E mutant melanoma with asymptomatic brain metastases without prior local brain-directed therapy and ECOG performance status of 0 or 1. • Cohort B: patients with BRAF V600E mutant melanoma with asymptomatic brain metastases with prior local brain-directed therapy and ECOG performance status of 0 or1. • Cohort C: patients with BRAF V600D/K/R mutant melanoma with asymptomatic brain metastases, with or without prior local brain-directed therapy and ECOG performance status of 0 or 1. • Cohort D: patients with BRAF V600D/E/K/R mutant melanoma with symptomatic brain metastases, with or without prior local brain-directed therapy and ECOG performance status of 0 or 1 or 2. The primary endpoint of the study was intracranial response in Cohort A, defined as the percentage of patients with a confirmed intracranial response assessed by the investigator using modified Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1. Intracranial response assessed by the investigator in Cohorts B, C and D were secondary endpoints of the study. Due to small sample size reflected by wide 95% CIs, the results in Cohorts B, C, and D should be interpreted with caution. Efficacy results are summarised in Table 16. Table 16. Efficacy data by investigator assessment from COMBI-MB study All treated patients population Endpoints/ Cohort A Cohort B Cohort C Cohort D assessment N=76 N=16 N=16 N=17 Intracranial response rate, % (95 % CI) 59% 56% 44% 59% (47.3, 70.4) (29.9, 80.2) (19.8, 70.1) (32.9, 81.6) Duration of intracranial response, median, months (95% CI) 6.5 7.3 8.3 4.5 (4.9, 8.6) (3.6, 12.6) (1.3, 15.0) (2.8, 5.9) Overall response rate, % (95% CI) 59% 56% 44% 65% (47.3, 70.4) (29.9, 80.2) (19.8, 70.1) (38.3, 85.8) Progression-free survival, median, months (95% CI) 5.7 7.2 3.7 5.5 (5.3, 7.3) (4.7, 14.6) (1.7, 6.5) (3.7, 11.6) Overall survival, median, months (95% CI) 10.8 24.3 10.1 11.5 (8.7, 17.9) (7.9, NR) (4.6, 17.6) (6.8, 22.4) CI = Confidence Interval NR = Not reached • Trametinib monotherapy Treatment naïve patients The efficacy and safety of trametinib in patients with BRAF unresectable or metastatic mutant melanoma (V600E and V600K) were evaluated in a randomised open-label Phase III study (MEK114267 [METRIC]). Measurement of patients’ BRAF V600 mutation status was required. Patients (N = 322) who were treatment naïve or may have received one prior chemotherapy treatment in the metastatic setting [Intent to Treat (ITT) population] were randomised 2:1 to receive trametinib 2 mg once daily or chemotherapy (dacarbazine 1000 mg/m2 every 3 weeks or paclitaxel 175 mg/m2 every 3 weeks). Treatment for all patients continued until disease progression, death or withdrawal. The primary endpoint of the study was to evaluate the efficacy of trametinib compared to chemotherapy with respect to PFS in patients with advanced/metastatic BRAF V600E/K mutation- positive melanoma without a prior history of brain metastases (N = 273) which is considered the primary efficacy population. The secondary endpoints were PFS in the ITT population and OS, ORR, and DoR in the primary efficacy population and ITT population. Patients in the chemotherapy arm were allowed to cross-over to the trametinib arm after independent confirmation of progression. Of the patients with confirmed disease progression in the chemotherapy arm, a total of 51 (47%) crossed over to receive trametinib. Baseline characteristics were balanced between treatment groups in the primary efficacy population and the ITT population. In the ITT population, 54% of patients were male and all were Caucasian. The median age was 54 years (22% were ≥65 years); all patients had an ECOG performance score of 0 or 1; and 3 % had history of brain metastases. Most patients (87%) in the ITT population had BRAF V600E mutation and 12% of patients had BRAF V600K. Most patients (66%) received no prior chemotherapy for advanced or metastatic disease. The efficacy results in the primary efficacy population were consistent with those in the ITT population; therefore, only the efficacy data for the ITT population are presented in Table 17. Kaplan- Meier curves of investigator assessed OS (post-hoc analysis 20 May 2013) is presented in Figure 3. Table 17. Investigator assessed efficacy results (ITT population) Endpoint Trametinib Chemotherapya Progression-Free Survival (N = 214) (N = 108) Median PFS (months) 4.8 1.5 (95% CI) (4.3, 4.9) (1.4, 2.7) Hazard Ratio 0.45 (95% CI) (0.33, 0.63) P value <0.0001 Overall Response Rate (%) 22 8 ITT = Intent to Treat; PFS = Progression-free survival; CI = confidence interval. a Chemotherapy included patients on dacarbazine (DTIC) 1000 mg/m2 