Quest for the right Drug
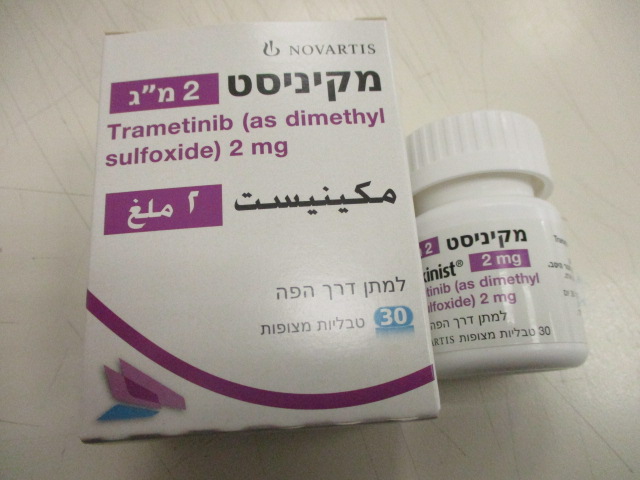
מקיניסט 2 מ"ג MEKINIST 2 MG (TRAMETINIB AS DIMETHYL SULFOXIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Summary of the safety profile The safety of trametinib monotherapy has been evaluated in the integrated safety population of 329 patients with BRAF V600 mutant unresectable or metastatic melanoma treated with trametinib 2 mg once daily in studies MEK114267, MEK113583, and MEK111054. Of these patients, 211 were treated with trametinib for BRAF V600 mutant melanoma in the randomised open label Phase III study MEK114267 (METRIC) (see section 5.1). The most common adverse reactions (incidence ≥20%) for trametinib were rash, diarrhoea, fatigue, oedema peripheral, nausea, and dermatitis acneiform. The safety of trametinib in combination with dabrafenib has been evaluated in the integrated safety population of 1,076 patients with BRAF V600 mutant unresectable or metastatic melanoma Stage III BRAF V600 mutant melanoma following complete resection (adjuvant treatment) and advanced NSCLC treated with trametinib 2 mg once daily and dabrafenib 150 mg twice daily. Of these patients, 559 were treated with the combination for BRAF V600 mutant melanoma in two randomised Phase III studies, MEK115306 (COMBI-d) and MEK116513 (COMBI-v), 435 were treated with the combination in the adjuvant treatment of Stage III BRAF V600 mutant melanoma after complete resection in a randomised Phase III study BRF115532 (COMBI-AD) and 82 were treated with the combination for BRAF V600 mutant NSCLC in a multi-cohort, non-randomised Phase II study BRF113928 (see section 5.1). The most common adverse reactions (incidence ≥ 20 %) for trametinib in combination with dabrafenib were: pyrexia, fatigue, nausea, chills, headache, diarrhoea, vomiting, arthralgia and rash. The safety of trametinib when administered with dabrafenib was also evaluated in a multi-cohort, multi- center, non-randomized, open-label study in adult patients with cancers with the BRAF V600E mutation (Study BRF117019). A total of 206 patients were enrolled in the trial, 36 of whom were enrolled in the ATC cohort, 105 were enrolled in specific solid tumor cohorts, and 65 in other malignancies (see section 5.1) Patients received trametinib 2 mg orally once daily and dabrafenib 150 mg orally twice daily until disease progression or unacceptable toxicity. Among these 206 patients, 101 (49%) were exposed to trametinib for ≥ 1 year and 103 (50%) were exposed to dabrafenib for ≥ 1 year. The median age was 60 years (range: 18 to 89); 56% were male; 79% were White; and 34% had baseline ECOG performance status of 0 and 60% had ECOG performance status of 1. The adverse reaction profile among all patients in study BRF117019 was similar to that observed in other approved indications. \ Tabulated list of adverse reactions Adverse reactions associated with trametinib obtained from clinical studies and post marketing surveillance are tabulated below for trametinib monotherapy (Table 6) and trametinib in combination with dabrafenib (Table 7). Adverse reactions are listed below by MedDRA system organ class. The following convention has been utilised for the classification of frequency: Very common ≥1/10 Common ≥1/100 to <1/10 Uncommon ≥1/1,000 to <1/100 Rare ≥1/10,000 to <1/1,000 Very rare <1/10,000 Not known (cannot be estimated from the available data) Categories have been assigned based on absolute frequencies in the clinical trial data. Within each frequency grouping, adverse reactions are presented in order of decreasing seriousness. Table 6. Adverse reactions with trametinib monotherapy System Organ Class Frequency (all Adverse Reactions grades) Folliculitis Paronychia Infections and infestations Common Cellulitis Rash pustular Blood and lymphatic system Common Anaemia disorders Immune system disorders Common Hypersensitivitya Metabolism and nutrition Common Dehydration disorders Peripheral neuropathy (including sensory Nervous system disorders Common and motor neuropathy) Vision blurred Common