Quest for the right Drug
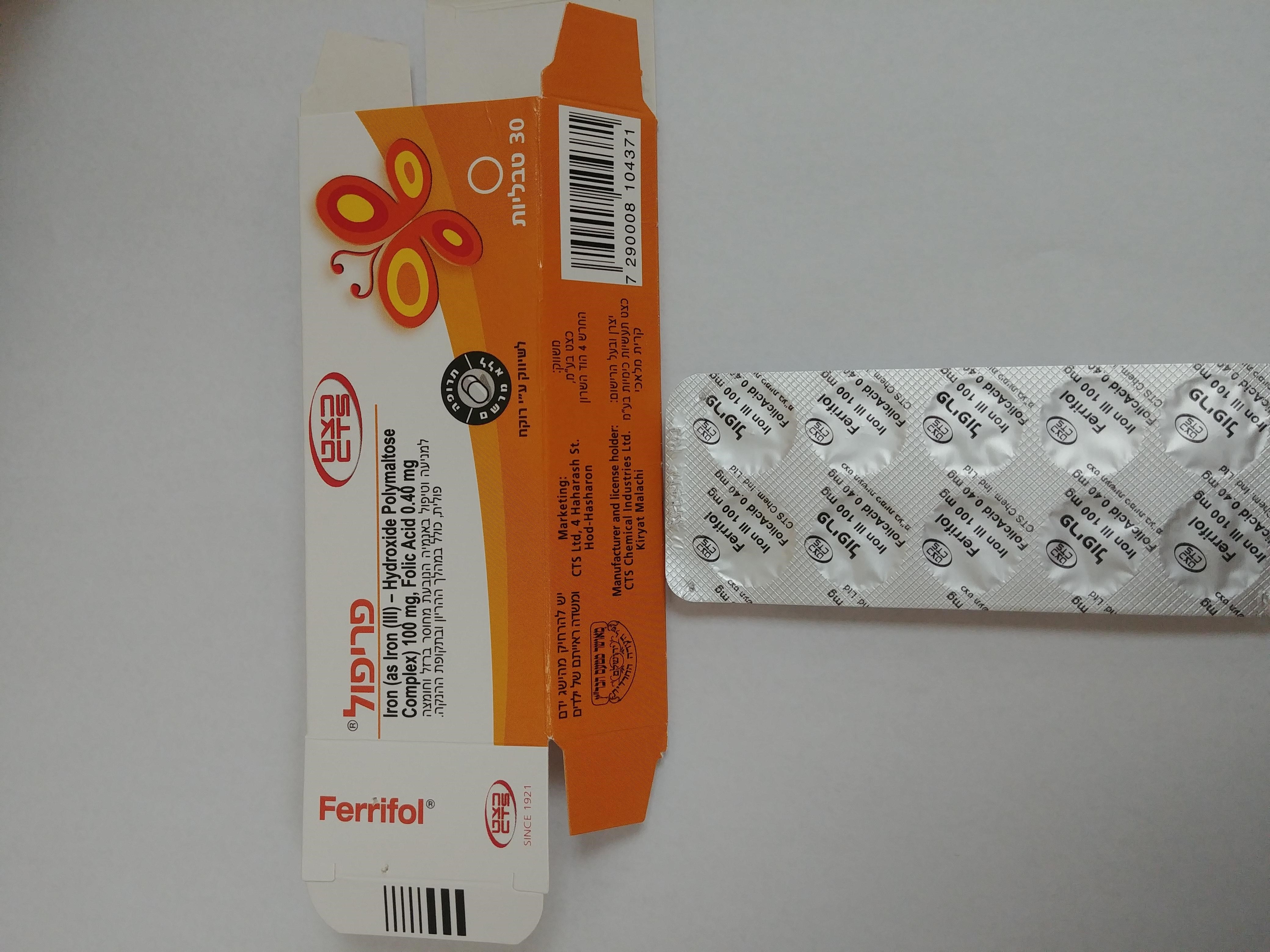
פריפול FERRIFOL (FERROUS AS IRON III HYDROXIDE POLYMALTOSE COMPL., FOLIC ACID)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
Mechanism of action In IPC, the polynuclear iron (III) hydroxide core is surrounded at its surface by a number of non-covalently bound polymaltose molecules resulting in an overall average molecular weight of approximately 50 kDa. The polynuclear core of IPC has a structure similar to that of the physiological iron storage protein ferritin. IPC is a stable complex and does not release large amounts of iron under physiological conditions. Because of its size, the extent of diffusion of IPC through the membrane of the mucosa is about 40 times less than that of most water-soluble iron (II) salts, existing in aqueous solution as Hexaquo-iron(II) ion complex. Iron from the complex IPC is taken up in the gut via an active mechanism. Folic acid (folate) is a member of the Vitamin B group. It is a tetrahydrofolate precursor, a coenzyme involved in various metabolic processes including the biosynthesis of nucleic acid purines and thymidylates. Folic acid is required for nucleoprotein synthesis and maintenance of normal erythropoiesis. Pharmacodynamics The absorbed iron is bound to transferrin and is used for Hb synthesis in the bone marrow or is stored, mainly in the liver, where it is bound to ferritin. Clinical efficacy During pregnancy, there is an increased requirement for iron which is approximately 0.8 mg/day in the first trimester and up to 6 mg/day during the third trimester of pregnancy. In addition, there is an increased requirement for folic acid, particularly during pregnancy. Low folic acid levels can lead to signs of deficiency in both mothers (anaemia, peripheral neuropathies) and the foetus (congenital neural tube defects). Clinical studies have been carried out in pregnant women to investigate the safety and efficacy of the treatment of iron deficiency with or without anaemia, as well as to prevent an iron and folic acid deficiency with IPC treatment in combination with folic acid (Ferrifol). Changes in haematological parameters were compared during treatment with Ferrifol tablets at a dose of 100 mg–300 mg