every 3 weeks or paclitaxel 175 mg/m2 every 3 weeks. The PFS result was consistent in the subgroup of patients with V600K mutation-positive melanoma (HR = 0.50; [95% CI: 0.18, 1.35], p=0.0788). An additional OS analysis was undertaken based upon the 20 May 2013 data cut, see Table 18. For October 2011, 47% of subjects had crossed over, while for May 2013, 65% of subjects had crossed over. Table 18. Survival data from the primary and post-hoc analyses Cut-off Treatment Number Median Hazard ratio Percent dates of deaths months OS (95% CI) survival at (%) (95% CI) 12 months (95% CI) October 26, Chemotherapy 29 (27) NR NR 2011 (n=108) 0.54 (0.32, 0.92) Trametinib 35 (16) NR NR (n=214) May 20, Chemotherapy 67 (62) 11.3 (7.2, 14.8) 50 (39,59) 2013 (n=108) 0.78 (0.57, 1.06) Trametinib 137 (64) 15.6 (14.0, 61(54, 67) (n=214) 17.4) NR=not reached Figure 3 Kaplan-Meier curves of overall survival (OS –ad hoc analysis 20 May 2013) Prior BRAF inhibitor therapy In a single-arm Phase II study, designed to evaluate the objective response rate, safety, and pharmacokinetics following dosing of trametinib at 2 mg once daily in patients with BRAF V600E, V600K, or V600D mutation-positive metastatic melanoma (MEK113583), two separate cohorts were enrolled: Cohort A: patients with prior treatment with a BRAF inhibitor either with or without other prior therapy, Cohort B: patients with at least 1 prior chemotherapy or immunotherapy, without prior treatment with a BRAF inhibitor. In Cohort A of this study, trametinib did not demonstrate clinical activity in patients who had progressed on a prior BRAF inhibitor therapy. Adjuvant treatment of Stage III melanoma BRF115532 (COMBI-AD) The efficacy and safety of trametinib in combination with dabrafenib were studied in a Phase III, multicentre, randomised, double-blind, placebo-controlled study in patients with Stage III (Stage IIIA [lymph node metastasis >1 mm], IIIB, or IIIC) cutaneous melanoma with a BRAF V600 E/K mutation, following complete resection. Patients were randomised 1:1 to receive either combination therapy (dabrafenib 150 mg twice daily and trametinib 2 mg once daily) or two placebos for a period of 12 months. Enrollment required complete resection of melanoma with complete lymphadenectomy within 12 weeks prior to randomisation. Any prior systemic anti-cancer treatment, including radiotherapy, was not allowed. Patients with a history of prior malignancy, if disease-free for at least 5 years, were eligible. Patients presenting with malignancies with confirmed activating RAS mutations were not eligible. Patients were stratified by BRAF mutation status (V600E versus V600K) and stage of disease prior to surgery using the American Joint Committee on Cancer (AJCC) 7th edition Melanoma Staging System (by Stage III sub-stage, indicating different levels of lymph node involvement and primary tumour size and ulceration). The primary endpoint was investigator-assessed relapse-free survival (RFS), defined as the time from randomisation to disease recurrence or death from any cause. Radiological tumour assessment was conducted every 3 months for the first two years and every 6 months thereafter, until first relapse was observed. Secondary endpoints include overall survival (OS; key secondary endpoint), freedom from relapse (FFR) and distant metastasis-free survival (DMFS). A total of 870 patients were randomised to the combination therapy (n=438) and placebo (n=432) arms. Most patients were Caucasian (99%) and male (55%), with a median age of 51 years (18% were ≥65 years). The study included patients with all sub-stages of Stage III disease prior to resection; 18% of these patients had lymph node involvement only identifiable by microscope and no primary tumour ulceration. The majority of patients had a BRAF V600E mutation (91%). The median duration of follow-up at the time of the primary analysis was 2.83 years in the dabrafenib and trametinib combination arm and 2.75 years in the placebo arm. Results for the primary analysis of RFS are presented in Table 19. The study showed a statistically significant difference for the primary outcome of investigator-assessed RFS between treatment arms, with a median RFS of 16.6 months for the placebo arm and not yet reached for the combination arm (HR: 0.47; 95% confidence interval: (0.39, 0.58); p=1.53×10-14). The observed RFS benefit was consistently demonstrated across subgroups of patients including age, sex and race. Results were also consistent across stratification factors for disease stage and BRAF V600 mutation type. Table 19. Investigator-assessed RFS results for Study BRF115532 (COMBI-AD primary