Periorbital oedema Visual impairment Eye disorders Chorioretinopathy Papilloedema Uncommon Retinal detachment Retinal vein occlusion Left ventricular dysfunction Common Ejection fraction decreased Cardiac disorders Bradycardia Uncommon Cardiac failure Not known Atrioventricular blockb Hypertension Very common Vascular disorders Haemorrhagec Common Lymphoedema Cough Very common Respiratory, thoracic and Dyspnoea mediastinal disorders Common Pneumonitis Uncommon Interstitial lung disease Diarrhoea Nausea Vomiting Very common Constipation Gastrointestinal disorders Abdominal pain Dry mouth Common Stomatitis Uncommon Gastrointestinal perforation Colitis Rash Dermatitis acneiform Very common Dry skin Pruritus Skin and subcutaneous tissue Alopecia disorders Erythema Palmar-plantar erythrodysaesthesia Common syndrome Skin fissures Skin chapped Musculoskeletal and Uncommon Rhabdomyolysis connective tissue disorders Fatigue Very common Oedema peripheral General disorders and Pyrexia administration site Face oedema conditions Common Mucosal inflammation Asthenia Very common Aspartate aminotransferase increased Alanine aminotransferase increased Investigations Common Blood alkaline phosphatase increased Blood creatine phosphokinase increased a May present with symptoms such as fever, rash, increased liver transaminases, and visual disturbances. b Including atrioventricular block complete. c Events include but are not limited to: epistaxis, haematochezia, gingival bleeding, haematuria, and rectal, haemorrhoidal, gastric, vaginal, conjunctival, intracranial and post procedural haemorrhage. Table 7. Adverse reactions with trametinib in combination with dabrafenib System Organ Class Frequency (all Adverse Reactions grades) Very common Nasopharyngitis Urinary tract infection Infections and infestations Cellulitis Common Folliculitis Paronychia Rash pustular Cutaneous squamous cell carcinomaa Neoplasms benign, Common Papillomab malignant and unspecified Seborrhoeic keratosis (incl cysts and polyps) New primary melanomac Uncommon Acrochordon (skin tags) Neutropenia Blood and lymphatic system Anaemia disorders Common Thrombocytopenia Leukopenia Hypersensitivityd Uncommon Immune system disorders Sarcoidosis Rare Haemophagocytic lymphohistiocytosis Very common Decreased appetite Dehydration Metabolism and nutrition Hyponatraemia Common disorders Hypophosphataemia Hyperglycaemia Not known Tumour lysis syndrome Headache Very common Dizziness Nervous system disorders Peripheral neuropathy (including sensory Common and motor neuropathy) Vision blurred Common Visual impairment Uveitis Eye disorders Chorioretinopathy Uncommon Retinal detachment Periorbital oedema Common Ejection fraction decreased Cardiac disorders Atrioventricular blocke Uncommon Bradycardia Not known Myocarditis Hypertension Very common Haemorrhagef Vascular disorders Hypotension Common Lymphoedema Very common Cough Respiratory, thoracic and Common Dyspnoea mediastinal disorders Uncommon Pneumonitis Abdominal paing Constipation Very common Diarrhoea Nausea Vomiting Gastrointestinal disorders Dry mouth Common Stomatitis Pancreatitis Uncommon Colitis Rare Gastrointestinal perforation Dry skin Pruritus Very common Rash Erythemah Dermatitis acneiform Actinic keratosis Night sweats Hyperkeratosis Alopecia Palmar-plantar erythrodysaesthesia Skin and subcutaneous tissue Common syndrome disorders Skin lesion Hyperhidrosis Panniculitis Skin fissures Photosensitivity Uncommon Acute febrile neutrophilic dermatosis Stevens-Johnson syndrome Drug reaction with eosinophilia and Not Known systemic symptoms Dermatitis exfoliative generalised Arthralgia Musculoskeletal and Myalgia Very common connective tissue disorders Pain in extremity Muscle spasmsi Renal failure Renal and urinary disorders Uncommon Nephritis Fatigue Chills Asthenia General disorders and Very common Oedema peripheral administration site Pyrexia conditions Influenza-like illness Mucosal inflammation Common Face oedema Alanine aminotransferase increased Very common Aspartate aminotransferase