Quest for the right Drug
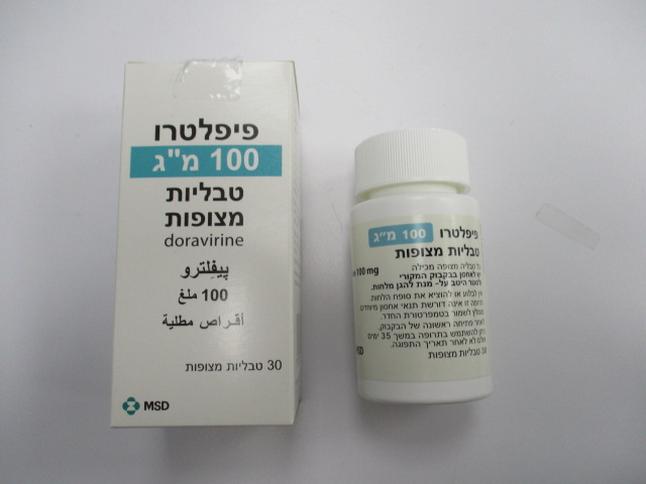
פיפלטרו 100 מ"ג טבליות מצופות PIFELTRO 100 MG FILM - COATED TABLETS (DORAVIRINE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antivirals for systemic use, ATC code: J05AG06 Mechanism of action Doravirine is a pyridinone non-nucleoside reverse transcriptase inhibitor of HIV-1 and inhibits HIV-1 replication by non-competitive inhibition of HIV-1 reverse transcriptase (RT). Doravirine does not inhibit the human cellular DNA polymerases α, ß, and mitochondrial DNA polymerase γ. Antiviral activity in cell culture Doravirine exhibited an EC50 value of 12.0±4.4 nM against wild-type laboratory strains of HIV-1 when tested in the presence of 100 % normal human serum using MT4-GFP reporter cells. Doravirine demonstrated antiviral activity against a broad panel of primary HIV-1 isolates (A, A1, AE, AG, B, BF, C, D, G, H) with EC50 values ranging from 1.2 nM to 10.0 nM. Antiviral activity in combination with other HIV antiviral medicinal products The antiviral activity of doravirine was not antagonistic when combined with the NNRTIs delavirdine, efavirenz, etravirine, nevirapine, or rilpivirine; the NRTIs abacavir, didanosine, emtricitabine, lamivudine, stavudine, tenofovir disoproxil, or zidovudine; the PIs darunavir or indinavir; the fusion inhibitor enfuvirtide; the CCR5 co-receptor antagonist maraviroc; or the integrase strand transfer inhibitor raltegravir. Resistance In cell culture Doravirine-resistant strains were selected in cell culture starting from wild-type HIV-1 of different origins and subtypes, as well as NNRTI-resistant HIV-1. Observed emergent amino acid substitutions in RT included: V106A, V106M, V106I, V108I, F227L, F227C, F227I, F227V, H221Y, M230I, L234I, P236L, and Y318F. The V106A, V106M, V108I, H221Y, F227C, M230I, P236L, and Y318F substitutions conferred 3.4-fold to 70-fold reductions in susceptibility to doravirine. Y318F in combination with V106A, V106M, V108I, or F227C conferred greater decreases in susceptibility to doravirine than Y318F alone, which conferred a 10-fold reduction in susceptibility to doravirine. Common NNRTI-resistant mutations (K103N, Y181C) were not selected in the in vitro study. V106A (yielding a fold change of around 19) appeared as an initial substitution in subtype B virus, and V106A or M in subtype A and C virus. Subsequently F227(L/C/V) or L234I emerged in addition to V106 substitutions (double mutants yielding a fold change of > 100). In clinical trials Treatment-naïve adult subjects The Phase 3 studies, DRIVE-FORWARD and DRIVE-AHEAD, included previously untreated patients (n = 747) where the following NNRTI substitutions were part of exclusion criteria: L100I, K101E, K101P, K103N, K103S, V106A, V106I, V106M, V108I, E138A, E138G, E138K, E138Q, E138R, V179L, Y181C, Y181I, Y181V, Y188C, Y188H, Y188L, G190A, G190S, H221Y, L234I, M230I, M230L, P225H, F227C, F227L, F227V. The following de novo resistance was seen in the resistance analysis subset (subjects with HIV-1 RNA greater than 400 copies per mL at virologic failure or at early study discontinuation and having resistance data). Table 3: Resistance development up to Week 96 in protocol defined virologic failure population + early discontinuation population DRIVE-FORWARD DRIVE-AHEAD DOR + DRV + r + DOR/TDF/3T EFV/TDF/FTC NRTIs* NRTIs* C (364) (383) (383) (364) Successful genotype, n 15 18 32 33 Genotypic resistance to DOR or control (DRV or 2 (DOR) 0 (DRV) 8 (DOR) 14 (EFV) EFV) NRTI backbone 2** 0 6 5 M184I/V only 2 0 4 4 K65R only 0 0 1 0 K65R + M184I/V 0 0 1 1 *NRTIs in DOR arm: FTC/TDF (333) or ABC/3TC (50); NRTIs in DRV+r arm: FTC/TDF (335) or ABC/3TC (48) **Subjects received FTC/TDF ABC=abacavir; FTC=emtricitabine; DRV=darunavir; r=ritonavir Emergent doravirine associated