analysis) Dabrafenib + Trametinib Placebo RFS parameter N=438 N=432 Number of events, n (%) 166 (38%) 248 (57%) Recurrence 163 (37%) 247 (57%) Relapsed with distant metastasis 103 (24%) 133 (31%) Death 3 (<1%) 1 (<1%) Median (months) NE 16.6 (95% CI) (44.5, NE) (12.7, 22.1) Hazard ratio[1] 0.47 (95% CI) (0.39, 0.58) p-value[2] 1.53×10-14 1-year rate (95% CI) 0.88 (0.85, 0.91) 0.56 (0.51, 0.61) 2-year rate (95% CI) 0.67 (0.63, 0.72) 0.44 (0.40, 0.49) 3-year rate (95% CI) 0.58 (0.54, 0.64) 0.39 (0.35, 0.44) [1] Hazard ratio is obtained from the stratified Pike model. [2] P-value is obtained from the two-sided stratified log-rank test (stratification factors were disease stage – IIIA vs. IIIB vs. IIIC – and BRAF V600 mutation type – V600E vs. V600K) NE = not estimable Based on updated data with an additional 29 months of follow-up compared to the primary analysis (minimum follow-up of 59 months), the RFS benefit was maintained with an estimated HR of 0.51 (95% CI: 0.42, 0.61) (Figure 4). The 5-year RFS rate was 52% (95% CI: 48, 58) in the combination arm compared to 36% (95% CI: 32, 41) in the placebo arm. Figure 4 Kaplan-Meier RFS curves for Study BRF115532 (ITT population, updated results) At the time of the final OS analysis, the median duration of follow-up was 8.3 years in the combination arm and 6.9 years in the placebo arm. The observed difference in OS was not statistically significant (HR: 0.80; 95% CI: 0.62, 1.01) with 125 events (29%) in the combination arm and 136 events (31%) in the placebo arm. Estimated 5-year OS rates were 79% in the combination arm and 70% in the placebo arm, and estimated 10-year OS rates were 66% in the combination arm and 63% in the placebo arm. Non-small cell lung cancer Study BRF113928 The efficacy and safety of trametinib in combination with dabrafenib was studied in a Phase II, three-cohort, multicentre, non-randomised and open-label study in which patients with Stage IV BRAF V600E mutant NSCLC were enrolled. The primary endpoint was ORR using the RECIST 1.1 assessed by the investigator. Secondary endpoints included DoR, PFS, OS, safety and population pharmacokinetics. ORR, DoR and PFS were also assessed by an Independent Review Committee (IRC) as a sensitivity analysis. Cohorts were enrolled sequentially: • Cohort A: Monotherapy (dabrafenib 150 mg twice daily), 84 patients enrolled. 78 patients had previous systemic treatment for their metastatic disease. • Cohort B: Combination therapy (dabrafenib 150 mg twice daily and trametinib 2 mg once daily), 59 patients enrolled. 57 patients had 1-3 lines of previous systemic treatment for their metastatic disease. 2 patients had no previous systemic treatment and were included in the analysis for patients enrolled in Cohort C. • Cohort C: Combination therapy (dabrafenib 150 mg twice daily and trametinib 2 mg once daily), 34 patients. All patients received study medicinal product as first-line treatment for metastatic disease. Among the total of 93 patients who were enrolled in the combination therapy cohorts B and C, most patients were Caucasian (>90%), and similar female versus male (54% versus 46%), with a median age of 64 years in second line or higher patients and 68 years in the first line patients. Most patients (94%) enrolled in the combination- therapy- treated cohorts had an ECOG performance status of 0 or 1. 26 (28%) had never smoked. The majority of patients had a non-squamous histology. In the previously- treated population, 38 patients (67%) had one line of systemic anti-cancer therapy for metastatic disease. At the time of the primary analysis, the primary endpoint of investigator-assessed ORR, in the first line population was 61.1% (95% CI, 43.5%, 76.9%) and in the previously-treated population was 66.7% (95% CI, 52.9%, 78.6%). These met the statistical significance to reject the null hypothesis that the ORR of dabrafenib in combination with trametinib for this NSCLC population was less than or equal to 30%. The ORR results assessed by IRC were consistent with the investigator assessment. The final analysis of efficacy performed 5 years after last subject first dose is presented in Table 20. Table 20. Summary of efficacy in the combination treatment cohorts based on investigator and independent radiology review Endpoint Analysis Combination 1st Line Combination 2nd Line Plus N=361 N=571 Overall confirmed By Investigator 23 (63.9%) 39 (68.4%) response n (%) (46.2, 79.2) (54.8, 80.1) (95% CI) By IRC 23 (63.9%) 36 (63.2%) (46.2, 79.2)) (49.3, 75.6) Median DoR By Investigator 10.2 (8.3, 15.2)15.2 (7.8, 9.8 (6.9, 18.3) Months (95% CI) By IRC 23.5) 12.6 (5.8, 26.2) Median PFS By