increased Investigations Blood alkaline phosphatase increased Common Gamma-glutamyltransferase increased Blood creatine phosphokinase increased The safety profile from MEK116513 is generally similar to that of MEK115306 with the following exceptions: 1) The following adverse reactions have a higher frequency category as compared to MEK115306: muscle spasm (very common); renal failure and lymphoedema (common); acute renal failure (uncommon); 2) The following adverse reactions have occurred in MEK116513 but not in MEK115306: cardiac failure, left ventricular dysfunction, interstitial lung disease (uncommon); 3) The following adverse reaction has occurred in MEK116513 and BRF115532 but not in MEK115306 and BRF113928: rhabdomyolysis (uncommon). a Cutaneous squamous cell carcinoma (cuSCC): SCC, SCC of the skin, SCC in situ (Bowen’s disease) and keratoacanthoma b Papilloma, skin papilloma c Malignant melanoma, metastatic malignant melanoma, and superficial spreading melanoma Stage III d Includes drug hypersensitivity e Including atrioventricular block complete f Bleeding from various sites, including intracranial bleeding and fatal bleeding g Abdominal pain upper and abdominal pain lower h Erythema, generalised erythema i Muscle spasms, musculoskeletal stiffness Description of selected adverse reactions New malignancies New malignancies, cutaneous and non-cutaneous, can occur when trametinib is used in combination with dabrafenib. Please refer to the dabrafenib Prescribing Information. Haemorrhage Haemorrhagic events, including major haemorrhagic events and fatal haemorrhages, occurred in patients taking trametinib as monotherapy and in combination with dabrafenib. The majority of bleeding events were mild. Fatal intracranial haemorrhages occurred in the integrated safety population of trametinib in combination with dabrafenib in <1% (8/1076) of patients. The median time to onset of the first occurrence of haemorrhagic events for the combination of trametinib and dabrafenib was 94 days in the melanoma Phase III studies and 75 days in the NSCLC study for the patients who had received prior anti-cancer therapy. The risk of haemorrhage may be increased with concomitant use of antiplatelet or anticoagulant therapy. If haemorrhage occurs, treat as clinically indicated (see section 4.4). LVEF reduction/Left ventricular dysfunction Trametinib has been reported to decrease LVEF when used as monotherapy or in combination with dabrafenib. In clinical trials, the median time to first occurrence of left ventricular dysfunction, cardiac failure and LVEF decrease was between 2 to 5 months. In the integrated safety population of trametinib in combination with dabrafenib, decreased LVEF has been reported in 6% (65/1076) of patients, with most cases being asymptomatic and reversible. Patients with LVEF lower than the institutional lower limit of normal were not included in clinical trials with trametinib. Trametinib should be used with caution in patients with conditions that could impair left ventricular function (see sections 4.2 and 4.4). Pyrexia Pyrexia has been reported in clinical trials with trametinib as monotherapy and in combination with dabrafenib; however, the incidence and severity of pyrexia are increased with the combination therapy. Please refer to sections 4.4 and 4.8 of the dabrafenib Prescribing Information. Hepatic events Hepatic adverse reactions have been reported in clinical trials with trametinib as monotherapy and in combination with dabrafenib. Of the hepatic adverse reactions, increased ALT and AST were the most common events and the majority were either Grade 1 or 2. For trametinib monotherapy, more than 90% of these liver events occurred within the first 6 months of treatment. Liver events were detected in clinical trials with monitoring every four weeks. It is recommended that patients receiving treatment with trametinib monotherapy or in combination with dabrafenib have liver function monitored every four weeks for 6 months. Liver monitoring may be continued thereafter as clinically