Quest for the right Drug
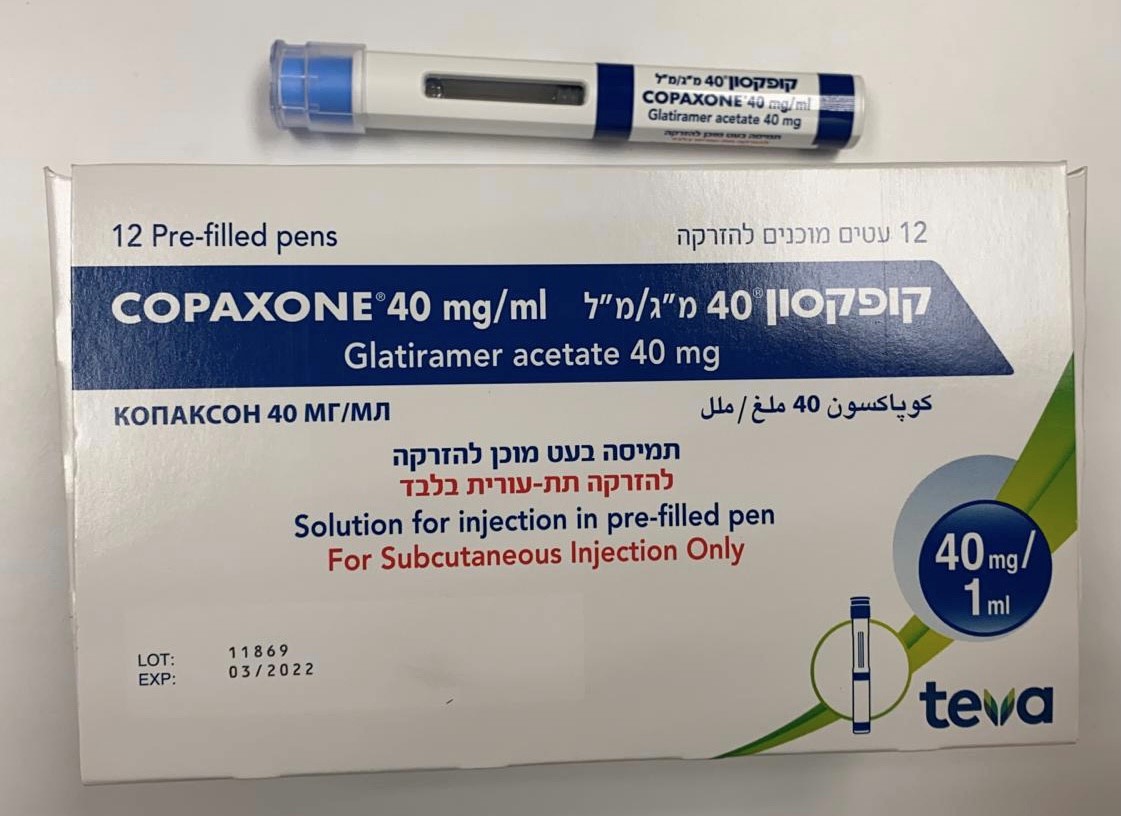
קופקסון ® 40 מ"ג/מ"ל COPAXONE ® 40 MG/ML (GLATIRAMER ACETATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תת-עורי : S.C
צורת מינון:
תמיסה להזרקה : SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Most Copaxone safety data were accumulated for Copaxone 20 mg/ml administered as a subcutaneous injection once daily. This section presents accumulated safety data from four placebo-controlled trials with Copaxone 20 mg/ml administered once daily, and from one placebo-controlled trial with Copaxone 40 mg/ml administered three times a week. A direct comparison of the safety between Copaxone 20 mg/ml (administered daily) and 40 mg/ml (administered three times per week) in the same study has not been performed. Copaxone 20 mg/ml (administered once daily) In all clinical trials with Copaxone 20 mg/ml, injection-site reactions were seen to be the most frequent adverse reactions and were reported by the majority of patients receiving Copaxone. In controlled studies, the proportion of patients reporting these reactions, at least once, was higher following treatment with Copaxone 20 mg/ml (70%) than placebo injections (37%). The most commonly reported injection-site reactions, which were more frequently reported in Copaxone 20 mg/ml vs. placebo- treated patients, were erythema, pain, mass, pruritus, oedema, inflammation and hypersensitivity. A reaction, associated with at least one or more of the following symptoms, has been described as the immediate post-injection reaction: vasodilatation (flushing), chest pain, dyspnoea, palpitation or tachycardia. This reaction may occur within minutes of a Copaxone injection. At least one component of this immediate post-injection reaction was reported at least once by 31% of patients receiving Copaxone 20 mg/ml compared to 13% of patients receiving placebo. All adverse reactions, which were more frequently reported in Copaxone 20 mg/ml vs. placebo-treated patients, are presented in the table below. This data was derived from four pivotal, double-blind, placebo-controlled clinical trials with a total of 512 patients treated with Copaxone 20 mg/day and 509 patients treated with placebo for up to 36 months. Three trials in relapsing-remitting MS (RRMS) included a total of 269 patients treated with Copaxone 20 mg/day and 271 patients treated with placebo for up to 35 months. The fourth trial in patients who have experienced a first clinical episode and were determined to be at high risk of developing clinically definite MS included 243 patients treated with Copaxone 20mg/day and 238 patients treated with placebo for up to 36 months. System Organ Class (SOC) Very Common Common Uncommon (≥1/10) (≥1/100 to <1/10) (≥1/1,000 to <1/100) Infections and infestations Infection, Influenza Bronchitis, Gastroenteritis, Abscess, Cellulitis, Furuncle, Herpes Simplex, Otitis Media, Herpes Zoster, Pyelonephritis Rhinitis, Tooth Abscess, Vaginal Candidiasis* Neoplasms benign, malignant Benign Neoplasm Of Skin, Skin Cancer and unspecified (incl cysts Neoplasm and polyps) Blood and lymphatic system Lymphadenopathy* Leukocytosis, Leukopenia, disorders Splenomegaly Thrombocytopenia, Lymphocyte Morphology Abnormal Immune system disorders Hypersensitivity Endocrine disorders Goitre, Hyperthyroidism Metabolism and nutrition Anorexia, Weight Increased* Alcohol Intolerance, Gout, disorders Hyperlipidaemia, Blood Sodium Increased, Serum Ferritin Decreased Psychiatric disorders Anxiety*, Nervousness Abnormal Dreams, Confusional