Investigator 10.8 (7.0, 14.5) 10.2 (6.9, 16.7) Months (95% CI) By IRC 14.6 (7.0, 22.1) 8.6 (5.2, 16.8) Median OS - 17.3 (12.3, 40.2) 18.2 (14.3, 28.6) Months (95% CI) 1 Data cut-off: 7 January 2021 Other studies - pyrexia management analysis Study CPDR001F2301 (COMBI-i) and Study CDRB436F2410 (COMBI-Aplus) Pyrexia is observed in patients treated with dabrafenib and trametinib combination therapy. The initial registration studies for the combination therapy in the unresectable or metastatic melanoma setting (COMBI-d and COMBI-v; total N=559) and in the adjuvant melanoma setting (COMBI-AD, N=435) recommended to interrupt only dabrafenib in case of pyrexia (fever ≥38.5°C). In two subsequent studies in unresectable or metastatic melanoma (COMBI-i control arm, N=264) and in the adjuvant melanoma setting (COMBI-Aplus, N=552), interruption of both medicinal products when patient’s temperature is ≥38oC (COMBI-Aplus), or at the first symptom of pyrexia (COMBI-i; COMBI-Aplus for recurrent pyrexia) was advised. In COMBI-i and COMBI-Aplus there was a lower incidence of grade 3/4 pyrexia, complicated pyrexia, hospitalisation due to serious pyrexia adverse events of special interest (AESIs), the time spent in pyrexia AESIs, and permanent discontinuations from both medicinal products due to pyrexia AESIs (the latter in the adjuvant setting only) compared to COMBI- d, COMBI-v and COMBI-AD. The COMBI-Aplus study met its primary endpoint with a composite rate of 8.0% (95% CI: 5.9, 10.6) for grade 3/4 pyrexia, hospitalisation due to pyrexia, or permanent treatment discontinuation due to pyrexia compared to 20.0% (95% CI: 16.3, 24.1) for the historical control (COMBI-AD). Anaplastic Thyroid Cancer (ATC) The safety and efficacy of trametinib administered with dabrafenib was evaluated in an activity- estimating, nine-cohort, multi-center, non-randomized, open-label trial (Study BRF117019; NCT02034110) in patients with rare cancers with the BRAF V600E mutation, including locally advanced, unresectable, or metastatic anaplastic thyroid cancer (ATC) with no standard locoregional treatment options. Trial BRF117019 excluded patients who could not swallow or retain the medication; who received prior treatment with BRAF or MEK inhibitors; with symptomatic or untreated CNS metastases; or who had airway obstruction. Patients received trametinib 2 mg once daily and dabrafenib 150 mg twice daily. The major efficacy outcome measure was overall response rate (ORR) per RECIST v1.1 as assessed by independent review committee (IRC) and duration of response (DoR). Thirty-six patients were enrolled and were evaluable for response in the ATC cohort. The median age was 71 years (range 47-85); 44% were male, 50% White, 44% Asian; and 94% had ECOG performance status of 0 or 1. Prior anti-cancer treatments included surgery and external beam radiotherapy (83% each), and systemic therapy (67%). Efficacy results are summarized in Table 21. Table 21. Efficacy Results in the ATC Cohort Based on Independent Review of Study BRF117019 ATC Cohort Population N = 36 Overall Response Rate ORR (95%CI) 53% (35.5%, 69.6%) Complete response 6% Partial response 47% Duration of Response n = 19 Median DoR, months (95% CI) 13.6 (3.8, NE) % with DoR ≥6 months 68% % with DoR ≥ 12 months 53% Abbreviations: ATC, anaplastic thyroid cancer; CI, confidence interval; DoR, duration of response; ORR, overall response rate; NE, not estimable. BRAF V600E Mutation-Positive Unresectable or Metastatic Solid Tumors The safety and efficacy of trametinib in combination with dabrafenib for the treatment of BRAF V600E mutation-positive unresectable or metastatic solid tumors were evaluated in Trials BRF117019, NCI-MATCH, and CTMT212X2101, and supported by results in COMBI-d, COMBI-v, and BRF113928. In adult studies, patients received trametinib 2 mg once daily and dabrafenib 150 mg twice daily. The major efficacy outcome measures were ORR per RECIST v1.1, RANO [HGG] or modified RANO [LGG] criteria and duration of response (DoR). BRF117019 Study and NCI-MATCH Study Study BRF117019 (NCT02034110) is a multi-cohort, multi-center, non-randomized, open-label trial in adult patients with selected tumors with the BRAF V600E mutation, including high grade glioma (HGG) (n = 45), biliary tract cancer (BTC) (n = 43), low grade glioma (LGG) (n = 13), adenocarcinoma of small intestine (ASI) (n = 3), gastrointestinal stromal tumor (GIST) (n = 1), and anaplastic thyroid cancer. Patients were enrolled based on local assessments of BRAF V600E mutation status; a central laboratory confirmed the BRAF V600E mutation in 93 of 105 patients. Arm H (EAY131-H) of the NCI-MATCH study (NCT02465060) is a single-arm, open-label study that enrolled patients with a BRAF V600E mutation. Patients with melanoma, thyroid cancer, or CRC were excluded. BRAF mutation status for enrollment was determined either by central or local laboratory test. The study included adult patients with solid tumors including gastrointestinal tumors (n = 14), lung tumors (n = 7), gynecologic or peritoneal tumors (n = 6), CNS tumors (n = 4), and ameloblastoma of mandible (n = 1). Among the 131 patients enrolled in BRF117019 and NCI-MATCH with the tumor types shown in Table 22, the baseline characteristics were: median age of 51 years with 20% age 65 or older; 56% female; 85% White, 9% Asian, 3% Black, 3% Other; and 37% ECOG 0, 56% ECOG 1, and 6% ECOG 2. Of the 131 patients, 90% received prior systemic therapy. Efficacy results in patients with solid tumors are summarized in Table 22. Table 22. Efficacy Results Based on Independent Review in Study BRF117019 and NCI MATCH Arm H Objective Response Rate Duration of Response Tumor Typea N % 95% CI Range (months) b Biliary tract cancer 48 46 (31, 61) 1.8d, 40d High grade gliomac 48 33 (20, 48) 3.9, 44 Glioblastoma 32 25 (12, 43) 3.9, 27 Anaplastic pleomorphic 6, 43 6 67 (22, 96) xanthoastrocytoma Anaplastic astrocytoma 5 20 (0.5, 72) 15 Astroblastoma 2 100 (16, 100) 15, 23d Undifferentiated 1 PR (2.5, 100) 6 Anaplastic ganglioglioma 1 0 NA NA Anaplastic oligodendroglioma 1 0 NA NA Low grade glioma 14 50 (23, 77) 6, 29d Astrocytoma 4 50 (7, 93) 7, 23 Ganglioglioma 4 50 (7, 93) 6, 13 Pleomorphic xanthoastrocytoma 2 50 (1.3, 99) 6 Pilocytic astrocytoma 2 0 NA NA Choroid plexus papilloma 1 PR (2.5, 100) 29d Gangliocytoma/ganglioglioma 1 PR (2.5, 100) 18d Low grade serous ovarian carcinoma 5 80 (28, 100) 12, 42d Adenocarcinoma small intestine 4 50 (7, 93) 7, 8 Adenocarcinoma pancreas 3 0 NA NA Mixed ductal / adenoneuroendocrine 2 0 NA NA carcinoma Neuroendocrine carcinoma of colon 2 0 NA NA Ameloblastoma of mandible 1 PR (2.5, 100) 30 Combined small cell-squamous 1 PR (2.5, 100) 5 carcinoma of lung Mucinous-papillary serous 1 PR (2.5, 100) 8 adenocarcinoma of peritoneum Adenocarcinoma of anus 1 0 NA NA Gastrointestinal stromal tumor 1 0 NA NA Abbreviations: PR, partial response. a Excludes NSCLC (n=6) and ATC (n=36) (previously approved tumor types for trametinib in combination with dabrafenib). b Median DoR 9.8 months (95% CI: 5.3, 20.4). c Median DoR 13.6 months (95% CI: 5.5, 26.7). d Denotes a right-censored DoR. CTMT212X2101 (X2101) Study Study X2101 (NCT02124772) was a multi-center, open-label, multi-cohort study in pediatric patients with refractory or recurrent solid tumors. Part C was a dose escalation of trametinib in combination with dabrafenib in patients with a BRAF V600E mutation. Part D was a cohort expansion phase of trametinib in combination with dabrafenib in patients with LGG with a BRAF V600E mutation. The major efficacy outcome measure was ORR as assessed by independent review committee per RANO criteria. The efficacy of trametinib in combination with dabrafenib was evaluated in 48 pediatric patients, including 34 patients with LGG and 2 patients with HGG. For patients with BRAF V600E mutant LGG in Parts C and D, the median age was 10 years (range: 1 to 17); 50% were male, 75% White, 8% Asian, 3% Black; and 58% had Karnofsky/Lansky performance status of 100. Prior anti-cancer treatments included surgery (83%), external beam radiotherapy (2.8%), and systemic therapy (92%). The ORR was 25% (95% CI: 12%, 42%). For the 9 patients who responded, DoR was ≥6 months for 78% of patients, and ≥24 months for 44% of patients. CDRB436G2201 (G2201) Study – High-Grade Glioma Cohort Study G2201 (NCT02684058) was a multi-center, randomized, open-label, Phase II study of dabrafenib and trametinib in chemotherapy naïve pediatric patients with BRAF V600E mutant low- grade glioma (LGG) and patients with relapsed or progressive BRAF V600E mutant HGG. Patients with HGG were enrolled in a single-arm cohort. The major efficacy outcome measure for the HGG cohort was ORR as assessed by independent review committee per RANO 2010 criteria. The efficacy of trametinib in combination with dabrafenib was evaluated in 41 pediatric patients with relapsed or progressive HGG. For patients with BRAF V600E mutant HGG enrolled in the HGG cohort, the median age was 13 years (range: 2 to 17); 56% were female, 61% White, 27% Asian, 2.4% Black and 37% had Karnofsky/Lansky performance status of 100. Prior anti-cancer treatments included surgery (98%), radiotherapy (90%), and chemotherapy (81%). The ORR was 56% (95% CI: 40, 72). The median DoR was not reached (95% CI: 