indicated (see section 4.4). Hypertension Elevations in blood pressure have been reported in association with trametinib as monotherapy and in combination with dabrafenib, in patients with or without pre-existing hypertension. Blood pressure should be measured at baseline and monitored during treatment, with control of hypertension by standard therapy as appropriate (see section 4.4). Interstitial lung disease (ILD)/Pneumonitis Patients treated with trametinib or combination with dabrafenib may develop ILD or pneumonitis. Trametinib should be withheld in patients with suspected ILD or pneumonitis, including patients presenting with new or progressive pulmonary symptoms and findings including cough, dyspnoea, hypoxia, pleural effusion, or infiltrates, pending clinical investigations. For patients diagnosed with treatment-related ILD or pneumonitis trametinib should be permanently discontinued (see sections 4.2 and 4.4). Visual impairment Disorders associated with visual disturbances, including RPED and RVO, have been observed with trametinib. Symptoms such as blurred vision, decreased acuity, and other visual disturbances have been reported in the clinical trials with trametinib (see sections 4.2 and 4.4). Rash Rash has been observed in about 60% of patients when given as monotherapy and in about 24% of patients in trametinib and dabrafenib combination studies in the integrated safety population. The majority of these cases were Grade 1 or 2 and did not require any dose interruptions or dose reductions (see sections 4.2 and 4.4). Rhabdomyolysis Rhabdomyolysis has been reported in patients taking trametinib alone or in combination with dabrafenib. Signs or symptoms of rhabdomyolysis should warrant an appropriate clinical evaluation and treatment as indicated (see section 4.4). Pancreatitis Pancreatitis has been reported with dabrafenib in combination with trametinib. Please see the dabrafenib Prescribing Information. Renal failure Renal failure has been reported with dabrafenib in combination with trametinib. Please see the dabrafenib Prescribing Information. Special populations Paediatric Pediatric Safety Pool The pediatric pooled safety population reflects exposure to weight-based trametinib orally, once daily administered in combination with dabrafenib in 166 pediatric patients across two trials: a multi-center, open-label, multi-cohort study in pediatric patients with BRAF V600E mutation-positive glioma requiring systemic therapy (Study G2201; n = 123) and a multi-center, open-label, multi-cohort study in pediatric patients with refractory or recurrent solid tumors with MAPK pathway activation (Study X2101; n = 43) (see section 5.1). Among 166 patients who received trametinib administered with dabrafenib, 85% were exposed for 6 months and 69% were exposed for greater than one year. The most common (> 20%) adverse reactions were pyrexia (66%), rash (54%), headache (40%), vomiting (38%), musculoskeletal pain (36%), fatigue (31%), dry skin (31%), diarrhea (30%), nausea (26%), epistaxis and other bleeding events (25%), abdominal pain (24%), and dermatitis acneiform (23%). The most common (> 2%) Grade 3 or 4 laboratory abnormalities were decreased neutrophil count (20%), increased alanine aminotransferase (3.1%), and increased aspartate aminotransferase (3.1%). BRAF V600E Mutation-Positive Solid Tumors in Pediatric Patients Study CTMT212X2101 (X2101) The safety of trametinib when administered with dabrafenib was evaluated in Study X2101, a multi- center, open-label, multi-cohort study in pediatric patients (n=48) with refractory or recurrent solid tumors activation (see section 5.1) The median duration of exposure to trametinib in Parts C (dose escalation) and D (cohort expansion) was 20.8 and 24.4 months, respectively. The median duration of exposure to dabrafenib in Parts C and D was 20.8 and 24.9 months, respectively. The median age of pediatric patients who received trametinib with dabrafenib was 9 years (range: 1 to 17). Serious adverse reactions occurred in 46% of patients who