resistance substitutions in RT included one or more of the following: A98G, V106I, V106A, V106M/T, Y188L, H221Y, P225H, F227C, F227C/R, and Y318Y/F. Virologically suppressed adult subjects The DRIVE-SHIFT study included virologically suppressed patients (N=670) with no history of treatment failure (see section, Clinical experience). A documented absence of genotypic resistance (prior to starting first therapy) to doravirine, lamivudine, and tenofovir was part of the inclusion criteria for patients who switched from a PI- or INI-based regimen. Exclusionary NNRTI substitutions were those listed above (DRIVE-FORWARD and DRIVE-AHEAD), with the exception of substitutions RT K103N, G190A and Y181C (accepted in DRIVE-SHIFT). Documentation of pre- treatment resistance genotyping was not required for patients who switched from a NNRTI-based regimen. In the DRIVE-SHIFT clinical trial, no subjects developed genotypic or phenotypic resistance to DOR, 3TC, or TDF during the initial 48 weeks (immediate switch, N=447) or 24 weeks (delayed switch, N=209) of treatment with DOR/3TC/TDF. One subject developed RT M184M/I mutation and phenotypic resistance to 3TC and FTC during treatment with their baseline regimen. None of the 24 subjects (11 in the immediate switch group, 13 in the delayed switch group) with baseline NNRTI mutations (RT K103N, G190A, or Y181C) experienced virologic failure through Week 48, or at time of discontinuation. Cross-resistance Doravirine has been evaluated in a limited number of patients with NNRTI resistance (K103N n=7, G190A n=1); all patients were suppressed to < 40 copies/mL at Week 48. A breakpoint for a reduction in susceptibility, yielded by various NNRTI substitutions, that is associated with a reduction in clinical efficacy has not been established. Laboratory strains of HIV-1 harbouring the common NNRTI-associated mutations K103N, Y181C, or K103N/Y181C substitutions in RT exhibit less than a 3-fold decrease in susceptibility to doravirine compared to wild-type virus when evaluated in the presence of 100 % normal human serum. In in vitro studies, doravirine was able to suppress the following NNRTI-associated substitutions; K103N, Y181C, and G190A under clinically relevant concentrations. A panel of 96 diverse clinical isolates containing NNRTI-associated mutations was evaluated for susceptibility to doravirine in the presence of 10 % foetal bovine serum. Clinical isolates containing the Y188L substitution or V106 substitutions in combination with A98G, H221Y, P225H, F227C or Y318F showed a greater than 100-fold reduced susceptibility to doravirine. Other established NNRTI substitutions yielded a fold change of 5-10 (G190S (5.7), K103N/P225H (7.9), V108I/Y181C (6.9), Y181V (5.1)). The clinical relevance of a 5-10 fold reduction in susceptibility is unknown. Treatment emergent doravirine resistance associated substitutions may confer cross-resistance to efavirenz, rilpivirine, nevirapine, and etravirine. Of the 8 subjects who developed high level doravirine resistance in the pivotal studies, 6 had phenotypic resistance to EFV and nevirapine, 3 to rilpivirine, and 3 had partial resistance to etravirine based on the Monogram Phenosense assay. Clinical experience Treatment-naïve adult subjects The efficacy of doravirine is based on the analyses of 96-week data from two randomised, multicentre, double-blind, active controlled Phase 3 trials, (DRIVE-FORWARD and DRIVE-AHEAD) in antiretroviral treatment-naïve, HIV-1 infected subjects (n = 1494). Refer to Resistance section for NNRTI substitutions that were part of exclusion criteria. In DRIVE-FORWARD, 766 subjects were randomised and received at least 1 dose of either doravirine 100 mg or darunavir + ritonavir 800+100 mg once daily, each in combination with emtricitabine/tenofovir disoproxil (FTC/TDF) or abacavir/lamivudine (ABC/3TC) selected by the investigator. At baseline, the median age of subjects was 33 years (range 18 to 69 years), 86 % had CD4+ T cell count greater than 200 cells per mm3, 84 % were male, 27 % were non-white, 4 % had hepatitis B and/or C virus co-infection, 10 % had a history of AIDS, 20 % had HIV-1 RNA greater than 100,000 copies per mL, 13 % received ABC/3TC and 87 % received FTC/TDF; these characteristics were similar between treatment groups. In DRIVE-AHEAD, 728 subjects were randomised and received at least 1 dose of either doravirine/lamivudine/tenofovir disoproxil 100/300/245 mg (DOR/3TC/TDF) or efavirenz/emtricitabine/tenofovir disoproxil (EFV/FTC/TDF) once daily. At baseline, the median age of subjects was 31 years (range 18-70 years), 85 % were male, 52 % were non-white, 3% had hepatitis B or C co-infection, 14 % had a history of AIDS, 21 % had HIV-1 RNA > 100,000 copies per mL, and 12 % had CD4+ T cell count < 200 cells per mm3; these characteristics were similar between treatment groups. Week 48 and 96 outcomes for DRIVE-FORWARD and DRIVE-AHEAD are provided in Table 4. The doravirine-based regimens demonstrated consistent efficacy across demographic and baseline prognostic factors. Table 4: Efficacy response (< 40 copies/mL, Snapshot approach) in the pivotal studies DRIVE-FORWARD DRIVE-AHEAD DOR + 2 NRTIs DRV + r + 2 DOR/3TC/TDF EFV/FTC/TDF (383) NRTIs (383) (364) (364) Week 48 83 % 79 % 84 % 80 % Difference (95 % CI) 4.2 % (-1.4%, 9.7 %) 4.1 % (-1.5 %, 9.7 %) Week 96* 72 % (N=379) 64 % (N=376) 76 % (N=364) 73 % (N=364) Difference (95 % CI) 7.6 % (1.0 %, 14.2 %) 3.3 % (-3.1 %, 9.6 %) Week 48 outcome (< 40 copies/mL) by baseline factors HIV-1 RNA copies/mL ≤ 100 000 256/285 (90 %) 248/282 (88 %) 251/277 (91 %) 234/258 (91 %) > 100 000 63/79 (80 %) 54/72 (75 %) 54/69 (78 %) 56/73 (77 %) CD4 count, cells/µL ≤ 200 34/41 (83 %) 43/61 (70 %) 27/42 (64 %) 35/43 (81 %) > 200 285/323 (88 %) 260/294 (88 %) 278/304 (91 %) 255/288 (89 %) NRTI background therapy TDF/FTC 276/316 (87 %) 267/312 (86 %) NA ABC/3TC 43/48 (90 %) 36/43 (84 %) Viral subtype B 222/254 (87 %) 219/255 (86 %) 194/222 (87 %) 199/226 (88 %) non-B 97/110 (88 %) 84/100 (84 %) 109/122 (89 %) 91/105 (87 %) Mean CD4 change from baseline Week 48 193 186 198 188 Week 96 224 207 238 223 *For Week 96, certain subjects with missing HIV-1 RNA were excluded from the analysis. P007 was a Phase 2b trial in antiretroviral treatment-naïve HIV-1 infected adult subjects (n = 340). In Part I, subjects were randomised to receive one of 4 doses of doravirine or EFV, each in combination with FTC/TDF. After Week 24, all subjects randomised to receive doravirine were switched to (or maintained on) doravirine 100 mg. Additional subjects were randomised in Part II to receive either doravirine 100 mg or EFV, each in combination with FTC/TDF. In both parts of the trial, doravirine and EFV were administered as blinded-therapy and FTC/TDF was administered open-label. Table 5: Efficacy response at Week 24 (Snapshot approach) Doravirine Doravirine Doravirine Doravirine Efavirenz 25 mg 50 mg 100 mg 200 mg 600 mg (N=40) (N=43) (N=42) (N=41) (N=42) n (%) n (%) n (%) n (%) n (%) HIV-1 RNA < 40 copies/mL 32 (80) 32 (74) 30 (71) 33 (80) 27 (64) Treatment differences † 16 (-4, 34) 10 (-10, 6.6 (-13, 16 (-3, 34) (95 % CI) †† 29) 26) Mean CD4 change from 154 113 134 141 121 baseline (cells/mm3) ** †A positive value favours doravirine over efavirenz. ††The 95 % CIs were calculated using Miettinen and Nurminen’s method with weights proportional to the size of each stratum (screening HBV-1 RNA > 100,000 copies/mL or ≤ 100,000 copies/mL. **Approach to handle missing data: Observed Failure (OF) approach. Baseline CD4 cell count was carried forward for subjects who discontinued