9.2, NE). For the 23 patients who responded in the HGG cohort, DoR was ≥ 6 months for 78% of patients, ≥ 12 months for 48% of patients, and ≥ 24 months for 22% of patients. BRAF V600E Mutation-Positive Low-Grade Glioma CDRB436G2201 (G2201) Study – Low-Grade Glioma Cohort The safety and efficacy of trametinib in combination with dabrafenib for the treatment of BRAF V600E mutation-positive low-grade glioma (LGG) in pediatric patients aged 1 to < 18 years of age were evaluated in the multi-center, open-label trial (Study CDRB436G2201; NCT02684058). Patients with LGG (WHO grades 1 and 2) who required first systemic therapy were randomized in a 2:1 ratio to dabrafenib plus trametinib (D + T) or carboplatin plus vincristine (C + V). BRAF mutation status was identified prospectively via a local assessment or a central laboratory test. In addition, retrospective testing of available tumor samples by the central laboratory was performed to evaluate BRAF V600E mutation status. Patients received age- and weight-based dosing of trametinib and dabrafenib until loss of clinical benefit or until unacceptable toxicity. Carboplatin and vincristine were dosed based on body surface area at doses 175 mg/m2 and 1.5 mg/m2 (0.05 mg/kg for patients < 12 kg), respectively, as one 10- week induction course followed by eight 6-week cycles of maintenance therapy. The major efficacy outcome measure was overall response rate (ORR) by independent review based on RANO LGG (2017) criteria. Additional efficacy outcome measures were progression-free survival and overall survival. The primary analysis was performed when all patients had completed at least 32 weeks of therapy. In the LGG cohort, 110 patients were randomized to D + T (n = 73) or C + V (n = 37). Median age was 9.5 years (range: 1 to 17); 60% were female. Study G2201 showed a statistically significant improvement in ORR and PFS in patients with LGG randomized to D + T compared to those randomized to C + V. Efficacy results are shown in Table 23. Table 23. Efficacy Results Based on Independent Review in Study G2201 (LGG cohort) Trametinib plus Dabrafenib Carboplatin plus Vincristine N = 73 N = 37 Overall Response Rate ORR% (95% CI)a 46.6 (34.8, 58.6) 10.8 (3.0, 25.4) P value < 0.001 Complete response, n (%) 2 (2.7) 1 (2.7) Partial response, n (%) 32 (44) 3 (8) Duration of Response Median (95% CI)b, months 23.7 (14.5, NE) NE (6.6, NE) % with observed DoR ≥ 12 months 56 50 % with observed DoR ≥ 24 months 15 25 Progression-Free Survival Median (95% CI)b, months 20.1 (12.8, NE) 7.4 (3.6, 11.8) c Hazard ratio (95% CI) 0.31 (0.17, 0.55) P value < 0.001 Abbreviations: CI, confidence interval; NE, not estimable. a Based on Clopper-Pearson exact confidence interval b Based on Kaplan-Meier method c Based on proportional hazards model Figure 5. Kaplan-Meier Curves for Progression-Free Survival in Study G2201 (LGG cohort) At the time of the interim analysis of overall survival (OS), conducted when all patients had completed at least 32 weeks of treatment or had discontinued earlier, there was one death on the C + V arm. The OS results at interim analysis did not reach statistical significance.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption Trametinib is absorbed orally with median time to achieve peak concentrations of 1.5 hours post-dose. The mean absolute bioavailability of a single 2 mg tablet dose is 72% relative to an intravenous (IV) microdose. The increase in exposure (Cmax and AUC) was dose-proportional following repeat dosing. Following administration of 2 mg once daily, steady-state geometric mean Cmax, AUC(0-τ) and predose concentration were 22.2 ng/ml, 370 ng*hr/ml and 12.1 ng/ml, respectively with a low peak:trough ratio (1.8). Inter-subject variability at steady state was low (<28%). Trametinib accumulates with repeat daily dosing with a mean accumulation ratio of 6.0 at 2 mg once daily dose. Steady state was achieved by Day 15. Administration of a single dose of trametinib with a high-fat, high-calorie meal resulted in a 70% and 10% decrease in Cmax and AUC, respectively compared to fasted conditions (see sections 4.2 and 4.5). Distribution Binding of trametinib to human plasma proteins is 97.4%. Trametinib has a volume of distribution of approximately 1200 L determined following administration of a 5 µg intravenous microdose. Biotransformation In vitro and in vivo studies demonstrated that trametinib is metabolised predominantly via deacetylation alone or in combination with mono-oxygenation. The deacetylated metabolite was further metabolised by glucuronidation. CYP3A4 oxidation is considered a minor pathway of metabolism. The