received trametinib in combination with dabrafenib. Serious adverse reactions in > 5% of patients included pyrexia (25%) and decreased ejection fraction (6%). Permanent treatment discontinuation due to an adverse reaction occurred in 21% of patients. Adverse reactions which resulted in permanent treatment discontinuation in > 3% of patients included increased ALT (6%), increased AST (4.2%) and decreased ejection fraction (4.2%). Dose interruptions due to an adverse reaction occurred in 73% of patients. Adverse reactions which required dose interruption in > 5% of patients included pyrexia (56%), vomiting (19%), neutropenia (13%), rash (13%), decreased ejection fraction (6%) and uveitis (6%). Dose reductions due to an adverse reaction occurred in 25% of patients. Adverse reactions which required dose reductions in > 5% of patients included pyrexia (13%). The most common (≥20%) adverse reactions, including laboratory abnormalities, are listed in Table 8 and Table 9. Table 8 summarizes the adverse reactions in Study X2101. Table 8. Adverse Reactions (>20%) in Pediatric Patients Treated with Trametinib Plus Dabrafenib in Study X2101 Trametinib plus Dabrafeniba (N=48) Adverse Reactions All Grades Grade 3 or 4 (%) (%) General Pyrexia 75 17 Fatigueb 48 0 Skin and subcutaneous tissue Rashc 73 2.1 Dry skin 48 0 Dermatitis acneiformd 40 0 Gastrointestinal Vomiting 52 4.2 Diarrhea 42 2.1 Abdominal paine 33 4.2 Nausea 33 2.1 Constipation 23 0 Respiratory system Cough 44 0 Nervous system Headache 35 0 Vascular Hemorrhagef 33 0 Infections and infestations Paronychia 23 0 a NCI CTCAE version 4.0. b Includes fatigue, asthenia and malaise. c Includes rash, rash maculo-papular, rash erythematous, rash papular, rash pustular, and rash macular. d Includes dermatitis acneiform and acne. e Includes abdominal pain and abdominal pain upper. f Includes epistaxis, hematuria, contusion, hematoma, petechiae, rectal hemorrhage, and red blood cell count decreased. Clinically relevant adverse reactions for trametinib in Study X2101 observed in less than 20% of patients (N=48) who received trametinib in combination with dabrafenib were: atrioventricular block (2.1%). Table 9 summarizes the laboratory abnormalities in Study X2101. Table 9. Select Laboratory Abnormalities (>20%) That Worsened from Baseline in Pediatric Patients Treated with Trametinib Plus Dabrafenib in Study X2101 Laboratory Abnormality Trametinib plus Dabrafeniba All Grades Grade 3 or 4 (%) (%) Chemistry Hyperglycemia 65 2.2 Hypoalbuminemia 48 2.1 Hypocalcemia 40 2.1 Decreased phosphate 38 0 Decreased magnesium 33 2.1 Hypernatremia 27 0 Hypokalemia 21 2.1 Hepatic Increased AST 55 4.2 Increased ALT 40 6 Increased alkaline phosphatase 28 6 Increased total bilirubin 21 2.1 Hematology Decreased hemoglobin 60 6 Decreased neutrophils 49 28 Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase. a The denominator used to calculate the rate varied from 39 to 48 based on the number of patients with a baseline value and at least one post-treatment value. BRAF V600E Mutation-Positive Low-Grade Glioma in Pediatric Patients Study CDRB436G2201 (G2201) The safety of trametinib in combination with dabrafenib was evaluated in pediatric patients 1 to < 18 years of age in Study G2201. Patients with low-grade glioma (LGG) who required first systemic therapy were randomized (2:1) to trametinib plus dabrafenib (n = 73) or carboplatin plus vincristine (n = 33). Nine patients crossed over from the carboplatin plus vincristine arm to the trametinib and dabrafenib arm. Pediatric patients received weight-based trametinib orally once daily administered in combination with dabrafenib until disease progression or intolerable toxicity. Patients in the control arm received carboplatin and vincristine at doses of 175 mg/m2 and 1.5 mg/m2, respectively in 10- week induction course followed by eight 6-week cycles of maintenance therapy or until disease progression or intolerable toxicity. Among patients with low-grade glioma who were randomized to trametinib plus dabrafenib (n = 73), 