Depression State, Euphoric Mood, Hallucination, Hostility, Mania, Personality Disorder, Suicide Attempt Nervous system disorders Headache, Dysgeusia, Hypertonia, Carpal Tunnel Syndrome, Migraine, Speech Disorder, Cognitive Disorder, Convulsion, Syncope, Tremor* Dysgraphia, Dyslexia, Dystonia, Motor Dysfunction, Myoclonus, Neuritis, Neuromuscular Blockade, Nystagmus, Paralysis, Peroneal Nerve Palsy, Stupor, Visual Field Defect Eye disorders Diplopia, Eye Disorder* Cataract, Corneal Lesion, Dry Eye, Eye Haemorrhage, Eyelid Ptosis, Mydriasis, Optic Atrophy Ear and labyrinth disorders Ear Disorder Cardiac disorders Palpitations*, Tachycardia* Extrasystoles, Sinus Bradycardia, Tachycardia Paroxysmal Vascular disorders Vasodilatation* Varicose Vein Respiratory, thoracic and Dyspnoea* Cough, Rhinitis Seasonal Apnoea, Epistaxis, mediastinal disorders Hyperventilation, Laryngospasm, Lung Disorder, Choking Sensation System Organ Class (SOC) Very Common Common Uncommon (≥1/10) (≥1/100 to <1/10) (≥1/1,000 to <1/100) Gastrointestinal disorders Nausea* Anorectal Disorder, Colitis, Colonic Polyp, Constipation, Dental Caries, Enterocolitis, Eructation, Dyspepsia, Dysphagia, Faecal Oesophageal Ulcer, Periodontitis Incontinence, Vomiting* Rectal Haemorrhage, Salivary Gland Enlargement Hepatobiliary disorders Liver Function Test Abnormal Cholelithiasis, Hepatomegaly Skin and subcutaneous tissue Rash* Ecchymosis, Hyperhidrosis, Angioedema, Dermatitis Contact, disorders Pruritus, Skin Disorder*, Erythema Nodosum, Skin Nodule Urticaria Musculoskeletal and Arthralgia, Back Neck Pain Arthritis, Bursitis, Flank Pain, connective tissue disorders Pain* Muscle Atrophy, Osteoarthritis Renal and urinary disorders Micturition Urgency, Haematuria, Nephrolithiasis, Pollakiuria, Urinary Retention Urinary Tract Disorder, Urine Abnormality Pregnancy, puerperium and Abortion perinatal Conditions Reproductive system and Breast Engorgement, Erectile breast disorders Dysfunction, Pelvic Prolapse, Priapism, Prostatic Disorder, Smear Cervix Abnormal, Testicular Disorder, Vaginal Haemorrhage, Vulvovaginal Disorder General disorders and Asthenia, Chest Chills*, Face Oedema*, Cyst, Hangover, Hypothermia, administration site conditions Pain*, Injection Site Injection Site Atrophy#, Local Immediate Post-Injection Reaction, Reactions*§, Pain* Reaction*, Oedema Peripheral, Inflammation, Injection Site Oedema, Pyrexia Necrosis, Mucous Membrane Disorder Injury, poisoning and Post Vaccination Syndrome procedural complications * More than 2% (>2/100) higher incidence in the Copaxone treatment group than in the placebo group. Adverse reaction without the * symbol represents a difference of less than or equal to 2%. § The term ‘injection site reactions’ (various kinds) comprises all adverse events occurring at the injection site excluding injection site atrophy and injection site necrosis, which are presented separately within the table. # Includes terms which relate to localized lipoatrophy at the injection sites. In the fourth trial noted above, an open-label treatment phase followed the placebo- controlled period. No change in the known risk profile of Copaxone 20 mg/ml was observed during the open-label follow-up period of up to 5 years. Rare (≥1/10,000 to <1/1,000) reports of anaphylactoid reactions were collected from MS patients treated with Copaxone in uncontrolled clinical trials and from post- marketing experience with Copaxone. Copaxone 40 mg/ml (administered three times per week) The safety of Copaxone 40 mg/ml was assessed based on a