iron/day in conjunction with 0.35 mg folic acid/day in comparison to iron (II) sulphate standard preparations with and without folic acid. A study investigated the efficacy of IPC with the addition of a folic acid supplement compared to intravenous iron administration, and another study examined the efficacy and tolerability of Ferrifol compared to a diet high in iron. In total, approximately 700 pregnant women with normal and decreased iron were included, and more than 400 of these patients received Ferrifol. Treatment of pregnant women with Ferrifol showed similar improvements in haematological parameters compared to results with Ferrifol in non-pregnant patients with at the same time a good tolerability. An improvement in the haemoglobin values to an average of 0.72 to 2.2 g/dL (p<0.05) as compared to the start of treatment was observed in the clinical studies following treatment with Ferrifol lasting between 30 days and 2.5 months. In addition, improvements were measured in serum ferritin (+5.74 mcg/L) and in red blood cell ferritin levels (on average +6.3 mcg/g or 5.74 mcg/g after treatment lasting 30 days or 2.5 months compared to the baseline). An open study investigated the efficacy of Ferrifol (200 mg IPC/day for 10 days and 100 mg/day for 20 days) with supplemental vitamin B12 in pregnant women with iron deficiency anaemia. There was a significant increase in haemoglobin values as well as in the haematocrit, the number of erythrocytes and folic acid values. (p<0.01). An open study with 43 adolescents with varying degrees of iron deficiency anaemia between 14.5 and 17 years of age investigated the efficacy of Maltofer Fol on haemoglobin levels. In the group with mild anaemia (n=19), the anaemia was corrected after 48 to 49 days of treatment. Hb levels increased from 104.3 ± 1.7 g/L to 134.1 ± 1.3 g/L in this group. Correction of anaemia was achieved in patients with moderate anaemia (n=16; baseline Hb levels = 83.0 ± 0.4 g/L) after 75 to 76 days of treatment (Hb levels = 133.2 ± 1.1 g/L) and in patients with severe anaemia (n=8; baseline Hb levels = 67.9 ± 0.9 g/L) after 82 to 83 days of treatment (Hb levels = 134.4 ± 0.9 g/L).
Pharmacokinetic Properties

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