95% were exposed for 6 months or longer and 71% were exposed for greater than one year. The median age of these patients was 10 years (range: 1 to 17); 60% female; 75% White, 7% Asian, 2.7% Black or African American, 4% other race and 11% where race was unknown or not reported. Serious adverse reactions occurred in 40% of these patients. Serious adverse reactions in > 3% of patients included pyrexia (14%) and vomiting (4%). Permanent discontinuation of trametinib due to an adverse reaction occurred in 4% of patients. Adverse reactions which resulted in permanent discontinuation of trametinib included chills, fatigue, pyrexia, weight increased, and headache. Dosage interruptions of trametinib due to an adverse reaction occurred in 70% of patients. Adverse reactions which required a dosage interruption in > 5% of patients included pyrexia (52%). Dose reductions of trametinib due to an adverse reaction occurred in 12% of patients. Adverse reactions which required dose reductions in > 2% of patients included weight increased (2.7%). The most common (≥ 15%) adverse reactions were pyrexia (68%), rash (51%), headache (47%), vomiting (34%), musculoskeletal pain (34%), fatigue (33%), diarrhea (29%), dry skin (26%), nausea (25%), hemorrhage (25%), abdominal pain (25%), dermatitis acneiform (22%), dizziness (15%), upper respiratory tract infection (15%), and weight increased (15%). The most common (≥ 20%) laboratory abnormalities that worsened from baseline were leukopenia (59%), increased alkaline phosphatase (55%), anemia (46%), decreased neutrophils (44%), increased AST (37%), decreased magnesium (34%), increased magnesium (32%), decreased platelets (30%), increased ALT (29%), and increased lymphocytes (24%). Table 10 summarizes the adverse reactions in Study G2201. Table 10. Adverse Reactions (≥ 15%) in Pediatric LGG Patients Who Received Trametinib in Combination with Dabrafenib in Study G2201a Trametinib plus Dabrafenib Carboplatin plus Vincristine Adverse Reactions N = 73 N = 33 All Grades Grade ≥ 3 All Grades Grade ≥ 3 (%) (%) (%) (%) Gastrointestinal Vomiting 34 1 48 3 Diarrheab 29 0 18 6 Nausea 25 0 45 0 c Abdominal pain 25 0 24 0 Constipation 12 0 36 0 Stomatitisd 10 0 18 0 General Pyrexiae 68 8 18 3 Fatiguef 33 0 39 0 Nervous system Headacheg 47 1 33 3 Dizzinessh 15 0 9 3 Peripheral neuropathyi 7 0 45 6 Vascular Hemorrhagej 25 0 12 0 Skin and subcutaneous tissue Rashk 51 2.7 18 3 Dry skin 26 0 3 0 Dermatitis acneiforml 22 0 0 0 Alopecia 3 0 24 0 Musculoskeletal and connective tissue Musculoskeletal painm 34 0 30 0 Pain in jaw 1.4 0 18 0 Metabolism and nutrition Decreased appetite 5 0 24 0 Respiratory, thoracic and mediastinal Oropharyngeal pain 11 0 18 0 Psychiatric Anxiety 1.4 0 15 3 Immune system Hypersensitivity 0 0 15 3 Infections and infestations Upper respiratory tract infection 15 0 6 0 Injury, poisoning and procedural complications Infusion related reaction 0 0 15 3 Investigations Weight increased 15 7 0 0 aNCI CTCAE version 4.03. bIncludes diarrhea, colitis, enterocolitis, and enteritis. cIncludes abdominal pain and upper abdominal pain. dIncludes stomatitis, cheilitis, mouth ulceration, aphthous ulcer, and glossitis. eIncludes pyrexia and body temperature increased. fIncludes fatigue and asthenia. gIncludes headache and migraine with aura. hIncludes dizziness and vertigo. iIncludes peripheral neuropathy, peripheral motor neuropathy, peripheral sensorimotor neuropathy, paresthesia, neuralgia, hypoaesthesia, and peripheral sensory neuropathy. jIncludes epistaxis, post-procedural hemorrhage, hematuria, upper gastrointestinal hemorrhage, and hemorrhage intracranial. kIncludes rash, rash macular, rash maculo-papular, rash pustular, rash papular, rash erythematous, eczema, erythema multiforme, dermatitis, dermatitis exfoliative, skin exfoliation, palmar-plantar erythrodysaesthesia syndrome, and dermatitis bullous. lIncludes dermatitis acneiform, acne, and acne pustular. mIncludes back pain, myalgia, pain in extremity, arthralgia, bone pain, non-cardiac chest pain, neck pain, and