Quest for the right Drug
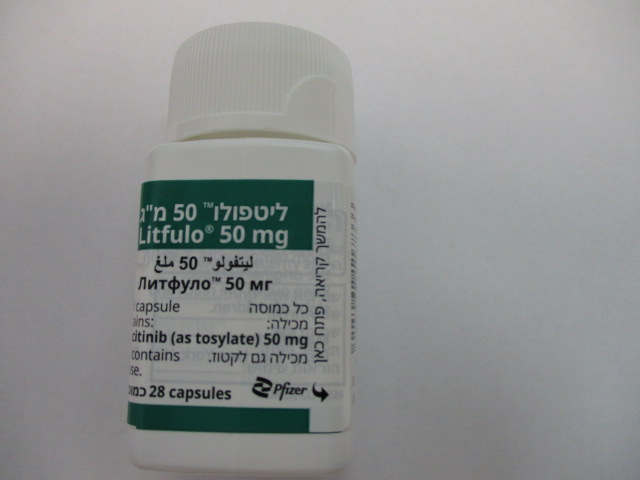
ליטפולו 50 מ"ג LITFULO 50 MG (RITLECITINIB, RITLECITINIB AS TOSYLATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
קפסולות : CAPSULES
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Serious infections Serious infections have been reported in patients receiving ritlecitinib. The most frequent serious infections have been appendicitis, COVID-19 infection (including pneumonia), and sepsis. Treatment with ritlecitinib must not be initiated in patients with an active, serious infection (see section 4.3). The risks and benefits of treatment should be considered in patients: • with chronic or recurrent infection • who have been exposed to tuberculosis (TB) • with a history of serious or an opportunistic infection • who have resided or traveled in areas of endemic TB or mycoses, or • with underlying conditions that may predispose them to infection Patients should be closely monitored for the development of signs and symptoms of infection during and after treatment with ritlecitinib. Treatment should be interrupted if a patient develops a serious or opportunistic infection. A patient who develops a new infection during treatment with ritlecitinib should undergo prompt and complete diagnostic testing appropriate for an immunocompromised patient, appropriate antimicrobial therapy should be initiated, and the patient should be closely monitored. If interrupted, ritlecitinib may be resumed once the infection is controlled. As there is a higher incidence of infections in elderly and in the diabetic population in general, caution should be exercised when treating the elderly and patients with diabetes, and particular attention paid with respect to occurrence of infections. Tuberculosis Patients should be screened for TB before starting therapy with ritlecitinib. Ritlecitinib must not be given to patients with active TB (see section 4.3). Anti-TB therapy should be started prior to initiating therapy with ritlecitinib in patients with a new diagnosis of latent TB or previously untreated latent TB. In patients with a negative latent TB test, anti-TB therapy should still be considered before initiating treatment with ritlecitinib in those at high risk and screening for patients at high risk for TB during treatment with ritlecitinib should be considered. Viral reactivation Viral reactivations, including cases of herpes virus reactivation (e.g., herpes zoster), have been reported (see section 4.8). If a patient develops herpes zoster, temporary interruption of treatment may be considered until the episode resolves. Screening for viral hepatitis should be performed in accordance with clinical guidelines before starting therapy with ritlecitinib. Patients with evidence of hepatitis B or C infection were excluded from studies with ritlecitinib. Monitoring for reactivation of viral hepatitis according to clinical guidelines is recommended during ritlecitinib treatment. If there is evidence of reactivation, a liver specialist should be consulted. Malignancy (including non-melanoma skin cancer) Malignancies, including non-melanoma skin cancer (NMSC) have been reported in patients receiving ritlecitinib. It is not known whether selective JAK3 inhibition may be associated with adverse reactions of Janus Kinase (JAK) inhibition predominantly involving JAK1 and JAK2. In a large randomised active-controlled study of tofacitinib (another JAK inhibitor) in rheumatoid arthritis (RA) patients 50 years and older with at least one additional cardiovascular risk factor, a higher rate of malignancies, particularly lung cancer, lymphoma and NMSC, was observed with tofacitinib compared to tumour necrosis factor (TNF) inhibitors. In this study, current or past smokers had an additional increased risk of overall malignancies. Limited clinical data are available to assess the potential relationship of exposure to ritlecitinib and the development of malignancies. Long-term safety evaluations are ongoing. The risks and benefits of ritlecitinib treatment should be considered prior to initiating or continuing therapy in patients with a known malignancy other than a successfully treated NMSC or cervical cancer. Periodic skin