deacetylation is mediated by the carboxyl-esterases 1b, 1c and 2, with possible contributions by other hydrolytic enzymes. Following single and repeated doses of trametinib, trametinib as parent is the main circulating component in plasma. Elimination Mean terminal half-life is 127 hours (5.3 days) after single dose administration. Trametinib plasma IV clearance is 3.21 L/hr. Total dose recovery was low after a 10-day collection period (<50%) following administration of a single oral dose of radiolabelled trametinib as a solution, due to the long elimination half-life. Drug-related material was excreted predominantly in the faeces (>80% of recovered radioactivity) and to a minor extent in urine (≤19%). Less than 0.1% of the excreted dose was recovered as parent in urine. Special patient populations Hepatic impairment Population pharmacokinetic analyses and data from a clinical pharmacology study in patients with normal hepatic function or with mild, moderate or severe bilirubin and/or AST elevations (based on National Cancer Institute [NCI] classification) indicate that hepatic function does not significantly affect trametinib oral clearance. Renal impairment Renal impairment is unlikely to have a clinically relevant effect on trametinib pharmacokinetics given the low renal excretion of trametinib. The pharmacokinetics of trametinib were characterised in 223 patients enrolled in clinical trials with trametinib who had mild renal impairment and 35 patients with moderate renal impairment using a population pharmacokinetic analysis. Mild and moderate renal impairment had no effect on trametinib exposure (<6% for either group). No data are available in patients with severe renal impairment (see section 4.2). Elderly Based on the population pharmacokinetic analysis (range 19 to 92 years), age had no relevant clinical effect on trametinib pharmacokinetics. Safety data in patients ≥75 years is limited (see section 4.8). Race There are insufficient data to evaluate the potential effect of race on trametinib pharmacokinetics as clinical experience is limited to Caucasians. Pediatric Patients The pharmacokinetics of trametinib were evaluated in 95 pediatric patients after single or repeat weight-adjusted dosing. The pharmacokinetic exposures of trametinib at the recommended weight- adjusted dosage in pediatric patients were within range of those observed in adults. Body weight and gender Based on a population pharmacokinetic analysis, gender and body weight were found to influence trametinib oral clearance. Although smaller female subjects are predicted to have higher exposure than heavier male subjects, these differences are unlikely to be clinically relevant and no dosage adjustment is warranted in adults. Medicinal product interactions Effects of trametinib on drug-metabolising enzymes and transporters: In vitro and in vivo data suggest that trametinib is unlikely to affect the pharmacokinetics of other medicinal products. Based on in vitro studies, trametinib is not an inhibitor of CYP1A2, CYP2A6, CYP2B6, CYP2D6 and CYP3A4. Trametinib was found to be an in vitro inhibitor of CYP2C8, CYP2C9 and CYP2C19, an inducer of CYP3A4 and an inhibitor of the transporters OAT1, OAT3, OCT2, MATE1, OATP1B1, OATP1B3, P-gp and BCRP. However, based on the low dose and low clinical systemic exposure relative to the in vitro potency of inhibition or induction values, trametinib is not considered to be an in vivo inhibitor or inducer of these enzymes or transporters, although transient inhibition of BCRP substrates in the gut may occur (see section 4.5). Effects of other medicinal products on trametinib: In vivo and in vitro data suggest that the pharmacokinetics of trametinib are unlikely to be affected by other medicinal products. Trametinib is not a substrate of CYP enzymes or of the transporters BCRP, OATP1B1, OATP1B3, OATP2B1, OCT1, MRP2, and MATE1. Trametinib is an in vitro substrate of BSEP and the efflux transporter P- gp. Although trametinib exposure is unlikely to be affected by inhibition of BSEP, increased levels of trametinib upon strong inhibition of hepatic P-gp cannot be excluded (see section 4.5). Effects of trametinib on other medicinal products: the effect of repeat-dose trametinib on the steady state pharmacokinetics of combination oral contraceptives, norethindrone and ethinyl estradiol, was assessed in a clinical study that consisted of 19 female patients with solid tumours. Norethindrone exposure increased by 20% and ethinyl estradiol exposure was similar when co-administered with trametinib. Based on these results, no loss of efficacy of hormonal contraceptives is expected when co-administered with trametinib monotherapy.