assigned therapy due to lack of efficacy. Note: Both doravirine and efavirenz were administered with emtricitabine/tenofovir disoproxil (FTC/TDF). Virologically suppressed adult subjects The efficacy of switching from a baseline regimen consisting of two nucleoside reverse transcriptase inhibitors in combination with a ritonavir- or cobicistat-boosted PI, or cobicistat-boosted elvitegravir, or an NNRTI to DOR/3TC/TDF was evaluated in a randomised, open-label trial (DRIVE-SHIFT), in virologically suppressed HIV-1 infected adults. Subjects must have been virologically suppressed (HIV-1 RNA < 40 copies/mL) on their baseline regimen for at least 6 months prior to trial entry, with no history of virologic failure, and a documented absence of RT substitutions conferring resistance to doravirine, lamivudine and tenofovir (see section Resistance). Subjects were randomised to either switch to DOR/3TC/TDF at baseline [N = 447, Immediate Switch Group (ISG)], or stay on their baseline regimen until Week 24, at which point they switched to DOR/3TC/TDF [N = 223, Delayed Switch Group (DSG)]. At baseline, the median age of subjects was 43 years, 16 % were female, and 24 % were non-white. In the DRIVE-SHIFT trial, an immediate switch to DOR/3TC/TDF was demonstrated to be non- inferior at Week 48 compared to continuation of the baseline regimen at Week 24 as assessed by the proportion of subjects with HIV-1 RNA < 40 copies/mL. Treatment results are shown in Table 6. Consistent results were seen for the comparison at study Week 24 in each treatment group. Table 6: Efficacy response (Snapshot approach) in the DRIVE-SHIFT study DOR/3TC/TDF Baseline Regimen Once Daily ISG DSG Week 48 Week 24 Outcome N=447 N=223 HIV-1 RNA < 40 copies/mL 90 % 93 % ISG-DSG, Difference (95 % CI)* -3.6 % (-8.0 %, 0.9 %) Proportion (%) of Subjects With HIV-1 RNA < 40 copies/mL by Baseline Regimen Received Ritonavir- or Cobicistat-boosted PI 280/316 (89 %) 145/156 (93 %) Cobicistat-boosted elvitegravir 23/25 (92 %) 11/12 (92 %) NNRTI 98/106 (92 %) 52/55 (95 %) Proportion (%) of Subjects With HIV-1 RNA < 40 copies/mL by Baseline CD4+ T cell Count (cells/mm3) < 200 cells/mm3 10/13 (77 %) 3/4 (75 %) ≥ 200 cells/mm3 384/426 (90 %) 202/216 (94 %) HIV-1 RNA ≥ 40 copies/mL† 3% 4% No Virologic Data Within the Time Window 8% 3% Discontinued study due to AE or Death‡ 3% 0 Discontinued study for Other Reasons § 4% 3% On study but missing data in window 0 0 *The 95 % CI for the treatment difference was calculated using stratum-adjusted Mantel-Haenszel method. †Includes subjects who discontinued study treatment or study before Week 48 for ISG or before Week 24 for DSG for lack or loss of efficacy and subjects with HIV-1 RNA ≥ 40 copies/mL in the Week 48 window for ISG and in the Week 24 window for DSG. ‡Includessubjects who discontinued because of adverse event (AE) or death if this resulted in no virologic data on treatment during the specified window. §Otherreasons include: lost to follow-up, non-compliance with study treatment, physician decision, protocol deviation, withdrawal by subject. Baseline regimen = ritonavir or cobicistat-boosted PI (specifically atazanavir, darunavir, or lopinavir), or cobicistat-boosted elvitegravir, or NNRTI (specifically efavirenz, nevirapine, or rilpivirine), each administered with two NRTIs. Discontinuation due to adverse events In a pooled analysis combining data from two treatment-naïve trials (P007 and DRIVE-AHEAD), a lower proportion of subjects who discontinued due to an adverse event by Week 48 was seen for the combined doravirine (100 mg) treatment groups (2.8 %) compared with the combined EFV treatment group (6.1 %) (treatment difference -3.4 %, p-value 0.012). Paediatric population Pifeltro is not indicated for children and adolescents below 18 years of age. .