musculoskeletal stiffness. Table 11 summarizes the laboratory abnormalities in Study G2201. Table 11. Select Laboratory Abnormalities (≥ 20%) That Worsened from Baseline in Pediatric LGG Patients Who Received Trametinib in Combination with Dabrafenib in Study G2201a Trametinib plus Dabrafenib Carboplatin plus Vincristine N = 73 N = 33 Laboratory Abnormality All Grades Grade 3 or 4 All Grades Grade 3 or 4 (%) (%) (%) (%) Hepatic Increased alkaline phosphatase 55 0 13 0 Increased AST 37 1.4 55 0 Increased ALT 29 3 61 9 Chemistry Decreased magnesium 34 4.1 76 6 Increased magnesium 32 0 24 3 Increased potassium 15 4.2 21 6 Decreased calcium 14 4.1 22 9 Decreased potassium 8 1.4 70 0 Decreased phosphate 7 2.7 33 3 Decreased sodium 5 1.4 27 6 Increased serum fasting glucose 0 0 44 0 Hematology Decreased leukocytes 59 0 91 18 Decreased hemoglobin 46 0 94 36 Decreased neutrophils 44 17 84 75 Decreased platelets 30 0 73 18 Increased lymphocytes 24 0 13 3.1 Decreased lymphocytes 16 1.4 56 6 Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase. a The denominator used to calculate the rate varied from 70 to 73 in D+T arm and 9 to 33 in C + V arm based on the number of patients with a baseline value and at least one post-treatment value. Elderly In the Phase III study with trametinib in patients with unresectable or metastatic melanoma (n = 211), 49 patients (23%) were ≥65 years of age, and 9 patients (4%) were ≥75 years of age. The proportion of subjects experiencing adverse reactions (AR) and serious adverse reactions (SAR) was similar in the subjects aged <65 years and those aged ≥65 years. Patients ≥65 years were more likely to experience ARs leading to permanent discontinuation of medicinal product, dose reduction and dose interruption than those <65 years. In the integrated safety population of trametinib in combination with dabrafenib (n=1,076) 265 patients (25%) were ≥65 years of age; 62 patients (6%) were ≥75 years of age. The proportion of patients experiencing ARs was similar in those aged <65 years and those aged ≥65 years in all studies. Patients ≥65 years were more likely to experience SARs and ARs leading to permanent discontinuation of medicinal product, dose reduction and dose interruption than those <65 years. Of the 26 patients with ATC who received trametinib in Study BRF117019, 77% were aged 65 years and older and 31% were aged 75 years and older (see section 5.1). This study did not include sufficient numbers of younger adults to determine whether they respond differently compared to geriatric patients. Renal impairment No dosage adjustment is required in patients with mild or moderate renal impairment (see section 5.2). Trametinib should be used with caution in patients with severe renal impairment (see sections 4.2 and 4.4). Hepatic impairment No dosage adjustment is required in patients with mild hepatic impairment (see section 5.2). Trametinib should be used with caution in patients with moderate or severe hepatic impairment (see sections 4.2 and 4.4) Trametinib in combination with dabrafenib in patients with brain metastases The safety and efficacy of the combination of trametinib and dabrafenib have been evaluated in a multi-cohort, open-label, Phase II study in patients with BRAF V600 mutant melanoma with brain metastases. The safety profile observed in these patients appears to be consistent with the integrated safety profile of the combination. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il And to Novartis using the following email address: safetydesk.israel@novartis.com