double-blind, placebo- controlled clinical trial in RRMS patients with a total of 943 patients treated with Copaxone 40 mg/ml three times per week, and 461 patients treated with placebo for 12 months. In general, the kind of adverse drug reactions seen in patients treated with Copaxone 40 mg/ml administered three times per week were those already known and labelled for Copaxone 20 mg/ml administered daily. In particular, adverse injection site reactions (ISR) and immediate post-injection reactions (IPIR) were reported at lower frequency for Copaxone 40 mg/ml administered three times per week than for Copaxone 20 mg/ml administered daily (35.5 % vs. 70 % for ISRs and 7.8 % vs. 31 % for IPIRs, respectively). Injection site reactions were reported by 36% of the patients on Copaxone 40 mg/ml compared to 5% on placebo. Immediate post-injection reaction was reported by 8% of the patients on Copaxone 40 mg/ml compared to 2% on placebo. A few specific adverse reactions are noted: • Anaphylactic response was seen rarely (≥1/10,000, <1/1,000) in MS patients treated with Copaxone 20 mg/ml in uncontrolled clinical trials and from post-marketing experience. It was reported by 0.3% of the patients on Copaxone 40 mg/ml (Uncommon: 1/1,000 to < 1/100). • No injection site necrosis was reported. • Skin erythema and pain in extremity, not labelled for Copaxone 20 mg/ml, were reported each by 2.1% of the patients on Copaxone 40 mg/ml (Common: 1/100 to < 1/10). • Drug-induced liver injury and toxic hepatitis, also seen rarely in MS patients treated with Copaxone 20 mg/ml in post marketing surveillance, were each reported by one patient (0.1%) on Copaxone 40 mg/ml (Uncommon: 1/1,000 to < 1/100). Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול בחולים עם אבחנה וודאית של טרשת נפוצה (על פי הקריטריונים העדכניים על שם McDonald) עם מחלה פעילה או Clinically Isolated Syndrome (CIS), בהתאם לתנאי הרישום.הטיפול לא יינתן לחולים עם מחלה פרוגרסיבית ראשונית (PPMS) או פרוגרסיבית שניונית פעילה (SPMS) שאינם מטופלים בתרופות ייעודיות לטרשת נפוצה.ב. הטיפול יינתן כמונותרפיה.ג. התחלת הטיפול בתרופה תיעשה לפי מרשם של נוירו אימונולוג שעבר השתלמות עמיתים, או נוירולוג ילדים שעבר השתלמות עמיתים בטרשת נפוצה, או מומחה בנוירולוגיה העובד במרפאת טרשת נפוצה או מרפאה נוירואימונולוגית ייעודית.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| א. התרופה תינתן לטיפול בחולים עם אבחנה וודאית של טרשת נפוצה (על פי הקריטריונים העדכניים על שם McDonald) עם מחלה פעילה או Clinically Isolated Syndrome (CIS), בהתאם לתנאי הרישום. הטיפול לא יינתן לחולים עם מחלה פרוגרסיבית ראשונית (PPMS) או פרוגרסיבית שניונית פעילה (SPMS) שאינם מטופלים בתרופות ייעודיות לטרשת נפוצה. ב. הטיפול יינתן כמונותרפיה. ג. התחלת הטיפול בתרופה תיעשה לפי מרשם של נוירו אימונולוג שעבר השתלמות עמיתים, או נוירולוג ילדים שעבר השתלמות עמיתים בטרשת נפוצה, או מומחה בנוירולוגיה העובד במרפאת טרשת נפוצה או מרפאה נוירואימונולוגית ייעודית. | 03/02/2022 | נוירולוגיה | טרשת נפוצה, Multiple sclerosis | |
| התרופה האמורה תינתן לטיפול במקרים האלה: א. טרשת נפוצה, ובהתקיים כל התנאים האלה (התוויה כלולה בסל): (1) החולה מאובחן כסובל מטרשת נפוצה מסוג נסיגה נשנית (relapsing remitting) בלבד; (2) למחלה ניתנה אבחנה קלינית מוגדרת (clinically definite) או אבחנה הנתמכת בבדיקת מעבדה (laboratory supported definite); (3) החולה בעל כושר תנועה ואינו זקוק לתמיכה קבועה לצורכי ניידות (5.5EDSS | 03/01/2010 | נוירולוגיה | טרשת נפוצה, Multiple sclerosis | |
| 01/06/1997 | נוירולוגיה | טרשת נפוצה, Multiple sclerosis |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/06/1997
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