examination is recommended for patients who are at increased risk of skin cancer. Major adverse cardiovascular events (MACE), deep venous thrombosis (DVT) and pulmonary embolism (PE) Events of venous and arterial thromboembolism, including MACE, have been reported in patients receiving ritlecitinib. It is not known whether selective JAK3 inhibition may be associated with adverse reactions of JAK inhibition predominantly involving JAK1 and JAK2. In a large randomised active-controlled study of tofacitinib (another JAK inhibitor) in RA patients 50 years and older with at least one additional cardiovascular risk factor, a higher rate of MACE, defined as cardiovascular death, non-fatal myocardial infarction and non-fatal stroke, and a dose -dependent higher rate of venous thromboembolism including DVT and PE were observed with tofacitinib compared to TNF inhibitors. Patients who are current or past smokers are at additional increased risk for major adverse cardiovascular events (MACE). Long-term safety evaluations for ritlecitinib are ongoing. Ritlecitinib should be used with caution in patients with known risk factors for thromboembolism. In patients with a suspected thromboembolic event, discontinuation of ritlecitinib and prompt re-evaluation is recommended. The risks and benefits of ritlecitinib treatment should be considered prior to initiating therapy in patients. Neurological events Ritlecitinib-related axonal dystrophy has been observed in chronic Beagle dog toxicity studies (see section 5.3). Treatment with ritlecitinib should be discontinued in case unexplained neurological symptoms occur. Audiological events Routine audiological testing (including pure tone audiometry, speech audiometry, and immittance audiometry) was implemented in the trials at specified time points to assess for potential changes in hearing status. In the placebo-controlled trials, for up to 24 weeks, sensorineural hearing loss occurred in less than 1% of participants in the ritlecitinib group (1 case) and the rate in placebo was 0. Across clinical trials, including the long-term trial, events meeting criteria for sensorineural hearing loss were reported in 14 subjects (0.71 per 100 subject-years) treated with Ritlecitinib 50 mg or higher. The majority of audiological events were mild in severity, did not demonstrate a dose response, were considered unrelated to ritlecitinib, and resolved without change to Ritlecitinib treatment. There were no reports of central hearing disorder. There were no events meeting criteria for sensorineural hearing loss reported in adolescents. Haematologic abnormalities Treatment with ritlecitinib was associated with decreases in lymphocytes and platelets (see section 4.8). Prior to initiating treatment with ritlecitinib, ALC and platelet counts should be performed. Treatment with ritlecitinib should not be initiated in patients with an ALC < 0.5 × 103/mm3 or a platelet count < 100 × 103/mm3. After initiating treatment with ritlecitinib, treatment interruption or discontinuation are recommended based on ALC and platelet count abnormalities (see section 4.2). ALC and platelet counts are recommended at 4 weeks after initiation of therapy with ritlecitinib, and thereafter according to routine patient management. Vaccinations No data are available on the response to vaccination in patients receiving ritlecitinib. Use of live attenuated vaccines should be avoided during or immediately prior to ritlecitinib treatment. Prior to initiating ritlecitinib, it is recommended that patients are brought up to date with all immunisations, including prophylactic herpes zoster vaccinations, in agreement with current immunisation guidelines. Elderly There are limited data in patients ≥ 65 years of age. Age appeared to be a risk factor for lower ALC in patients ≥ 65 years of age. Excipients with known effect Lactose Patients with rare hereditary problems of galactose intolerance, total lactase deficiency or glucose-galactose malabsorption should not take this medicinal product.
Effects on Driving
4.7 Effects on ability to drive and use machines Litfulo has no or negligible influence on the ability to drive and use machines.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