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. בשילוב עם Dabrafenib מלנומה מתקדמת (גרורתית או שאיננה נתיחה) בחולה המבטא מוטציה ב-BRAF. 2. בשילוב עם Dabrafenib כטיפול משלים (Adjuvant) במלנומה בשלב III לאחר הסרה מלאה של הגידול בחולה המבטא מוטציה ב-BRAF. משך הטיפול בתכשיר להתוויה זו לא יעלה על שנה.במהלך מחלתו יהיה החולה זכאי לטיפול בתרופה אחת בלבד מהתרופות המפורטות להלן – Binimetinib, Cobimetinib, Trametinibלעניין זה מלנומה בשלב מתקדם (לא נתיח או גרורתי) לא תוגדר כאותה מחלה כמו מלנומה בשלב בר הסרה בניתוח.3. בשילוב עם Dabrafenib כטיפול בסרטן תירואיד מסוג BRAF mutated ATC, מתקדם מקומי או גרורתי, בחולה שמיצה את אופציות הטיפול הקיימות.4. בשילוב עם Dabrafenib כטיפול בסרטן ריאה מתקדם מסוג BRAF V600 mutated NSCLC. 5. בשילוב עם Dabrafenib כטיפול בגליומה בדרגה נמוכה (low grade glioma) לא נתיחה או גרורתית עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. 6. בשילוב עם Dabrafenib כטיפול בגליומה בדרגה גבוהה (high grade glioma) לא נתיחה או גרורתית עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. 7. בשילוב עם Dabrafenib כטיפול באמלובלסטומה עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. 8. בשילוב עם Dabrafenib כטיפול בסרטן של דרכי המרה (Biliary tract cancer) לא נתיח או גרורתי עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. 9. בשילוב עם Dabrafenib כטיפול בסרטן תירואיד פפילרי (Papillary thyroid cancer) לא נתיח או גרורתי עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. 10. בשילוב עםDabrafenib כטיפול באדנוקרצינומה של המעי הדק (Adenocarcinoma of the small intestine) לא נתיחה או גרורתית עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. 11. בשילוב עם Dabrafenib כטיפול בסרטן שחלה בדרגה נמוכה (Low grade ovarian cancer) לא נתיח או גרורתי עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה או מומחה באנדוקרינולוגיה או ברפואת אף אוזן גרון.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| בשילוב עם Dabrafenib כטיפול בגליומה בדרגה נמוכה (low grade glioma) לא נתיחה או גרורתית עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. | 01/02/2023 | אונקולוגיה | Glioma (low grade) | |
| בשילוב עם Dabrafenib כטיפול משלים (Adjuvant) במלנומה בשלב III לאחר הסרה מלאה של הגידול בחולה המבטא מוטציה ב-BRAF. משך הטיפול בתכשיר להתוויה זו לא יעלה על שנה. | 16/01/2019 | אונקולוגיה | מלנומה בשלב III נתיח | |
| בשילוב עםDabrafenib כטיפול באדנוקרצינומה של המעי הדק (Adenocarcinoma of the small intestine) לא נתיחה או גרורתית עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. | 01/02/2023 | אונקולוגיה | אדנוקרצינומה של המעי הדק, Small intestine adenocarcinoma | |
| בשילוב עם Dabrafenib כטיפול באמלובלסטומה עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. | 01/02/2023 | אונקולוגיה | אמלובלסטומה, Ameloblastoma | |
| בשילוב עם Dabrafenib כטיפול בסרטן תירואיד פפילרי (Papillary thyroid cancer) לא נתיח או גרורתי עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. | 01/02/2023 | אונקולוגיה | סרטן תירואיד פפילרי, PTC, Papillary thyroid cancer | |
| בשילוב עם Dabrafenib כטיפול בסרטן ריאה מתקדם מסוג BRAF V600 mutated NSCLC. | 30/01/2020 | אונקולוגיה | NSCLC | |
| בשילוב עם Dabrafenib מלנומה מתקדמת (גרורתית או שאיננה נתיחה) בחולה המבטא מוטציה ב-BRAF. | 12/01/2017 | אונקולוגיה | מלנומה מתקדמת (גרורתית או שאינה נתיחה) | |
| בשילוב עם Dabrafenib כטיפול בסרטן של דרכי המרה (Biliary tract cancer) לא נתיח או גרורתי עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. | 01/02/2023 | אונקולוגיה | סרטן בדרכי המרה, Biliary tract cancer | |
| בשילוב עם Dabrafenib כטיפול בסרטן תירואיד מסוג BRAF mutated ATC, מתקדם מקומי או גרורתי, בחולה שמיצה את אופציות הטיפול הקיימות. | 30/01/2020 | אונקולוגיה | ATC, Anaplastic thyroid cancer | |
| בשילוב עם Dabrafenib כטיפול בגליומה בדרגה גבוהה (high grade glioma) לא נתיחה או גרורתית עם מוטציה מסוג BRAF V600E, לאחר התקדמות מחלה בטיפול קודם או כאשר לא קיימות אופציות טיפוליות חלופיות. | 01/02/2023 | אונקולוגיה | Glioma (high grade) |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
12/01/2017
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
07.06.23 - עלון לצרכן אנגלית 16.03.23 - עלון לצרכן עברית 07.06.23 - עלון לצרכן ערבית 17.04.24 - עלון לצרכן עברית 25.06.24 - עלון לצרכן עברית 02.07.24 - עלון לצרכן אנגלית 02.07.24 - עלון לצרכן ערבית 28.08.24 - עלון לצרכן אנגלית 28.08.24 - עלון לצרכן ערבית 10.10.24 - עלון לצרכן עברית 10.04.16 - החמרה לעלון 21.12.16 - החמרה לעלון 01.06.17 - החמרה לעלון 09.01.18 - החמרה לעלון 07.03.19 - החמרה לעלון 04.12.19 - החמרה לעלון 18.04.21 - החמרה לעלון 27.04.22 - החמרה לעלון 16.03.23 - החמרה לעלון 17.04.24 - החמרה לעלון 25.06.24 - החמרה לעלון 10.10.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
מקיניסט 2 מ"ג