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption The pharmacokinetics of doravirine were studied in healthy subjects and HIV-1 infected subjects. Doravirine pharmacokinetics are similar in healthy subjects and HIV-1-infected subjects. Steady state was generally achieved by Day 2 of once daily dosing, with accumulation ratios of 1.2 to 1.4 for AUC0-24, Cmax, and C24. Doravirine steady state pharmacokinetics following administration of 100 mg once daily to HIV-1 infected subjects, based on a population pharmacokinetics analysis, are provided below. Parameter AUC0-24 Cmax C24 GM (% CV) μg•h/mL μg/mL μg/mL Doravirine 100 mg 16.1 (29) 0.962 (19) 0.396 (63) once daily GM: Geometric mean, % CV: Geometric coefficient of variation Following oral dosing, peak plasma concentrations are achieved 2 hours after dosing. Doravirine has an estimated absolute bioavailability of approximately 64 % for the 100 mg tablet. Effect of food on oral absorption The administration of a single doravirine tablet with a high-fat meal to healthy subjects resulted in a 16 % and 36 % increase in doravirine AUC and C24, respectively, while Cmax was not significantly affected. Distribution Based on administration of an intravenous microdose, the volume of distribution of doravirine is 60.5 L. Doravirine is approximately 76 % bound to plasma proteins. Biotransformation Based on in vitro data, doravirine is primarily metabolised by CYP3A. Elimination Doravirine has a terminal half-life (t1/2) of approximately 15 hours. Doravirine is primarily eliminated via oxidative metabolism mediated by CYP3A4. Biliary excretion of unchanged medicinal product may contribute to the elimination of doravirine, but this elimination route is not expected to be significant. Excretion of unchanged medicinal product via urinary excretion is minor. Renal impairment Renal excretion of doravirine is minor. In a study comparing 8 subjects with severe renal impairment to 8 subjects without renal impairment, the single dose exposure of doravirine was 31 % higher in subjects with severe renal impairment. In a population pharmacokinetic analysis, which included subjects with CrCl between 17 and 317 mL/min, renal function did not have a clinically relevant effect on doravirine pharmacokinetics. No dose adjustment is required in patients with mild, moderate or severe renal impairment. Doravirine has not been studied in patients with end-stage renal disease or in patients undergoing dialysis (see section 4.2). Hepatic impairment Doravirine is primarily metabolised and eliminated by the liver. There was no clinically relevant difference in the pharmacokinetics of doravirine in a study comparing 8 subjects with moderate hepatic impairment (classified as Child-Pugh score B primarily due to increased encephalopathy and ascites scores) to 8 subjects without hepatic impairment. No dose adjustment is required in patients with mild or moderate hepatic impairment. Doravirine has not been studied in subjects with severe hepatic impairment (Child-Pugh score C) (see section 4.2). Elderly Although a limited number of subjects aged 65 years and over has been included (n=36), no clinically relevant differences in the pharmacokinetics of doravirine have been identified in subjects at least 65 years of age compared to subjects less than 65 years of age in a Phase 1 trial or in a population pharmacokinetic analysis. No dose adjustment is required. Gender No clinically relevant pharmacokinetic differences have been identified between men and women for doravirine. Race No clinically relevant racial differences in the pharmacokinetics of doravirine have been identified based on a population pharmacokinetic analysis of doravirine in healthy and HIV-1 infected subjects.

פרטי מסגרת הכללה בסל
א. התרופה האמורה תינתן לטיפול בנשאי HIV.ב. מתן התרופה ייעשה לפי מרשם של מנהל מרפאה לטיפול באיידס, במוסד רפואי שהמנהל הכיר בו כמרכז AIDS.ג. משטר הטיפול בתרופה יהיה כפוף להנחיות המנהל, כפי שיעודכנו מזמן לזמן על פי המידע העדכני בתחום הטיפול במחלה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| טיפול בנשאי HIV | 30/01/2020 | מחלות זיהומיות | HIV |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
30/01/2020
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
רישום
164 62 36060 00
מחיר
0 ₪
מידע נוסף
עלון מידע לצרכן
22.08.22 - עלון לצרכן אנגלית 22.08.22 - עלון לצרכן עברית 14.11.22 - עלון לצרכן ערבית 28.02.23 - עלון לצרכן 28.02.23 - עלון לצרכן 28.02.23 - עלון לצרכן עברית 16.03.23 - עלון לצרכן ערבית 10.10.23 - עלון לצרכן אנגלית 10.10.23 - עלון לצרכן עברית 30.10.23 - עלון לצרכן ערבית 17.10.24 - עלון לצרכן אנגלית 30.10.24 - עלון לצרכן עברית 22.08.22 - החמרה לעלון 28.02.23 - החמרה לעלון 09.10.23 - החמרה לעלון 17.10.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
פיפלטרו 100 מ"ג טבליות מצופות