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. בשילוב עם Dabrafenib מלנומה מתקדמת (גרורתית או שאיננה נתיחה) בחולה המבטא מוטציה ב-BRAF. 2. בשילוב עם Dabrafenib כטיפול משלים (Adjuvant) במלנומה בשלב III לאחר הסרה מלאה של הגידול בחולה המבטא מוטציה ב-BRAF. משך הטיפול בתכשיר להתוויה זו לא יעלה על שנה.במהלך מחלתו יהיה החולה זכאי לטיפול בתרופה אחת בלבד מהתרופות המפורטות להלן – Binimetinib, Cobimetinib, Trametinibלעניין זה מלנומה בשלב מתקדם (לא נתיח או גרורתי) לא תוגדר כאותה מחלה כמו מלנומה בשלב בר הסרה בניתוח.3. בשילוב עם Dabrafenib כטיפול בסרטן תירואיד מסוג BRAF mutated ATC, מתקדם מקומי או גרורתי, בחולה שמיצה את אופציות הטיפול הקיימות.4. בשילוב עם Dabrafenib כטיפול בסרטן ריאה מתקדם מסוג BRAF V600 mutated NSCLC. 5. בשילוב עם Dabrafenib כטיפול בגליומה בדרגה נמוכה (low grade glioma) לא נתיחה או גרורתית עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. 6. בשילוב עם Dabrafenib כטיפול בגליומה בדרגה גבוהה (high grade glioma) לא נתיחה או גרורתית עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. 7. בשילוב עם Dabrafenib כטיפול באמלובלסטומה עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. 8. בשילוב עם Dabrafenib כטיפול בסרטן של דרכי המרה (Biliary tract cancer) לא נתיח או גרורתי עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. 9. בשילוב עם Dabrafenib כטיפול בסרטן תירואיד פפילרי (Papillary thyroid cancer) לא נתיח או גרורתי עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. 10. בשילוב עםDabrafenib כטיפול באדנוקרצינומה של המעי הדק (Adenocarcinoma of the small intestine) לא נתיחה או גרורתית עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. 11. בשילוב עם Dabrafenib כטיפול בסרטן שחלה בדרגה נמוכה (Low grade ovarian cancer) לא נתיח או גרורתי עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה או מומחה באנדוקרינולוגיה או ברפואת אף אוזן גרון.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| בשילוב עם Dabrafenib כטיפול בסרטן ריאה מתקדם מסוג BRAF V600 mutated NSCLC. | 30/01/2020 | אונקולוגיה | NSCLC | |
| בשילוב עם Dabrafenib כטיפול בסרטן תירואיד מסוג BRAF mutated ATC, מתקדם מקומי או גרורתי, בחולה שמיצה את אופציות הטיפול הקיימות. | 30/01/2020 | אונקולוגיה | ATC, Anaplastic thyroid cancer | |
| בשילוב עם Dabrafenib כטיפול משלים (Adjuvant) במלנומה בשלב III לאחר הסרה מלאה של הגידול בחולה המבטא מוטציה ב-BRAF. משך הטיפול בתכשיר להתוויה זו לא יעלה על שנה. | 16/01/2019 | אונקולוגיה | מלנומה בשלב III נתיח | |
| בשילוב עם Dabrafenib מלנומה מתקדמת (גרורתית או שאיננה נתיחה) בחולה המבטא מוטציה ב-BRAF. | 12/01/2017 | אונקולוגיה | מלנומה מתקדמת (גרורתית או שאינה נתיחה) | |
| בשילוב עם Dabrafenib כטיפול בגליומה בדרגה נמוכה (low grade glioma) לא נתיחה או גרורתית עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. | 01/02/2023 | אונקולוגיה | Glioma (low grade) | |
| בשילוב עםDabrafenib כטיפול באדנוקרצינומה של המעי הדק (Adenocarcinoma of the small intestine) לא נתיחה או גרורתית עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. | 01/02/2023 | אונקולוגיה | אדנוקרצינומה של המעי הדק, Small intestine adenocarcinoma | |
| בשילוב עם Dabrafenib כטיפול באמלובלסטומה עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. | 01/02/2023 | אונקולוגיה | אמלובלסטומה, Ameloblastoma | |
| בשילוב עם Dabrafenib כטיפול בסרטן תירואיד פפילרי (Papillary thyroid cancer) לא נתיח או גרורתי עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. | 01/02/2023 | אונקולוגיה | סרטן תירואיד פפילרי, PTC, Papillary thyroid cancer | |
| בשילוב עם Dabrafenib כטיפול בסרטן של דרכי המרה (Biliary tract cancer) לא נתיח או גרורתי עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. | 01/02/2023 | אונקולוגיה | סרטן בדרכי המרה, Biliary tract cancer | |
| בשילוב עם Dabrafenib כטיפול בגליומה בדרגה גבוהה (high grade glioma) לא נתיחה או גרורתית עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. | 01/02/2023 | אונקולוגיה | Glioma (high grade) |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
12/01/2017
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
14.08.22 - עלון לצרכן אנגלית 14.08.22 - עלון לצרכן עברית 14.08.22 - עלון לצרכן ערבית 07.06.23 - עלון לצרכן אנגלית 16.03.23 - עלון לצרכן עברית 07.06.23 - עלון לצרכן ערבית 17.04.24 - עלון לצרכן עברית 25.06.24 - עלון לצרכן עברית 02.07.24 - עלון לצרכן אנגלית 02.07.24 - עלון לצרכן ערבית 28.08.24 - עלון לצרכן אנגלית 28.08.24 - עלון לצרכן ערבית 10.10.24 - עלון לצרכן עברית 10.04.16 - החמרה לעלון 21.12.16 - החמרה לעלון 01.06.17 - החמרה לעלון 09.01.18 - החמרה לעלון 07.03.19 - החמרה לעלון 04.12.19 - החמרה לעלון 18.04.21 - החמרה לעלון 27.04.22 - החמרה לעלון 16.03.23 - החמרה לעלון 17.04.24 - החמרה לעלון 25.06.24 - החמרה לעלון 10.10.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
מקיניסט 0.5 מ"ג